甲状腺球蛋白检测对甲状腺癌颈部转移淋巴结的鉴别诊断价值
2015-03-21赫铁军
赫铁军,杨 柏,张 洋
1辽宁医学院附属第三医院 超声科,辽宁锦州 121000;2辽宁医学院附属第一医院,辽宁锦州 121000;3锦州市凌河区医院,辽宁锦州 121000
甲状腺球蛋白检测对甲状腺癌颈部转移淋巴结的鉴别诊断价值
赫铁军1,杨 柏2,张 洋3
1辽宁医学院附属第三医院 超声科,辽宁锦州 121000;2辽宁医学院附属第一医院,辽宁锦州 121000;3锦州市凌河区医院,辽宁锦州 121000
目的探讨甲状腺球蛋白检测(FNA-Tg)对甲状腺癌颈部转移淋巴结的鉴别诊断价值。方法所有病例选自2010年7月- 2014年3月因甲状腺结节来辽宁医学院附属第三医院就诊患者,超声发现104例可疑甲状腺癌患者伴有184个颈部可疑转移淋巴结,行超声引导细针穿刺抽吸细胞学检查(fine-needle aspiration cytology,FNAC),同时获得穿刺冲洗液送检甲状腺球蛋白检测。以手术病理为参考,评价FNAC和FNA-Tg对甲状腺癌颈部转移淋巴结的诊断准确性。结果FNAC和FNA-Tg对甲状腺癌颈部转移淋巴结的诊断敏感性、特异性和准确性分别为74.0%、100%、89.1%和92.2%、100%、96.7%;FNAC与手术病理诊断差异有统计学意义(P=0.03);FNA-Tg与手术病理诊断差异无统计学意义(P=0.23)。结论FNA-Tg作为一种安全、简便、可靠、准确的辅助检查手段,可提高FNAC对甲状腺癌颈部转移淋巴结的诊断准确率。
超声;穿刺活检;甲状腺癌;颈部淋巴结
乳头状癌是最常见的一种甲状腺癌,约占所有甲状腺癌的80%,其颈部淋巴结转移率为4.1% ~42.6%[1-2]。颈部淋巴结转移灶的出现,决定着患者治疗策略的选择,并严重影响患者的治疗效果及预后,因此对甲状腺乳头状癌颈部淋巴结转移灶的准确诊断尤为重要[3-5]。目前,对颈部淋巴结的检查常首选超声,但其鉴别良恶性能力尚显不足。因此超声引导下细针穿刺活检细胞学检查(fine needle aspiration cytology,FNAC)备受推崇[6-9]。然而,据报道FNAC因取材量及病理诊断医师经验等限制,常伴有20% ~ 25%不确定性或假阴性诊断[10]。近年来,国外多有报道颈部淋巴结细针穿刺活检水洗液甲状腺球蛋白(thyroglobulin,Tg)检查(即FNA-Tg),可提高对甲状腺乳头状癌颈部转移淋巴结的鉴别诊断能力[11-16]。因此,本研究基于多年甲状腺结节及颈部淋巴结FNAC基础上,探讨FNA-Tg对甲状腺癌颈部转移淋巴结的鉴别诊断价值。
资料和方法
1 病例资料 所有病例选自2010年7月- 2014年3月因甲状腺结节来辽宁医学院附属第三医院就诊患者,经超声检查初诊为可疑甲状腺癌患者384例,其中124例发现颈部可疑病变淋巴结,为进一步明确诊断,拟行颈部可疑病变淋巴结FNAC检查及FNA-Tg检测。根据病情需要,最终104例患者行甲状腺及颈部淋巴结手术切除治疗,并入选本研究,其中男26例、女78例,年龄(48.5±16.0)岁。
2 超声检查 采用GE logiq E9配备ML6-15MHz探头进行颈部淋巴结进行全面扫查。观察可疑淋巴结的颈部淋巴结转移灶大小、数目、形态、回声、部位、内部钙化、声晕、多普勒血流丰富程度等常规超声特征。根据超声特征选择可疑转移淋巴结行FNAC检查。可疑转移淋巴结选择标准:内部回声增高;部分呈囊性变;伴有微钙化;周边环绕血供丰富;淋巴结门结构消失;皮髓质界限不清;趋于类圆形;短径>5 mm;最小径>6 mm。
3 超声引导下FNAC及FNA-Tg检测 所有患者经术前告知并签署知情同意书,完善术前血常规、凝血指标等相关检查,由1名经验丰富的超声专业主治医师行超声引导下FNAC,患者卧于检查床,调整患者体位,使病灶处于最便于行超声引导穿刺的位置,根据目标淋巴结超声检查,选择安全、较近的穿刺路径,避开颈部血管、气管、神经等重要结构。选择细针穿刺(穿刺针为21 ~ 25 G针,连接5 ml注射器),穿刺针尖进入目标病灶内部后回抽注射器产生适当负压,反复多点抽吸>5次,可见少量含血穿刺物吸入注射器后退针,然后取出穿刺物涂片、无水乙醇固定、HE染色,所有穿刺病灶位置与对应标本均明确标记,一一对应后,送病理科做细胞学检查。然后将穿刺针及注射器用0.5 ~ 1.0 ml 0.9%氯化钠注射液冲洗,制成水洗液,送Tg水平检测,Tg检测采用电化学发光法。以100 ng/ml作为FNA-Tg诊断颈部淋巴结是否为转移淋巴结的截断值,FNA-Tg>100 ng/ml为转移性,FNA-Tg<100 ng/ml为良性[17]。
4 手术治疗及病理诊断 根据病情需要,部分病例行不同术式的甲状腺手术切除及相应的颈部淋巴结清扫术,手术标本送病理科检查。
5 统计学分析 采用SPSS16.0统计学软件进行统计分析。计量资料采用-x±s表示,两组间比较采用χ2检验,P<0.05为差异有统计学意义。以手术病理诊断作为诊断金标准,比较FNAC和FNATg诊断敏感性、特异性、阳性预测值、阴性预测值及诊断准确率。
结 果
1 颈部淋巴结超声回声特征 184个颈部可疑淋巴结经高频超声检查,其中长径(19.3±10.6) mm,短径(11.1±8.2) mm,其超声特征见表1。
2 颈部淋巴结超声引导下FNAC 104例入选病例经高频超声检查后,共184个颈部可疑淋巴结行超声引导下FNAC(图1)及FNA-Tg检查,FNAC细胞样本行HE染色细胞学检查(图2)。

图 1 超声引导下颈部可疑淋巴结(红色箭头)FNAC,淋巴结内部可见点状微钙化,并可见穿刺针(黄色箭头)准确穿刺入淋巴结图 2 颈部淋巴结FNAC穿刺细胞标本经HE染色后,可见核大深染的甲状腺乳头状癌细胞Fig. 1 Ultrasound guided fine needle (yellow arrow) aspiration cytology (FNAC) for suspicious cervical lymph node (red arrow) with microcalcif i cationFig. 2 FNAC of cervical lymph node demonstrated papillary thyroid cancer metastasis after hematoxylin eosin staining
3 颈部淋巴结FNAC、FNA-Tg和手术病理诊断对比结果 FNAC诊断良性淋巴结127例(69%),转移性淋巴结57例(31%);根据前述诊断标准,FNATg诊断良性淋巴结113例(61.4%),FNA-Tg检测范围为(0.2 ~ 29.2) ng/ml,(7.4±5.9) ng/ml;FNA-Tg诊断转移淋巴结71例(38.6%),FNA-Tg检测范围为(14.4 ~ 4 976.4) ng/ml,(1 680.7±1 023.9) ng/ml;手术病理诊断良性淋巴结107例(58.2%),转移性淋巴结77例(41.8%)。颈部淋巴结FNAC、FNATg及手术病理对照结果见表2。通过分析比较,FNAC在甲状腺癌颈部淋巴结鉴别诊断方面与手术病理诊断差异有统计学意义(P=0.03);而FNAC与FNA-Tg之间及FNA-Tg与手术病理诊断之间差异均无统计学意义(P=0.23)。以手术病理诊断作为参考,FNAC及FNA-Tg对甲状腺癌颈部转移淋巴结鉴别诊断的敏感性、特异性、阳性预测值、阴性预测值及准确率(表3)。由表2和表3可见,虽然FNAC与FNA-Tg差异无统计学意义,但FNA-Tg对颈部转移淋巴结的诊断敏感性由74.0%提高到92.2%,诊断准确性由89.1%提高到96.7%。
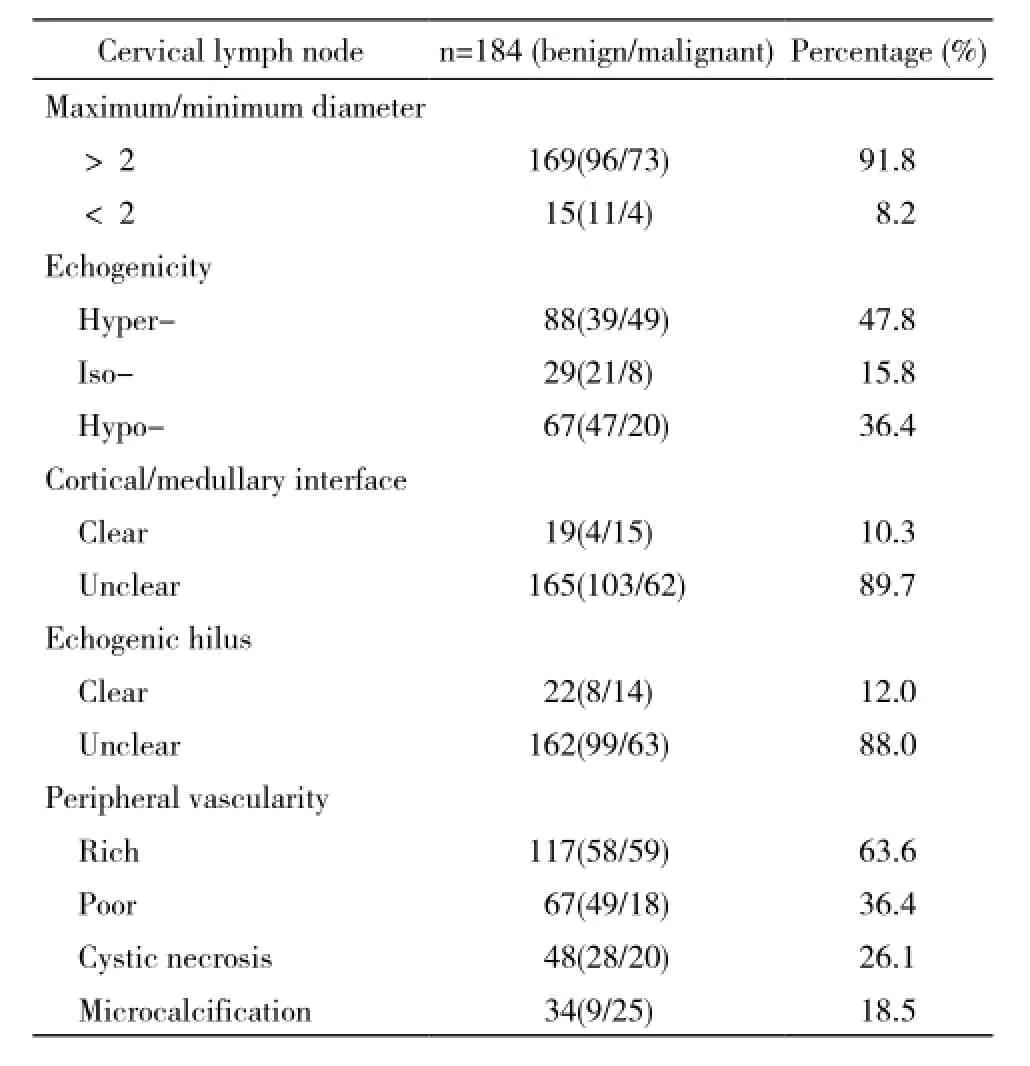
表1 颈部淋巴结超声特征Tab. 1 Sonographic features of cervical lymph nodes
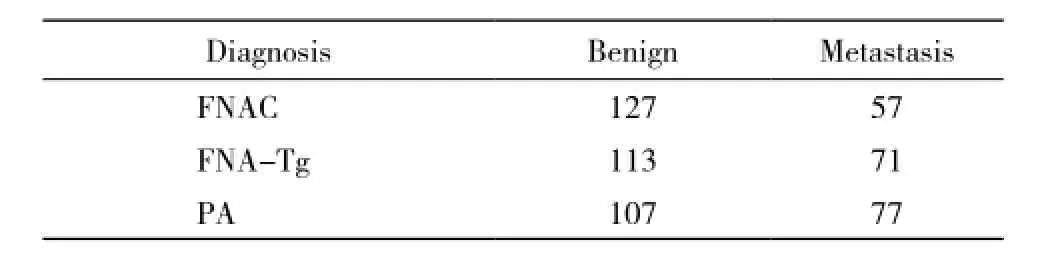
表2 颈部可疑淋巴结FNAC、FNA-Tg及手术病理诊断(PA)结果对照表Tab. 2 Diagnostic results of FNAC, FNA-Tg and surgical pathology for suspicious cervical lymph nodes (n)
Data represents the number of cervical lymph nodes. FNAC vs PA: χ2=4.69, P=0.03; FNA-Tg vs PA:χ2=1.44, P=0.23; FNAC vs FNA-Tg: χ2=2.35, P=0.13
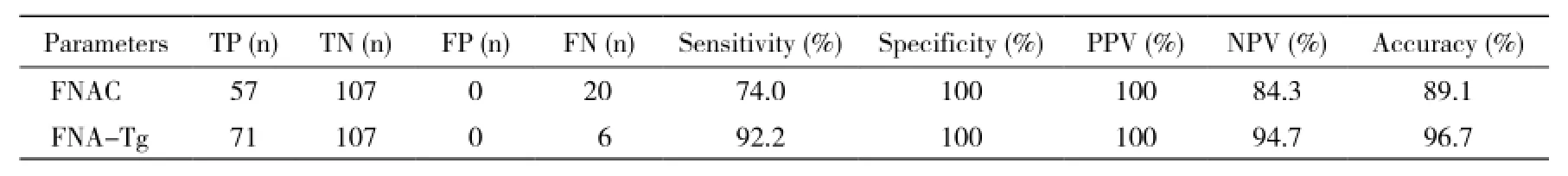
表3 FNAC及FNA-Tg对颈部转移淋巴结鉴别诊断结果Tab. 3 Comparison of FNAC and FNA-Tg for differential diagnosis of cervical lymph node
TP: true positive; TN: true negative; FP: false positive; FN: false negative; PPV: positive predictive value; NPV: negative predictive value
讨 论
Tg是由甲状腺上皮细胞合成的一种碘化糖蛋白,是碘在甲状腺的储存形式。在正常甲状腺组织和甲状腺上皮细胞源性癌组织中Tg含量较高,但在正常淋巴结组织中含量极低,等同于血清Tg水平。因此可采用穿刺活检样本水洗液(FNA-Tg水平)检测对甲状腺癌颈部转移淋巴结进行鉴别诊断。该技术1992年由Pacini等[18]首先报道,在国外已成为甲状腺癌颈部转移淋巴结研究的热点,并已有大量文献报道[2,13,19]。
目前甲状腺癌颈部淋巴结转移仍是甲状腺癌治疗的主要关注点之一,临床上筛检手段以高频超声影像诊断为主。高频超声可对颈部可疑淋巴结的形态、径线比、内部回声、囊性变、微钙化、周边环绕血流、淋巴结门结构、皮髓质界限等指标进行初步评估,但其诊断准确率仍难以令人满意。如在本研究中,所选择的目标淋巴结均具有不同程度的声像学转移淋巴结特征,而转移性淋巴结仅41.8%。超声引导下颈部淋巴结FNAC因其微创、简便、准确等优势,备受临床医师及患者好评,且在本研究中FNAC诊断准确率为89.1%。但根据我们FNAC操作经验及在与病理科医师交流时发现,FNAC极易受操作者的操作方法影响,如穿刺抽吸的针数、负压大小及抽吸的部位选择等均对获取细胞涂片的质量产生较大影响,而且涂片细胞学诊断与病理科医师的经验密切相关,以上因素容易导致假阴性诊断结果。
FNA-Tg作为一种甲状腺癌颈部转移淋巴结FNAC的附加诊断手段,其操作简便、经济、准确,而且Tg检测可一定程度上避免病理诊断的主观性。在本研究中,应用FNA-Tg检测技术可将甲状腺癌颈部转移淋巴结诊断准确率由FNAC的89.1%提高到96.7%。Jeon等[20]与Holmes等[12]证实,FNA-Tg对甲状腺乳头状癌颈部淋巴结转移鉴别诊断是一种有效、可靠的检查手段。而且Moon等[21]还提出以1.0 ng/ml作为最适诊断截断值。目前因患病人种、地域及检测手段等多种因素影响,对FNA-Tg诊断截断值的确定仍存在较大争议。
本研究初步探讨了FNA-Tg对甲状腺癌颈部淋巴结转移鉴别诊断价值,存在以下欠缺:1)未进行血清Tg、TSH等甲状腺功能指标检测加以分类比较;2)未根据手术病理诊断加以细化分类分析比较;3)研究样本存在一定区域性,且阳性样本量相对较小,在今后研究中拟针对上述情况进行进一步研究。
综上所述,FNA-Tg作为一种安全、简便、可靠、准确的辅助检查手段,可提高FNAC对甲状腺癌颈部转移淋巴结的诊断准确率。
1 Sherman SI. Thyroid carcinoma[J]. Lancet, 2003, 361(9356):501-511.
2 Chung J, Kim EK, Lim H, et al. Optimal indication of thyroglobulin measurement in fine-needle aspiration for detecting lateral metastatic lymph nodes in patients with papillary thyroid carcinoma[J]. Head Neck, 2014, 36(6): 795-801.
3 Nixon IJ, Shaha AR. Management of regional nodes in Thyroid Cancer[J]. Oral Oncol, 2013, 49(7): 671-675.
4 Vayisoglu Y, Ozcan C. Involvement of level IIb lymph node metastasis and dissection in thyroid cancer[J]. Gland Surg, 2013, 2(4):180-185.
5 Eun YG, Lee YC, Kwon KH. Predictive factors of contralateral paratracheal lymph node metastasis in papillary thyroid cancer:prospective multicenter study[J]. Otolaryngol Head Neck Surg,2014, 150(2): 210-215.
6 Giacomini CP, Jeffrey RB, Shin LK. Ultrasonographic evaluation of malignant and normal cervical lymph nodes[J]. Semin Ultrasound CT MR, 2013, 34(3): 236-247.
7 Kim DW, Choo HJ, Lee YJ, et al. Sonographic features of cervical lymph nodes after thyroidectomy for papillary thyroid carcinoma[J]. J Ultrasound Med, 2013, 32(7): 1173-1180.
8 Aysan E, Ersoy Y, Gucin Z, et al. New thyroid fine needle aspiration biopsy needle. Prospective, randomized, clinical study[J/OL]. http://dx.doi.org/10.1111/cen.12554
9 Choi SH, Baek JH, Lee JH, et al. Thyroid nodules with initially non-diagnostic, fine-needle aspiration results: comparison of coreneedle biopsy and repeated fine-needle aspiration[J/OL]. http:// link.springer.com/article/10.1007%2Fs00330-014-3325-4
10 Bahn RS, Castro MR. Approach to the patient with nontoxic multinodular goiter[J]. J Clin Endocrinol Metab, 2011, 96(5):1202-1212.
11 Grani G, Fumarola A. Thyroglobulin in lymph node fine-needle aspiration washout: a systematic review and meta-analysis of diagnostic accuracy[J]. J Clin Endocrinol Metab, 2014, 99(6):1970-1982.
12 Holmes BJ, Sokoll LJ, Li QK. Measurement of fine-needle aspiration thyroglobulin levels increases the detection of metastatic papillary thyroid carcinoma in cystic neck lesions[J]. Cancer Cytopathol,2014, 122(7):521-526.
13 Kim MJ, Kim EK, Kim BM, et al. Thyroglobulin measurement in fine-needle aspirate washouts: the criteria for neck node dissection for patients with thyroid cancer[J]. Clin Endocrinol (Oxf), 2009,70(1): 145-151.
14 Giovanella L, Ceriani L, Suriano S, et al. Thyroglobulin measurement on Fine-Needle washout fluids: influence of sample collection methods[J]. Diagn Cytopathol, 2009, 37(1): 42-44.
15 Cunha N, Rodrigues F, Curado F, et al. Thyroglobulin detection in fine-needle aspirates of cervical lymph nodes: a technique for the diagnosis of metastatic differentiated thyroid cancer[J]. Eur J Endocrinol, 2007, 157(1): 101-107.
16 Salmaslioglu A, Erbil Y, Citlak G, et al. Diagnostic value of thyroglobulin measurement in fine-needle aspiration biopsy for detecting metastatic lymph nodes in patients with papillary thyroid carcinoma[J]. Langenbecks Arch Surg, 2011, 396(1): 77-81.
17 付庆锋,周乐,边学海,等.甲状腺乳头状癌颈部淋巴结转移FNA-Tg诊断标准值的探讨[J].中华内分泌外科杂志,2013,7(2):154-156.
18 Pacini F, Fugazzola L, Lippi F, et al. Detection of thyroglobulin in fine needle aspirates of nonthyroidal neck masses: a clue to the diagnosis of metastatic differentiated thyroid cancer[J]. J Clin Endocrinol Metab, 1992, 74(6):1401-1404.
19 Suh YJ, Son EJ, Moon HJ, et al. Utility of thyroglobulin measurements in fine-needle aspirates of space occupying lesions in the thyroid bed after thyroid cancer operations[J]. Thyroid, 2013,23(3):280-288.
20 Jeon MJ, Park JW, Han JM, et al. Serum antithyroglobulin antibodies interfere with thyroglobulin detection in Fine-Needle aspirates of metastatic neck nodes in papillary thyroid carcinoma[J]. J Clin Endocrinol Metab, 2013, 98(1): 153-160.
21 Moon JH, Kim YI, Lim JA, et al. Thyroglobulin in washout fluid from lymph node fine-needle aspiration biopsy in papillary thyroid cancer:large-scale validation of the cutoff value to determine malignancy and evaluation of discrepant results[J]. J Clin Endocrinol Metab,2013, 98(3):1061-1068.
Value of FNA-Tg in differential diagnosis of suspicious cervical lymph node metastasis in patients with suspicious thyroid cancer
HE Tiejun1, YANG Bai2, ZHANG Yang31Department of Ultrasound, the Third Aff i liated Hospital of Liaoning Medical University, Jinzhou 121000, Liaoning Province, China;2The First Aff i liated Hospital of Liaoning Medical University, Jinzhou 121000, Liaoning Province, China;3Linghe District Hospital, Jinzhou 121000, Liaoning Province, China
Objective To investigate the value of FNA-Tg in differential diagnosis of suspicious cervical lymph node metastasis in patients with suspicious thyroid cancer. Methods All cases enrolled in this study were selected from patients with thyroid nodular in the Third Aff i liated Hospital of Liaoning Medical University from July 2010 to March 2014. A total of 184 patients with suspicious cervical lymph node metastasis were detected by ultrasound (US) and 104 patients were found to have suspicious thyroid cancer, and they all underwent US-guided fine-needle aspiration cytology (FNAC), then their thyroglubin in FNA washout fluid (FNA-Tg) were assayed. The accuracy of FNAC and FNA-Tg in diagnosing the cervical lymph node metastasis was assessed with the pathological diagnosis after surgical resection as the golden reference. Results Compared with the pathological diagnosis, the sensitivity, specificity and accuracy of FNAC and FNA-Tg in diagnosing the cervical lymph node metastasis were 74.0%, 100%, 89.1% and 92.2%, 100%, 96.7%, respectively. The signif i cant difference was detected between FNAC and pathological diagnosis (P=0.03), while no signif i cant difference was found between FNA-Tg and pathological diagnosis (P=0.23). Conclusion As a safe, convenient, reliable and accurate auxiliary method, FNA-Tg can improve the diagnostic accuracy of cervical lymph node metastasis in patients with suspicious thyroid cancer.
ultrasound; puncture biopsy; thyroid cancer; cervical lymph node
R 445.1
A
2095-5227(2015)02-0136-04
10.3969/j.issn.2095-5227.2015.02.012
时间:2014-10-29 10:16
http://www.cnki.net/kcms/detail/11.3275.R.20141029.1016.001.html
2014-08-04
赫铁军,男,硕士。专业方向:超声诊断与超声介入治疗。Email: hetiejun3@sina.com
The fi rst author: HE Tiejun. Email: hetiejun3@sina.com
