肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的预测指标研究
2015-02-21王万鹏高海英贾德兴
王万鹏,冯 静,许 蕾,高海英,贾德兴
·论著·
肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的预测指标研究
王万鹏,冯 静,许 蕾,高海英,贾德兴
目的 了解血清腹腔积液清蛋白梯度(SAAG)、门静脉内径(PVD)及血小板计数与脾长径比值(Plt/S-D)联合应用对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的预测价值。方法 抽取2013年1—12月,在潍坊医学院附属潍坊市人民医院接受住院治疗的肝炎肝硬化患者50例。根据有无食管胃底静脉曲张破裂出血,将其分为出血组(n=26)和非出血组(n=24)。比较并分析两组SAAG、PVD及Plt/S-D,绘制SAAG、PVD、Plt/S-D及三者联合应用对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血预测的受试者工作特征(ROC)曲线。结果 (1)两组SAAG、PVD及Plt/S-D比较,差异有统计学意义(P<0.01);非条件Logistic回归分析显示,SAAG、PVD及Plt/S-D对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的影响有统计学意义(P<0.05)。(2)SAAG、PVD、Plt/S-D对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血预测的ROC曲线下面积分别为0.74、0.81及0.67。SAAG取值为20.50 g/L时,灵敏度为80.8%,特异度为58.3%;取值为20.10 g/L时,灵敏度为65.4%,特异度为62.5%。PVD取值为13.50 mm时,灵敏度为80.8%,特异度为66.3%;取值为14.25 mm时,灵敏度为65.4%,特异度为83.3%。Plt/S-D取值为0.88×109个/mm时,灵敏度为80.8%,特异度为66.7%;取值为0.97×109个/mm时,灵敏度为65.4%,特异度为66.7%。(3)SAAG、PVD及Plt/S-D联合应用对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血预测的评分公式为:预测出血评分=SAAG×PVD÷Plt/S-D,ROC曲线下面积为0.91,取值为890.35时有最佳的灵敏度和特异度,分别为87.8%和90.7%。结论 SAAG、PVD及Plt/S-D是肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的影响因素,三项联合应用对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的预测价值较高。
肝炎;肝硬化;食管胃底静脉曲张破裂出血;预测
王万鹏,冯静,许蕾,等.肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的预测指标研究[J].中国全科医学,2015,18(22):2676-2679.[www.chinagp.net]
Wang WP,Feng J,Xu L,et al.Predictive indicators of esophageal varices bleeding in hepatitis patients with liver cirrhosis[J].Chinese General Practice,2015,18(22):2676-2679.
我国约有50%的肝硬化患者存在食管胃底静脉曲张,而门静脉高压所致的食管胃底静脉曲张破裂出血是肝硬化患者常见的严重并发症之一,年发病率为5%~15%[1],病死率超过20%[2-3]。尽管40%的肝硬化患者的食管胃底静脉曲张破裂出血可以自行停止或经内科治疗改善,但治疗后近期内再出血的病死率仍高达20%左右[1]。因此,准确预测肝硬化患者食管胃底静脉曲张破裂出血风险,对预防出血、改善预后及降低病死率都极为重要。目前,临床上一般以内镜检查为食管胃底静脉曲张的诊断方法,通过对曲张静脉进行分析来预测出血风险。但内镜检查本身就存在诱发出血的潜在风险,且易受患者身体情况和其他因素的影响,故多数患者无法耐受或拒绝接受此检查。既往有研究尝试采用其他替代指标来诊断或预测食管胃底静脉曲张程度和破裂出血风险,如血小板计数、脾脏大小及门静脉内径(PVD)等,但单一应用这些指标的预测价值较低[4-5]。本研究同时采用血清腹腔积液清蛋白梯度(SAAG)、PVD及血小板计数与脾长径比值(Plt/S-D)对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血进行预测,旨在评价三者联合应用对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的预测价值。
1 对象与方法

1.2 研究方法
1.2.1 一般资料收集 采用查看病历的方式,收集患者一般资料,包括性别、年龄、饮酒情况、临床症状、用药情况及既往病史等。
1.2.2 指标检测 (1)于空腹状态下,抽取患者静脉血,采用罗氏全自动生化分析仪进行血清清蛋白检测和血常规检查;(2)在患者知情同意的情况下,行腹腔穿刺术,采用罗氏全自动生化分析仪进行腹腔积液清蛋白定量检测;(3)采用GE彩色多普勒(美国)测量患者PVD和脾脏长径。SAAG=血清清蛋白-腹腔积液清蛋白。

2 结果
2.1 两组SAAG、PVD及Plt/S-D比较 两组SAAG、PVD及Plt/S-D比较,差异均有统计学意义(P<0.01,见表1)。
2.2 肝炎肝硬化患者并发食管胃底静脉曲张破裂出血影响因素的非条件Logistic回归分析 以食管胃底静脉曲张破裂出血为应变量,以SAAG、PVD及Plt/S-D为自变量,进行非条件Logistic回归分析。结果显示,SAAG、PVD及Plt/S-D对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的影响有统计学意义(P<0.05,见表2)。
2.3 SAAG、PVD、Plt/S-D及三者联合应用对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的预测价值 (1)绘制SAAG、PVD及Plt/S-D对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血预测的ROC曲线(见图1)。ROC曲线下面积分别为0.74、0.81及0.67,以灵敏度和特异度和的最大值确定每个参数的最佳临界点:SAAG取值为20.50 g/L时,灵敏度为80.8%,特异度为58.3%;取值为20.10 g/L时,灵敏度为65.4%,特异度为62.5%。PVD取值为13.50 mm时,灵敏度为80.8%,特异度为66.3%;取值为14.25 mm时,灵敏度为65.4%,特异度为83.3%。Plt/S-D取值为0.88×109个/mm时,灵敏度为80.8%,特异度为66.7%;取值为0.97×109个/mm时,灵敏度为65.4%,特异度为66.7%。(2)联合应用SAAG、PVD及Plt/S-D,建立预测肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的评分系统,预测出血评分=SAAG×PVD÷Plt/S-D,计算每例患者的总分。以1-特异度为横坐标,以灵敏度为纵坐标构建ROC曲线(见图2),所得曲线下面积为0.91,取值为890.35时,有最佳灵敏度和特异度,分别为87.8%和90.7%。

表1 两组SAAG、PVD及Plt/S-D比较
注:SAAG=血清腹腔积液清蛋白梯度,PVD=门静脉内径,Plt/S-D=血小板计数与脾长径比值
表2 肝炎肝硬化患者并发食管胃底静脉曲张破裂出血影响因素的非条件Logistic回归分析
Table 2 Non-conditional logistic regression analysis of influencing factors for EGVB in hepatitis patients with liver cirrhosis

自变量β值SEWaldχ2值P值OR(95%CI)SAAG008007104<005109(107,127)PVD054018853<005171(119,242)Plt/S-D043075031<005154(132,602)
3 讨论
肝硬化导致的门静脉高压是食管胃底静脉曲张破裂出血的主要原因,门静脉高压发生时,食管胃底静脉曲张程度加重,出血风险增加。有研究显示,当门静脉压力>12 mm Hg(1 mm Hg=0.133 kPa)时,食管胃底曲张的静脉压力达到管壁弹性限度,静脉曲张破裂出血发生,故监测门静脉压力对预测出血有重要意义[6]。吴诗品等[7]发现,PVD>13 mm、脾静脉内径>9 mm,提示门静脉高压;PVD>14 mm、脾静脉内径>10 mm,提示有食管胃底静脉曲张可能性。肖绍树[8]发现,肝硬化患者PVD≥15 mm、脾静脉内径≥10 mm,可作为预测食管胃底静脉曲张破裂出血的参考指标。Chalasani等[9]发现,脾脏增大和血小板计数降低是重度静脉曲张的独立预测因子,脾脏增大是门静脉高压的表现之一。
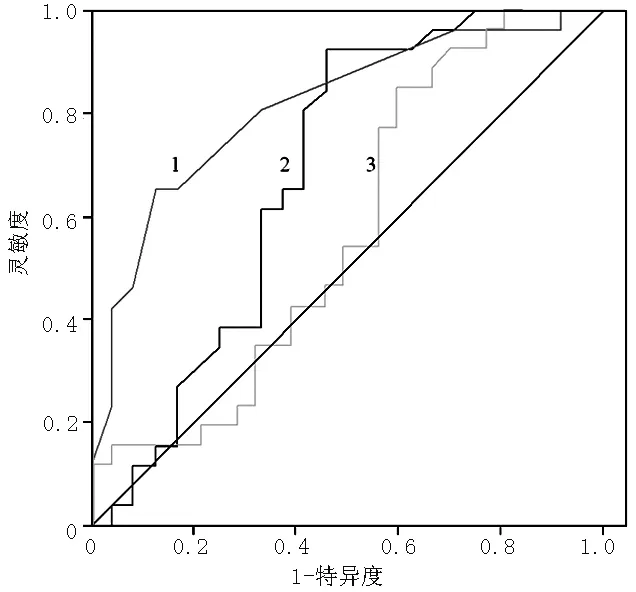
注:1:SAAG=血清腹腔积液清蛋白梯度,2:PVD=门静脉内径,3:Plt/S-D=血小板计数与脾长径比值
图1 SAAG、PVD及Plt/S-D对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血预测的ROC曲线
Figure 1 The ROC curves of SAAG,PVD and Plt/S-D predicting EGVB in hepatitis patients with liver cirrhosis

图2 SAAG、PVD及Plt/S-D联合应用对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血预测的ROC曲线
Figure 2 ROC curves of the combined application of SAAG,PVD and Plt/S-D predicting EGVB in hepatitis patients with liver cirrhosis
Giannini等[10]对266例肝硬化患者分别进行了回顾性和前瞻性研究,发现当Plt/S-D临界值为909时,静脉曲张程度的阳性预测值和阴性预测值分别为96%和100%。李朝辉等[11]对73例肝硬化并发食管胃底静脉曲张的患者进行回顾性分析,发现Plt/S-D与食管胃底静脉曲张程度呈明显相关性,且所有重度曲张患者的Plt/S-D均≤894。Chawla等[12]通过研究发现,Plt/S-D可以成为一个筛检门静脉高压患者初级预防内镜检查的实用参数模型。有研究显示,SAAG只由门静脉压力决定,不受血清清蛋白、腹腔积液感染、利尿剂使用、治疗性腹腔穿刺、清蛋白输注及肝脏疾病病因等因素影响,且SAAG与门静脉压力呈正相关关系,随着SAAG的升高,食管胃底静脉曲张和破裂出血发生率升高,提示SAAG对肝硬化门静脉高压性食管胃底静脉曲张破裂出血有较高的预测价值[13-14]。SAAG>20 g/L,需高度警惕食管胃底静脉曲张破裂出血的可能[15]。
门静脉压的检测包括游离肝静脉压力、肝静脉插管测定肝静脉契压、肝静脉压力梯度及门静脉造影时测压等,也可以在内镜下直接行静脉穿刺测压。其中内镜下静脉穿刺测压和肝静脉压力梯度的临床价值较高,但实际操作较难,目前主要用于科学研究。现在临床上主要通过内镜检查食管胃底静脉曲张程度来预测破裂出血风险,但内镜检查在操作过程中会给患者带来痛苦,有诱发出血的危险,且容易受患者身体状况限制,临床上难以普及。近年来,研究者们开始探讨采用实验室检查、超声影像学及CT等无创性手段来评估门静脉高压和食管胃底静脉曲张程度,以达到预测消化道出血风险的目的。
本研究结果显示,出血组患者的SAAG、PVD及Plt/S-D与非出血组患者比较,差异有统计学意义。非条件Logistic回归分析显示,SAAG、PVD及Plt/S-D均为肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的独立危险因素。为了全面、准确地评价SAAG、PVD及Plt/S-D的预测价值,以 1-特异度为横坐标,以灵敏度为纵坐标,构建SAAG、PVD及Plt/S-D的ROC曲线,ROC曲线下面积分别为0.74、0.81及0.67,提示使用单一因素预测肝炎肝硬化并发食管胃底静脉曲张破裂出血的灵敏度和特异度均不高,出血预测价值较低。为提高灵敏度和特异度,联合应用SAAG、PVD及Plt/S-D建立一个预测出血评分系统,根据评分构建ROC曲线,所得曲线下面积为0.91,取值为890.35时有最佳灵敏度和特异度,且灵敏度和特异度水平较高,提示当肝炎肝硬化患者的出血评分达到890.35时应进行出血预防性治疗。
综上所述,SAAG、PVD及Plt/S-D均为肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的影响因素,且三者联合应用对肝炎肝硬化患者并发食管胃底静脉曲张破裂出血的预测价值较高,可用于出血高危人群的初步筛查。
[1]Garcia-Tsao G,Sanyal AJ,Grace ND,et al.Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis[J].Hepatology,2007,46(3):922-938.
[2]D′Amico G,De Franchis R.Upper digestive bleeding in cirrhosis.Post-therapeutic outcome and prognostic indicators[J].Hepatology,2003,38(3):599-612.
[3]Carbonell N,Pauwels A,Serfaty L,et al.Improved survival after variceal bleeding in patients with cirrhosis over the past two decades[J].Hepatology,2004,40(3):652-659.
[4]Sharma SK,Aggarwal R.Prediction of large esophageal varices in patients with cirrhosis of the liver using clinical,laboratory and imaging parameters[J].J Gastroenterol Hepatol,2007,22(11):1909-1915.
[5]Sarangapani A,Shanmugam C,Kalyanasundaram M,et al.Noninvasive prediction of large esophageal varices in chronic liver disease patients[J].Saudi J Gastroenterol,2010,16(1):38-42.
[6]唐羿,潘凤莲,刘星.肝硬化门静脉高压上消化道出血手术治疗的体会[J].局解手术学杂志,2011,20(1):112.
[7]Wu SP,Huang ZZ.Ultrasonographic prediction of esophageal variceal bleeding in liver cirrhosis patient[J].Chinese J Ultrasound Med,1998,14(7):29-30.(in Chinese) 吴诗品,黄自在.B型超声显像预测肝硬化食管静脉曲张破裂出血[J].中国超声医学杂志,1998,14(7):29-30.
[8]肖绍树.食管静脉曲张破裂出血危险的预测[J].新医学,1996,27(4):222-223.
[9]Chalasani N,Imperiale TF,Ismail A,et al.Predictors of large esophageal varices in patients with cirrhosis[J].Am J Gastroenterol,1999,94(11):3285-3291.
[10]Giannini E,Botta F,Borro P,et al.Platelet count/spleen diameter ratio:proposal and validation of a non-invasive parameter to predict the presence of oesophageal varices in patients with liver cirrhosis[J].Gut,2003,52(8):1200-1205.
[11]李朝辉,武焕弟.非侵入性检查预测肝硬化食管静脉曲张的临床研究[J].当代医学,2011,17(9):236-237.
[12]Chawla S,Katz A,Attar BM,et al.Platelet count/spleen diameter ratio to predict the presence of esophageal varices in patients with cirrhosis:a systematic review[J].Eur J Gastroenterol Hepatol,2012,24(4):431-436.
[13]Jiang CF,Shi B,Xie WF.The value of serum-ascites albumin gradient for predicting esophageal-gastric fundus variceal bleeding[J].China J Dig,2011,31(9):591-593.(in Chinese) 蒋彩凤,施斌,谢渭芬.血清腹水白蛋白梯度对食管胃底静脉曲张破裂出血的预测价值[J].中华消化杂志,2011,31(9):591-593.
[14]Han L,Xu QY,Xu XN.Subject relationship between serum ascites albumin gradient and esophageal variceal bleeding[J].China Pra Med,2010,5(26):48-50.(in Chinese) 韩琳,许秋泳,许向农.血清-腹水白蛋白梯度与食管静脉曲张破裂出血的关系[J].中国实用医药,2010,5(26):48-50.
[15]Zhang L,Zhang ST,Yu ZL.Study of the relationship between serum-ascites album in gradient and esophageal-gastric fundus variceal bleeding[J].J Clin Intem Med,2007,24(2):92-93.(in Chinese) 张莉,张澍田,于中麟.血清-腹水白蛋白梯度与食管-胃底静脉曲张破裂出血的关系[J].临床内科杂志,2007,24(2):92-93.
(本文编辑:王凤微)
Predictive Indicators of Esophageal Varices Bleeding in Hepatitis Patients With Liver Cirrhosis
WANGWan-peng,FENGJing,XULei,etal.
DepartmentofInfectiousDiseases,WeifangPeople′sHospital,Weifang261041,China
Objective To evaluate the value of the combined application of serum-ascites albumin gradient(SAAG),portal vein diameter(PVD) and the ratio of platelet count/spleen-diameter(Plt/S-D) in predicting esophageal varices bleeding(EGVB) in hepatitis patients with liver cirrhosis.Methods We enrolled 50 hepatitis patients with liver cirrhosis who received hospitalized treatment in Weifang People′s Hospital Affiliated to Weifang Medical College from January to December 2013.According to whether EGVB occurred,the subjects were divided into two groups:bleeding group(n=26) and non-bleeding group(n=24).We analyzed and compared SAAG,PVD and Plt/S-D between the two groups.The ROC curves of SAAG,PVD,Plt/S-D and their combined application predicting EGVB in hepatitis patients with liver cirrhosis was drawn.Results (1)The two groups were significantly different(P<0.01) in SAAG,PVD and Plt/S-D;non-conditional logistic regression analysis showed that SAAG,PVD and Plt/S-D had significant influence(P<0.05) on EGVB in hepatitis patients with liver cirrhosis.(2)The areas under ROC curves of SAAG,PVD and Plt/S-D predicting EGVB in hepatitis patients with liver cirrhosis were 0.74,0.81 and 0.67 respectively.When the value of SAAG was 20.50 g/L,the corresponding sensitivity was 80.8% and the specificity was 58.3%;when the value of SAAG was 20.10 g/L,the corresponding sensitivity was 65.4% and the specificity was 62.5%.When the value of PVD was 13.50 mm,the corresponding sensitivity was 80.8% and the specificity was 66.3%;when the value of PVD was 14.25 mm,the corresponding sensitivity was 65.4% and the specificity was 83.3%.When the value of Plt/S-D was 0.88×109个/mm,the corresponding sensitivity was 80.8% and the specificity was 66.7%;when the value of Plt/S-D was 0.97×109个/mm,the corresponding sensitivity was 65.4% and the specificity was 66.7%.(3)The evaluation formula of the combined application of SAAG,PVD and Plt/S-D predicting EGVB in hepatitis patients with liver cirrhosis was found:score of bleeding prediction=SAAG×PVD÷Plt/S-D.When the area under ROC was 0.91 and the value was 890.35,we got the highest sensitivity and specificity,which were 87.8% and 90.7%.Conclusion SAAG,PVD and Plt/S-D are the influencing factors for EGVB in hepatitis patients with liver cirrhosis.The combined application of the three factors has higher value in predicting EGVB in hepatitis patients with liver cirrhosis.
Hepatitis;Liver cirrhosis;Esophageal varices bleeding;Forecasting
261041 山东省潍坊市人民医院感染性疾病科
王万鹏,261041 山东省潍坊市人民医院感染性疾病科;E-mail:wangwanpeng0630@163.com
R 575
A
10.3969/j.issn.1007-9572.2015.22.013
2015-04-02;
2015-06-01)
