直乙肠交界处癌与直肠癌及乙状结肠癌的预后比较
2015-02-21徐建梅刘风玲
孔 雁,徐建梅,刘风玲,左 静
·论著·
直乙肠交界处癌与直肠癌及乙状结肠癌的预后比较
孔 雁,徐建梅,刘风玲,左 静
目的 探讨直乙肠交界处癌与直肠癌、乙状结肠癌预后的差异及影响因素。方法 选取2008年1月—2012年12月河北医科大学第四医院收治的结直肠癌患者354例为研究对象,收集患者临床特征资料。以手术日期或病理确诊日期为随访起点对患者或家属进行随访,以肿瘤复发、转移及死亡为终点事件,随访时间截至2014-01-01,无进展生存期(PFS)定义为从确诊至肿瘤复发、转移或死亡的时间。结果 直乙肠交界处癌、直肠癌和乙状结肠癌患者年龄、初始治疗方式、肿瘤最长径及浸润深度比较,差异有统计学意义(χ2=0.009、0.015、0.019、0.005,P<0.05)。354例患者失访17例,失访率为4.8%;随访时间3~91个月,中位随访时间为44个月。直乙肠交界处癌中位生存时间为64.0个月〔95%CI(47.5,80.5)〕,1、2、3年生存率分别为93.6%、85.3%和76.2%;直肠癌中位生存时间为63.0个月〔95%CI(53.2,72.8)〕,1、2、3年生存率分别为93.4%、85.5%和76.3%;乙状结肠癌中位生存时间为63.0个月〔95%CI(51.2,74.8)〕,1、2、3年生存率分别为94.5%、87.2%和79.3%。直乙肠交界处癌、直肠癌和乙状结肠癌患者生存曲线比较,差异无统计学意义(χ2=1.246,P=0.536)。直乙肠交界处癌、直肠癌和乙状结肠癌中位PFS分别为48.0个月〔95%CI(36.3,59.7)〕、29.0个月〔95%CI(17.9,40.1)〕和63.0个月〔95%CI(37.1,88.9)〕。直乙肠交界处癌、直肠癌和乙状结肠癌PFS的生存曲线比较,差异有统计学意义(χ2=17.329,P=0.001)。Cox比例风险回归分析结果显示,肿瘤部位〔HR=0.585,95%CI(0.338,0.891),P=0.012〕及浸润深度〔HR=3.516,95%CI(1.883,6.746),P=0.038〕是影响结直肠癌患者PFS的独立预测因素。结论 直乙肠交界处癌与直肠癌、乙状结肠癌生存时间未见不同,而PFS存在差异,肿瘤浸润深度可能为结直肠癌患者PFS的影响因素。
结肠肿瘤;乙状结肠肿瘤;直肠肿瘤;预后
结直肠癌是常见的恶性肿瘤之一,直乙肠交界处是结肠癌的好发部位,据报道,乙状结肠癌及直乙肠交界处癌占结肠癌的27.8%[1]。直乙肠交界处位于第3骶椎前方,乙状结肠近直角与直肠交界处,是全部结肠中最狭窄位置,因此直乙肠交界处癌易误诊、漏诊[2]。有关直乙肠交界处癌与直肠癌、乙状结肠癌预后比较研究较为少见,本研究对直乙肠交界处癌与直肠癌、乙状结肠癌预后进行比较,分析三者的临床特点。
1 资料与方法
1.1 一般资料 选取2008年1月—2012年12月于河北医科大学第四医院治疗的结直肠癌患者354例为研究对象,其中男202例,女152例;年龄19~82岁,平均年龄(59.1±12.2)岁;直乙肠交界处癌92例,直肠癌113例,乙状结肠癌149例。患者均经手术病理或临床活检确诊,明确肿瘤部位,并经过完整规范化治疗。排除标准:(1)存在其他部位的原发肿瘤;(2)其他组织来源的肿瘤,如黑色素瘤、淋巴瘤等;(3)随访资料不完整。
1.2 方法
1.2.1 资料收集 收集患者性别、年龄、病理分期、初始治疗方式、肿瘤大小、浸润深度及淋巴结阳性比例等临床特征。
1.2.2 随访 以电话形式随访患者或家属,随访起点为手术日期或病理确诊日期,以肿瘤复发、转移、死亡为终点事件,随访时间截至2014-01-01,随访期间失访及未出现终点事件的患者定义为截尾。无进展生存期(PFS)定义为从确诊至肿瘤复发、转移或死亡的时间。
1.3 统计学方法 采用SPSS 16.0统计软件进行统计分析,计数资料的分析采用χ2检验;采用Kaplan-Meier绘制生存曲线,以Log-rank检验比较不同部位结直肠癌患者的生存率;采用Cox比例风险回归模型分析不同部位结直肠癌患者预后的影响因素。以P<0.05为差异有统计学意义。
2 结果
2.1 临床特征 直乙肠交界处癌、直肠癌和乙状结肠癌患者性别、病理分期及淋巴结阳性比例比较,差异无统计学意义(P>0.05);而年龄、初始治疗方式、肿瘤最长径及浸润深度比较,差异有统计学意义(P<0.05,见表1)。
表1 不同部位结直肠癌患者临床特征比较〔n(%)〕
Table 1 Comparison of clinical features among patients with colorectal neoplasm at different sites

临床特征直乙肠交界处癌(n=92)直肠癌(n=113)乙状结肠癌(n=149)χ2值P值性别18320400 男54(587)69(611)79(530) 女38(413)44(389)70(470)年龄(岁)130330011 <459(98)18(159)29(195) 45~6020(217)43(381)44(295) >6063(685)52(460)76(510)病理分期(期)113650078 Ⅰ12(130)21(186)8(54) Ⅱ38(413)45(398)67(450) Ⅲ32(348)37(327)58(389) Ⅳ10(109)10(89)16(107)初始治疗方式128750012 根治术78(848)103(912)133(893) 姑息术11(120)4(35)16(107) 姑息化疗3(32)6(53) 0 肿瘤最长径(cm)76980021 ≤567(728)87(770)92(617) >525(272)26(230)57(383)浸润深度a23833<0001 T1+T213(144)26(243)10(68) T365(722)75(701)105(719) T412(134)6(56)31(213)淋巴结阳性比例a29210232 ≥0318(205)13(124)19(134) <0370(795)92(876)123(866)
注:a表示部分晚期患者未行手术治疗,缺乏术后病理,无法明确浸润深度及淋巴结转移数目
2.2 生存时间 354例患者中失访17例,失访率为4.8%;随访时间3~91个月,中位随访时间为44个月。直乙肠交界处癌中位生存时间为64.0个月〔95%CI(47.5,80.5)〕,1、2、3年生存率分别为93.6%、85.3%和76.2%;直肠癌中位生存时间为63.0个月〔95%CI(53.2,72.8)〕,1、2、3年生存率分别为93.4%、85.5%和76.3%;乙状结肠癌中位生存时间为63.0个月〔95%CI(51.2,74.8)〕,1、2、3年生存率分别为94.5%、87.2%和79.3%。直乙肠交界处癌、直肠癌和乙状结肠癌患者生存曲线比较,差异无统计学意义(χ2=1.246,P=0.536,见图1)。

图1 不同部位结直肠癌患者生存曲线
Figure 1 Survival curves of patients with colorectal neoplasm at different sites
2.3 PFS 直乙肠交界处癌、直肠癌和乙状结肠癌中位PFS分别为48.0个月〔95%CI(36.3,59.7)〕、29.0个月〔95%CI(17.9,40.1)〕和63.0个月〔95%CI(37.1,88.9)〕。直乙肠交界处癌、直肠癌和乙状结肠癌PFS的生存曲线比较,差异有统计学意义(χ2=17.329,P=0.001,见图2)。
2.4 Cox比例风险回归分析 以患者临床特征及肿瘤部位为自变量,是否出现疾病进展为因变量行Cox比例风险回归分析,变量赋值见表2。Cox比例风险回归分析结果显示,肿瘤部位及浸润深度是影响结直肠癌患者PFS的独立预测因素(P<0.05,见表3)。
3 讨论
直乙肠交界处癌在结直肠癌中较为常见,目前临床对直乙肠交界处癌检查方法不够完善,X线检查极易误诊、漏诊,内镜检查则把乙状结肠螺旋形黏膜皱褶作为直肠与乙状结肠的分界线,由于直乙肠交界距肛门15 cm 以上,临床上极少将其作为独立病种进行诊治。
既往研究发现,结直肠癌在胚胎发生、解剖、生理和功能上有很大区别,不同部位的结直肠癌易感人群、发病机制及病理生理特征、治疗方法和预后等也存在差异[3-6]。在我国,直肠癌的发病率远高于结肠癌,预后也较结肠癌差[7]。诊断年龄是结肠癌患者预后的主要影响因素,而肿瘤的生长方式是直肠癌患者预后的主要影响因素[8-9]。直乙肠交界处作为结肠和直肠的分界线,其肿瘤的发病机制、治疗及预后可能与直肠癌、乙状结肠癌存在差异,但引起其差异的具体原因尚无定论。

图2 不同部位结直肠癌患者PFS的生存曲线
Figure 2 Survival curves of PFS of patients with colorectal neoplasm at different sites
表2 结直肠癌患者PFS影响因素的Cox比例模型分析变量赋值
Table 2 Variable assignment of Cox regression analysis on influencing factors for PFS of patients with colorectal cancer
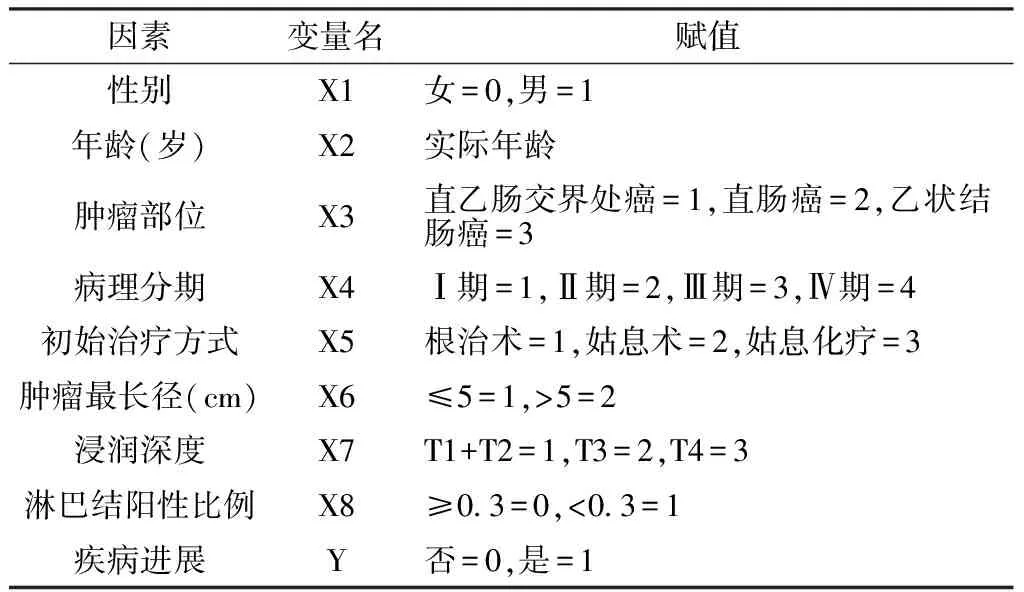
因素变量名赋值性别X1女=0,男=1年龄(岁)X2实际年龄肿瘤部位X3直乙肠交界处癌=1,直肠癌=2,乙状结肠癌=3病理分期X4Ⅰ期=1,Ⅱ期=2,Ⅲ期=3,Ⅳ期=4初始治疗方式X5根治术=1,姑息术=2,姑息化疗=3肿瘤最长径(cm)X6≤5=1,>5=2浸润深度X7T1+T2=1,T3=2,T4=3淋巴结阳性比例X8≥03=0,<03=1疾病进展Y否=0,是=1
表3 结直肠癌患者PFS影响因素的Cox比例模型分析
Table 3 Cox regression analysis on influencing factors for PFS of patients with colorectal cancer

变量名bSEWaldχ2值HR(95%CI)P值X10002000305451002(0996,1008)0460X20300015836251350(0991,1839)0057X3-0536021462550585(0338,0891)0012X4-0124011012650884(0713,1096)0261X5-0077018601740925(0643,1331)0676X60172021906191188(0773,1826)0432X70832040043203516(1883,6746)0038X80249014728891283(0963,1711)0089
DNA倍体是影响肿瘤预后的重要因素,若肿瘤细胞为二倍体,其预后将优于非整倍体肿瘤[10]。DNA二倍体多见于近端结肠癌,5氟尿嘧啶(5-FU)治疗使近端结肠癌患者获益较大,而远端结肠癌患者获益较小,提示从近端结肠癌、远端结肠癌到直肠癌,预后逐渐变差[11]。本研究结果发现,乙状结肠癌、直乙肠交界处癌和直肠癌中位PFS分别为63.0、48.0和29.0个月,且生存曲线存在差异,与上述结果相似。
在直乙肠交界处癌的诊断及治疗过程中,应采取不同于乙状结肠癌及直肠癌的手段。在下一步的研究中,应用大样本的前瞻性研究以探讨直乙肠交界处癌的发生机制,以加深临床对该病的认识。
[1]周永昌,郭万学.超声医学[M].4版.上海:科学技术文献出版社,2002:1083.
[2]Yu JY,Ding HY,Ding YQ,et al.Analysis of pathological diagnosis for biopsy of colorectal carcinoma[J].Chinese Journal of Diagnostic Pathology,2005,12(1):13-16,88-89.(in Chinese) 虞积耀,丁华野,丁彦青,等.结肠、直肠癌活检病理诊断的探讨[J].诊断病理学杂志,2005,12(1):13-16,88-89.
[3]Faivre J,Bédenne L,Boutron MC,et al.Epidemiological evidence for distinguishing subsites of colorectal cancer[J].J Epidemiol Community Health,1989,43(4):356-361.
[4]Stewart T,Henderson R,Grayson H,et al.Reduced incidence of rectal cancer,compared to gastric and colonic cancer,in a population of 73,076 men and women chronically immunosuppressed[J].Clin Cancer Res,1997,13(1):51-55.
[5]Nelson H,Petrelli M,Carlin A,et al.Guidelines 2000 for colon and rectal cancer surgery[J].J Natl Cancer Inst,2001,93(8):583-596.
[6]Frattini M,Balestra D,Suardi S,et al.Different genetic features associated with colon and rectal carcinogenesis[J].Clin Cancer Res,2004,10(12):4015-4021.
[7]Li LD,Rao KQ,Zhang SW,et al.Statistical analysis of data from 12 cancer registries in China,1993-1997[J].Bull Chin Cancer,2002,11(9):497-507.
[8]Chan KK,Dassanayake B,Deen R,et al.Young patients with colorectal cancer have poor survival in the first twenty months after operation and predictable survival in the medium and long-term:analysis of survival and prognostic markers[J].World J Surg Oncol,2010(8):82.
[9]Chou CL,Chang SC,Lin TC,et al.Differences in clinicopathological characteristics of colorectal cancer between younger and elderly patients: an analysis of 322 patients from a single institution[J].Am J Surg,2011,202(5):574-582.
[10]徐建明.正确认识结肠癌和直肠癌诊治理念的差异[J].中国实用外科杂志,2012,32(9):703-705.
[11]Xu H,Wang Z,Zeng X.Location and nucleous ploidy of gastrointestinal carcinoid[J].China Tropical Medicine,2009,9(2):255-256.(in Chinese) 徐洪,王箴,曾训.消化道类癌发生部位与核酸倍体[J].中国热带医学,2009,9(2):255-256.
(本文编辑:吴立波)
·读者服务·
《中国全科医学》开通投稿“绿色通道”
为尽快发表对临床及科研具有重大影响和指导价值的课题论文,《中国全科医学》杂志开通了投稿“绿色通道”,凡符合以下条件之一者均可申请进入“绿色通道”:
(1)国家自然科学基金和重大攻关项目论文(请提供基金项目批文的复印件);
(2)经证实具有国际或国内领先水平需尽快发表的前瞻性或创新性论文(请提供省级及以上图书馆或医学信息研究所等单位出具的“查新报告”);
(3)院士及首席科学家项目课题论文;
(4)省自然科学基金论文(请提供基金项目批文的复印件);
(5)有关全科医学教育、全科医疗和社区卫生服务的专项研究课题;
(6)取得专利的研究成果论文(请提供专利批文的复印件);
(7)博士研究生论文(请附导师推荐信)。
对符合“绿色通道”要求的论文,在收稿后21个工作日内就论文审稿结果(“绿色通道”发表、按普通稿件处理、退稿)给予作者答复,对于符合“绿色通道”发表的稿件在收稿后6个月内发表。
“绿色通道”投稿专用邮箱:qkyxjjlw@126.com;咨询电话:15188828922。
Comparison of Prognosis Among Recto-sigmoid Cancer,Rectal Neoplasm and Sigmoid Neoplasm
KONGYan,XUJian-mei,LIUFeng-ling,etal.
TheFourthHospitalofHebeiMedicalUniversity,Shijiazhuang050011,China
Objective To investigate the differences in the prognosis of recto-sigmoid cancer,rectal cancer and sigmoid cancer and the influencing factors.Methods We enrolled 354 patients with colorectal cancer in the Fourth Hospital of Hebei Medical University from January 2008 to December 2012.We collected the data of clinical features of the patients.From the day of surgery or pathological diagnosis,we conducted follow-up visits to patients and their families,and neoplasm recurrence ,metastasis and death were considered as the outcome events respectively.PFS was defined as the time from diagnosis to the neoplasm recurrence,metastasis or death.All follow-up visits were ceased on January 1,2014.Results Patients with the three kinds of neoplasms were significantly different in age,initial treatment method,the longest diameter of the tumor and the depth of infiltration(χ2=0.009,0.015,0.019,0.005;P<0.05).Of the 354 patients,we lost 17 patients with a loss rate of 4.8%; the follow-up time was 3 to 91 months,and the median follow-up time was 44 months.For the patients with recto-sigmoid cancer,the median survival time was 64.0 months〔95%CI(47.5,80.5)〕,and the survival rates of one year,two years and three years were 93.6%,85.3% and 76.2%;for the patients with rectal cancer,the median survival time was 63.0 months〔95%CI(53.2,72.8)〕,and the survival rates of one year,two years and three years were 93.4%,85.5% and 76.3%;for patients with sigmoid cancer,the median survival time was 63.0 months〔95%CI(51.2,74.8)〕,and the survival rates of one year,two years and three years were 94.5%,87.2% and 79.3%.Patients with the three kinds of neoplasm were not significantly different in the survival curve(χ2=1.246,P=0.536).The median PFS for patients with recto-sigmoid neoplasm,rectal neoplasm and sigmoid neoplasm was 48.0 months〔95%CI(36.3,59.7)〕,29.0 months〔95%CI(17.9,40.1)〕 and 63.0 months〔95%CI(37.1,88.9)〕 respectively.Patients with the three kinds of neoplasm were significantly different in PFS survival curve(χ2=17.329,P=0.001).Cox regression analysis showed that the neoplasm site〔HR=0.585,95%CI(0.338,0.891),P=0.012〕 and depth of infiltration〔HR=3.516,95%CI(1.883,6.746),P=0.038〕 were independent predictive factors for PFS of patients with colorectal cancer.Conclusion There are no differences in survival time among patients with recto-sigmoid neoplasm,rectal neoplasm and sigmoid neoplasm,while differences exist in PFS.The depth of infiltration may be the influencing factor for PFS of patients with colorectal cancer.
Colonic neoplasms;Sigmoid neoplasms;Rectal neoplasms;Prognosis
050011河北省石家庄市,河北医科大学第四医院(孔雁,刘风玲,左静);保定市第三医院(徐建梅)
刘风玲,050011河北省石家庄市,河北医科大学第四医院;E-mail:329502837@qq.com
R 735.35
A
10.3969/j.issn.1007-9572.2015.23.009
2014-12-18;
2015-06-29)
孔雁,徐建梅,刘风玲,等.直乙肠交界处癌与直肠癌及乙状结肠癌的预后比较[J].中国全科医学,2015,18(23):2783-2786.[www.chinagp.net]
Kong Y,Xu JM,Liu FL,et al.Comparison of prognosis among recto-sigmoid cancer,rectal neoplasm and sigmoid neoplasm[J].Chinese General Practice,2015,18(23):2783-2786.
