人股骨头坏死标本不同区域骨小梁的显微结构特征及病理学表现
2014-10-09苟文隆徐小龙袁雪凌卢世璧
王 程,苟文隆,徐小龙,袁雪凌,彭 江,卢世璧
解放军总医院 骨科,北京 100853
人股骨头坏死标本不同区域骨小梁的显微结构特征及病理学表现
王 程,苟文隆,徐小龙,袁雪凌,彭 江,卢世璧
解放军总医院 骨科,北京 100853
目的对股骨头坏死标本不同区域的骨小梁进行量化分析。方法 收集我院2011 - 2013年非创伤性股骨头坏死病人行全髋关节置换术后的股骨头标本10个以及病人病历和临床影像学资料(男性6例,女性4例)。对标本进行显微CT断层扫描,根据图像结果将标本分为健康区、硬化区和坏死区,分别进行骨计量学分析。分析指标有骨矿密度(bone mineral density,BMD)、骨矿容量(bone mineral content,BMC)、骨表面积与骨骼体积比(bone surface to bone volume ratio,BS/BV);体积分数(bone volume fraction,BVF)、结构模型指数(structure model index,SMI)、骨小梁数目(trabecular plate number,Tb.N)、骨小梁厚度(trabecular plate thickness,Tb.Th)、骨小梁间隙(trabecular spacing,Tb.Sp)。扫描后将标本作病理学处理。结果晚期股骨头坏死区和硬化区的骨小梁空间结构明显改变。与健康区相比,硬化区骨小梁明显增厚,BVF显著增加,两组间BMD、Tb.Th、BMC、BS/BV差异有统计学意义(P<0.05),而Tb.Sp差异无统计学意义(P>0.05);与健康区相比,坏死区的BMD、BMC、BVF、Tb.N明显减少,Tb.Sp较硬化区显著增宽,两组差异有统计学意义(P<0.05),而Tb.Th、BS/BV差异无统计学意义(P>0.05)。结论晚期股骨头坏死标本坏死区的骨小梁连续性破坏,结构散乱;硬化区的骨小梁结构增厚,数目增多,间隙变窄;正常区域骨小梁结构完整,厚度分布均匀。
骨坏死;股骨头;显微CT
股骨头坏死(osteonecrosis of the femoral head,ONFH)是骨科常见的一种难治性疾病,好发于中青年,而且自然进展快,致残率高[1]。目前其病理机制不甚明了,一些学者认为股骨头坏死是由于股骨头血运受阻,导致股骨头内骨细胞坏死,修复模式启动之后,股骨头力学强度减低,最终导致股骨头空间结构改变,塌陷。但是股骨头力学强度减低的程度与股骨头修复的范围和修复能力大小之间的关系尚不明确,因此有必要研究股骨头内部骨小梁的结构改变和股骨头塌陷的方式。本研究通过Micro-CT重现塌陷股骨头骨小梁的三维空间结构,探讨股骨头坏死塌陷的可能方式。
材料和方法
1 标本及资料 收集我院2011 - 2013年非创伤性股骨头骨坏死病人行全髋关节置换术后的股骨头标本10个(男6例,女4例,FicatⅣ期)以及病人病历和临床影像学资料。
2 仪器设备 Micro-CT(Locus SP GE公司美国),硬组织切片机(IsoMet® 5000 BUEHLER公司美国),包埋机 (Cast n’ Vac 1000 BUEHLER 公司美国 ),磨片机(MetaServ® BUEHLER公司美国)
3 Micro-CT扫描 将10个股骨头标本分别置于Micro-CT系统中进行扫描,扫描分辨率为45 μm×45 μm×45 μm,单次扫描时间为14 min。确定坏死区、硬化区、健康区的位置并且在每个区域分别选取3个长方体信息区进行重建(0.5 cm×0.5 cm×1 cm)。
4 不同区域骨微结构及矿物含量评价 采用Micro-CT自带软件GE Microview进行图像处理,对股骨头坏死不同区域进行三维重建以及骨计量学分析;计算以下骨矿物质参数:骨矿密度(bone mineral density,BMD),骨矿容量(bone mineral content,BMC),骨表面积与骨骼体积比(bone surface to bone volume ratio,BS/BV),体积分数(bone volume fraction,BVF),骨矿化含量(bone mineral content,BMC),结构模型指数 (structure model index,SMI),骨小梁数目 (trabecular plate number,Tb.N),骨小梁厚度(trabecular plate thickness,Tb.Th),骨小梁间隙(trabecular spacing,Tb.Sp)。
5 病理学观察 标本扫描之后,经75%、85%、95%、100%的酒精逐级脱水,二甲苯透明,树脂包埋切片,HE以及Masson染色后观察。
6 统计学分析 使用SPSS17.0统计软件,所有数据均以的形式表示。组间数据比较采用单因素方差分析,P<0.05为差异有统计学意义。
结 果
1 Micro-CT图像特征 股骨头坏死标本的三个区域(坏死区、硬化区和健康区)的骨小梁排列特征明显不同,坏死区的骨小梁断裂破碎,连续性破坏,结构较为散乱;硬化区的骨小梁结构增厚,数目增多,间隙变窄;正常区域骨小梁结构正常,厚度分布均匀。见图1。
2 骨计量学 不同区域骨小梁的计量学参数明显不同。与健康区域相比,硬化区骨小梁明显增厚,BVF增加200%,小梁厚度和数目明显增加,两组间差异有统计学意义(P<0.05),而Tb.Sp两组之间差异无统计学意义(P>0.05);与健康区相比,坏死区的BMD、BMC、BVF、Tb.N明显减少,Tb.Sp显著增宽,两组间差异有统计学意义(P<0.05),Tb.Th、BS/BV差异无统计学意义(P>0.05)。见表1。
表1 股骨头骨坏死样本不同区域骨计量学分析Tab. 1 Histomorphometry for necrosis of the femoral head in different regions (, n=10)
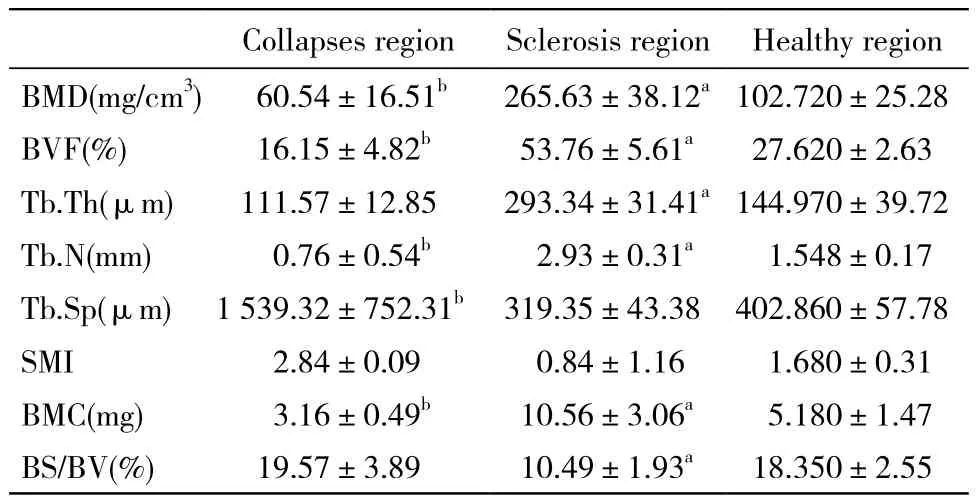
表1 股骨头骨坏死样本不同区域骨计量学分析Tab. 1 Histomorphometry for necrosis of the femoral head in different regions (, n=10)
aP<0.05, bP<0.05, vs healthy region
Collapses region Sclerosis region Healthy region BMD(mg/cm3) 60.54±16.51b 265.63±38.12a102.720±25.28 BVF(%) 16.15±4.82b 53.76±5.61a 27.620±2.63 Tb.Th(μm) 111.57±12.85 293.34±31.41a144.970±39.72 Tb.N(mm) 0.76±0.54b 2.93±0.31a 1.548±0.17 Tb.Sp(μm) 1 539.32±752.31b 319.35±43.38 402.860±57.78 SMI 2.84±0.09 0.84±1.16 1.680±0.31 BMC(mg) 3.16±0.49b 10.56±3.06a 5.180±1.47 BS/BV(%) 19.57±3.89 10.49±1.93a 18.350±2.55

Fig. 1 Micro-CT image showing two-dimensional reconstruction(A) in necrosed region (B), sclerotic region (C), and healthy region (D) of femoral head
3 病理表现 坏死区可见股骨头明显塌陷变形,软骨下骨结构基本消失,甚至有关节软骨分离等改变。坏死灶呈暗红色、不规则、与周围组织分界清楚,骨小梁坏死,骨组织被其他性质的病理组织取代。硬化区可见骨小梁增生,排列规则致密,硬化区有大量炎性细胞(淋巴细胞、单核细胞、肥大细胞、浆细胞)浸润。并伴有多种组织增生,包括结缔组织、新生血管等,形成一个显微组织修复区。见图2。

图 2 股骨头坏死标本,根据骨密度的不同分为坏死区(a),硬化区(b),健康区(c) A: HE染色; B: Masson染色Fig. 2 HE staining (A) and Masson staining (B) showing bone mineral density in necrosed region (a), sclerotic region (b)and healthy region (c) of femoral head
讨 论
股骨头坏死主要表现为骨结构的连续性破坏和骨小梁的断裂,其原因是因为载荷压力持续作用,导致缺血区骨无法及时修复,而股骨头具有承载载荷压力的作用,是承载人体负荷的重要部位[2-5]。股骨头的塌陷是骨小梁结构连续性变化的结果,股骨头坏死的生物应力不仅降低了骨矿物质密度,而且改变了骨小梁的空间排列以及立体结构,导致力学强度丧失,最终塌陷[6-7]。导致股骨头坏死的病因有很多,包括酒精、激素、创伤等,其发病机制还不太明确,大量研究表明成骨、破骨细胞的活性变化在其发生发展过程中起到关键的作用[8-10]。Micro-CT是一种非侵入性的检测方式,能以非常高的分辨率对活体或者离体标本进行检测,同时不破坏检测对象的内部结构,其在检测股骨头坏死标本时对骨小梁有很强的敏感性[11-12]。Feldkamp等[13]早在20世纪80年代就应用Micro-CT对骨小梁的微观结构进行了检测评价,并报道了相关研究结果。Marinozzi等[14]也认为Micro-CT是精确测量离体股骨头标本骨形态计量学的方法。本实验经研究发现,与健康区比较,坏死区股骨头骨小梁厚度及密度改变,骨小梁厚度不均,排列紊乱,多处的骨小梁骨折,股骨头高度变低,股骨头内骨密度分布不均,显示存在骨修复重建过程。大量研究表明,在骨坏死发生前期,修复反应也随之启动,成骨及破骨活动均增强,但后者更为活跃,由于坏死骨的吸收作用,使骨小梁的三维支撑结构破坏。新生的骨小梁排列紊乱,其力学支撑作用较差,在正常应力情况下就会出现微骨折,最终导致股骨头塌陷[15-18]。在骨计量学方面,股骨头坏死区骨小梁的BMD、BMC、BVF、Tb.N均降低,骨量显著降低。硬化区骨小梁BVF明显增加,Tb.Sp变窄,骨小梁增厚,结构发生显著变化。理想的杆状骨小梁和板状骨小梁的SMI数值分别为3和0,而本实验中坏死区与健康区骨小梁的SMI分别为2.84和1.68,可以看出在发生骨坏死时,SMI数值增加,骨小梁从板状向杆状的状态转变,硬化区骨小梁SMI出现负值,表示骨体积分数过大,骨小梁数目增多。另外,本实验仅从不同区域骨小梁的结构与骨密度改变推测股骨头的力学状态改变,下一步我们将结合生物力学测试检验我们的观点,通过分析骨小梁微观结构和应力分布的关系,探索股骨头坏死塌陷机制,为股骨头坏死的治疗及康复提供新的指导思想和研究方向。
1 Gagala J, Buraczynska M, Mazurkiewicz T, et al. Prevalence of genetic risk factors related with thrombophilia and hypofibrinolysis in patients with osteonecrosis of the femoral head in Poland[J]. BMC Musculoskelet Disord, 2013, 14 : 264.
2 Séguin C, Kassis J, Busque L, et al. Non-traumatic necrosis of bone (osteonecrosis) is associated with endothelial cell activation but not thrombophilia[J]. Rheumatology, 2008, 47(8): 1151-1155.
3 Kaushik AP, Das A, Cui Q. Osteonecrosis of the femoral head : An update in year 2012[J]. World J Orthop, 2012, 3(5): 49-57.
4 Amanatullah DF, Strauss EJ, Di Cesare PE. Current management options for osteonecrosis of the femoral head : part 1, diagnosis and nonoperative management[J]. Am J Orthop (Belle Mead NJ),2011, 40(9): E186-E192.
5 Amanatullah DF, Strauss EJ, Di Cesare PE. Current management options for osteonecrosis of the femoral head : part II, operative management[J]. Am J Orthop (Belle Mead NJ), 2011, 40(10):E216-E225.
6 Sakai T, Sugano N, Nishii T, et al. Extent of osteonecrosis on MRI predicts humeral head collapse[J]. Clin Orthop Relat Res, 2008,466(5): 1074-1080.
7 Schmitt-Sody M, Kirchhoff C, Mayer W, et al. Avascular necrosis of the femoral head: inter- and intraobserver variations of Ficat and ARCO classifications[J]. Int Orthop, 2008, 32(3): 283-287.
8 Fan M, Jiang WX, Wang AY, et al. Effect and mechanism of zoledronate on prevention of collapse in osteonecrosis of the femoral head[J]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao, 2012, 34(4):330-336.
9 Tortelli F, Pujic N, Liu Y, et al. Osteoblast and osteoclast differentiation in an in vitro three-dimensional model of bone[J].Tissue Eng Part A, 2009, 15(9): 2373-2383.
10 Shabtai L, Drexler M, Blummberg N. Biphosphonate in the treatment of avascular necrosis of the femoral head[J]. Harefuah, 2012, 151(4):242-245.
11 Hambli R. Micro-CT finite element model and experimental validation of trabecular bone damage and fracture[J]. Bone, 2013, 56(2):363-374.
12 Hsu JT, Wang SP, Huang HL, et al. The assessment of trabecular bone parameters and cortical bone strength: a comparison of micro-CT and dental cone-beam CT[J]. J Biomech, 2013, 46(15):2611-2618.
13 Feldkamp LA, Goldstein SA, Parfitt AM, et al. The direct examination of three-dimensional bone architecture in vitro by computed tomography[J]. J Bone Miner Res, 1989, 4(1): 3-11.
14 Marinozzi F, Bini F, Marinozzi A, et al. Technique for bone volume measurement from human femur head samples by classification of micro-CT image histograms [J] . Ann Ist Super Sanita, 2013, 49(3): 300-305.
15 Qin L, Zhang G, Sheng H, et al. Multiple bioimaging modalities in evaluation of an experimental osteonecrosis induced by a combination of lipopolysaccharide and methylprednisolone[J]. Bone, 2006, 39(4): 863-871.
16 Zhang G, Sheng H, He YX, et al. Continuous occurrence of both insufficient neovascularization and elevated vascular permeability in rabbit proximal femur during inadequate repair of steroid-associated osteonecrotic lesions[J]. Arthritis Rheum, 2009, 60(10):2966-2977.
17 Hasan SS, Romeo AA. Nontraumatic osteonecrosis of the humeral head[J]. J Shoulder Elbow Surg, 2002, 11(3): 281-298.
18 Ha YC, Kim HJ, Kim SY, et al. Effects of age and body mass index on the results of transtrochanteric rotational osteotomy for femoral head osteonecrosis: surgical technique[J]. J Bone Joint Surg Am,2011, 93(Suppl 1): 75-84.
Microstructure features and pathology of trabecula in different regions of femoral head necrosis
WANG Cheng, GOU Wen-long, XU Xiao-long, YUAN Xue-ling, PENG Jiang, LU Shi-bi
Department of Orthopedics, Chinese PLA General Hospital, Beijing 100853, China
Corresponding author: PENG Jiang. Email: pengjiang301@126.com
ObjectiveTo analyze the microstructure of trabecula in different regions of femoral head necrosis.MethodsClinical and imaging data about 10 patients (6 males and 4 females) with non-traumatic femoral head necrosis who underwent total hip arthroplasty in our hospital from 2011 to 2013 were retrospectively analyzed. Samples were taken from the healthy, sclerotic and necrosed regions of the patients. The following parameters were analyzed, including the bone mineral density (BMD), bone mineral content (BMC), bone surface/ bone volume (BS/BV) ratio, bone volume fraction(BVF), structure model index (SMI), number of trabecular plates, thickness of trabecular plate, and trabecular space. Results The spatial structure of trabecula was signi fi cantly changed in necrosed and sclerotic regions of femoral head. The trabecula was signi fi cantly thicker and the BVF was signi fi cantly higher in necrosed region than in healthy region (P<0.05). No significant difference was found in the BMD, the number of trabecular plates, the thickness of trabecular plate, and the BS/BV ratio between the two groups (P>0.05). The BMD and BMC,the BVF, and the thickness of trabecular plate were signi fi cantly lower while the trabecular space was signi fi cantly wider in necrosed region than in healthy region (P<0.05). No signi fi cant difference was found in the thickness of trabecular plate and the BS/BV ratio between the two groups (P>0.05).ConclusionThe spatial structure and pathological features of trabecula are different in different necrosis regions of femoral head. The continuity of trabecula in necrosed region is disrupted, with its structure disarranged and thickened, the number of trabecular plates increased, and the trabecular space narrowed. However, the structure of trabecula is intact and its thickness is even in the healthy region.
osteonecrosis; femur head; Micro-CT
R 681.22
A
2095-5227(2014)05-0463-04
10.3969/j.issn.2095-5227.2014.05.018
时间:2014-03-07 11:05
http://www.cnki.net/kcms/detail/11.3275.R.20140307.1105.002.html
2013-11-04
国家自然科学基金项目(30930092);国家“863”计划项目(2012AA020502)
Supported by the National Natural Science Foundation of China(30930092);"863" Program of China(2012AA020502)
王程,男,在读硕士。研究方向:骨坏死。Email: wang chengchina301@163.com
彭江,男,副主任医师,教授,硕士生导师。Email: pe ngjiang301@126.com
