肩关节前脱位的诊治体会
2014-07-05曹烈虎章浩张春才翁蔚宗李海航宋绍军纪方苏佳灿
曹烈虎 章浩 张春才 翁蔚宗 李海航 宋绍军 纪方 苏佳灿
肩关节前脱位的诊治体会
曹烈虎 章浩 张春才 翁蔚宗 李海航 宋绍军 纪方 苏佳灿
目的探讨肩关节前脱位手法复位前的伤情评估及相关并发症的防治。方法回顾性分析肩关节脱位患者56例,其中男性31例,女性25例。喙突下脱位31例,盂下脱位20例,锁骨下脱位5例,伴有肱骨大结节骨折15例,肱骨头骨折1例,腋神经损伤3例,医源性肱骨近端骨折2例。结果所有患者在急诊室试行Hippocrates法进行手法复位,48例手法复位成功,8例手法复位失败,其中1例伴有肱骨大结节患者在手术室全麻手法复位,2例臂丛麻醉下手法复位,4例行切开复位,1例肱骨头骨折卡压者行切开复位。结论肩关节脱位手法复位前应对伤情进行充分的评估,要认真分析影像资料,进行准确的手法复位。若手法失败,避免造成医源性损伤,应进行进一步的影像检查,必要时在臂丛或全麻下复位,甚至切开复位,并对相关的并发症进行准确的判断,减少医源性损伤的发生。
肩关节脱位; 手法复位; 医源性损伤; 切开复位
肩关节脱位是较为常见的肩关节损伤,占所有关节脱位的50%左右。其中,肩关节前脱位占96%[1],后脱位较为少见。肩关节前脱位在急诊室中大部分通过手法得到复位,但一些患者常合并大结节骨折、肱骨头骨折、肩袖损伤、神经损伤、腋动脉损伤等并发症。如果伤情未正确判断,手法复位粗暴,则会加重原来的损伤,不仅导致医源性肱骨近端骨折、神经血管损伤,还会导致不必要的医疗纠纷[23]。因此,我们必须对所有肩关节脱位患者进行正确的评估和判断,有效地进行手法复位。初次手法复位失败的患者需要进手术室麻醉复位,甚至需要切开复位。第二军医大学附属长海医院骨科自2012年8月至2013年10月急诊治疗56例患者,诊治情况报道如下。
资料与方法
一、一般资料
本组肩关节脱位患者56例,其中男性31例,女性25例;年龄23~85岁,平均年龄36.5岁;车祸外伤10例,摔伤32例,坠落伤8例,运动伤6例。伤后就诊时间为15min至8h,平均1.6h,均为新鲜、外伤性脱位。其中,喙突下脱位31例,盂下脱位20例,锁骨下脱位5例,伴有肱骨大结节骨折15例,肱骨头骨折1例,腋神经损伤3例,医源性肱骨近端骨折2例。
二、入选标准
明显外伤病史,就诊时患者患肢轻度外展内旋位,肘屈曲,用健侧手托住侧前臂,外观呈方肩畸形,肩峰明显突出,剑峰下空虚,在腋下、喙突下、锁骨下能摸到肱骨头,通过X线(正位加穿胸位)确诊为肩关节前脱位。
三、治疗方法
肩关节腔内注射1支利多卡因(100mg),约10min患者疼痛及情绪缓解后,按照Hippocrates法进行手法复位。
结 果
所有患者在急诊室试行Hippocrates法进行手法复位,48例手法复位成功,8例手法复位失败,其中1例伴有肱骨大结节患者在手术室全麻复位,2例臂丛麻醉下手法复位,4例行切开复位,1例肱骨头骨折卡压者行切开复位。
典型病例1:患者女性,82岁,摔伤导致右肩关节脱位。来我院之前在2家医院试行手法复位失败,到我院急诊科就诊,复查X线片提示右肩关节盂下脱位。我院急诊医师再次行手法复位失败,请上级医师会诊,行肩关节CT检查,提示右肱骨头骨折卡压。急诊在臂丛麻醉下行手术切开予以复位,详见图1。
典型病例2:患者男性,78岁,摔伤致左肩关节脱位伴大结节骨折(盂下脱位),臂丛神经损伤。在急诊科多次手法复位失败,收住入院,行三维CT检查提示肱骨大结节卡压在关节盂,诊断进一步明确后行切开复位内固定术,详见图2。

图1 患者,女性,82岁,摔伤导致右肩关节脱位 图A为术前X线片;图B为术前CT;图C为术后即刻X线片
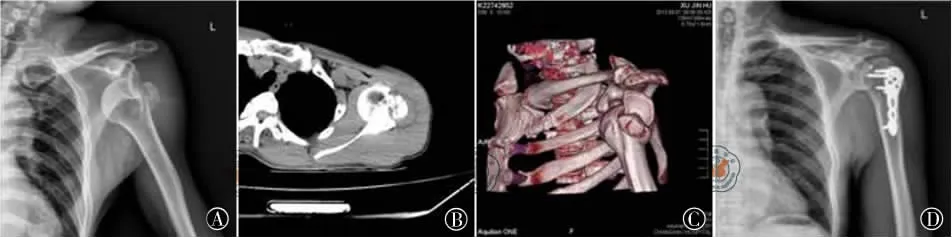
图2 患者,男性,78岁,摔伤致左肩关节脱位伴大结节骨折(盂下脱位),臂丛神经损伤 图A为术前X线片;图B为术前CT;图C为术前三维CT;图D为术后X线片
典型病例3:患者女性,34岁,由摔伤导致的左肱骨大结节骨折伴肩关节脱位。外院给予手法复位肩周带固定保守治疗,3周后患者因左上臂外展功能明显受限来我院就诊。行左肩关节MRI检查提示:左肩袖岗上肌腱损伤,我院给予行微创铆钉修复肩袖损伤+空心钉固定术,手术1个月后左臂外展功能明显恢复,详见图3。

图3 患者,女性,34岁,摔伤导致的左肱骨大结节骨折伴肩关节脱位 图A为术前X线片;图B为术前MRI提示:肩袖损伤;图C为术后X线片;图D为术后功能照
讨 论
肩关节脱位在骨科急诊较为常见,通过Hippocrates法大部分患者可顺利复位[4]。多数医师在肩关节脱位手法复位中积累了一定的经验,因此常常盲目相信自己,在没有认真阅读影像资料的情况下常徒手复位。一人复位不行,借助多人帮助暴力复位,常常造成医源性损伤的发生,导致医疗纠纷。采用多人复位,容易出现用力不均,出现应力点错移而导致复位失败,甚至出现应力点的骨折。而应力点最经常出现的就是解剖颈处,所以肩关节脱位出现整复性骨折者常为解剖颈骨折。笔者认为,对于青壮年或体力劳动者,因上肢肌肉发达,在仔细阅片的情况下,一人无法复位的时候,可借助多人进行复位。但复位过程中因循序渐进,避免暴力,特别是对于老年人。当手法复位失败时,切忌暴力复位,高质量的X线片对骨科医师避免漏诊、误诊有很大的作用。遇到可疑情况,必须重新拍片或者行CT重建,及时调整治疗方案。另外,单纯徒手复位失败时,适当给予利多卡因局部麻醉,减轻患者的疼痛感和紧张心理,利于手法复位。Tamaoki等[5]通过随机对照研究证实,对肩关节脱位手法复位给予局麻药患者在疼痛减轻、复位时间、引发并发症方面明显优于对照组。
肩关节脱位手法复位最常用的方法为Hippocrate法。由于此方法易出现并发症、患者耐受差等原因,专家们正探索更多的复位方法,如Kocher法、牵拉-反牵拉法、Stimson法、Eskimo法[6]。O′Connor等[7]对12例伴肱骨大结节骨折患者采用Milch法复位,不仅肩关节脱位全部成功复位,且复位后12例患者大结节骨折移位均<5mm,认为Milch法是现场急救和急诊室人力紧张时的理想方法。采用肩胛骨复位法,也可成功复位肩关节脱位口,但由于采用被动俯卧位,对需要采用臂丛或全麻的患者不宜使用(备注:因为此复位法是俯卧位,如打臂丛或全麻麻醉的话,通过仰卧位Hippocrate法就可解决,不需要采用肩胛骨复位法)。此外,对于肩胛骨较难触摸的肥胖患者也不宜使用。肩关节外旋法是相对新的方法,Eachempati等[8]强调对合并大结节骨折的患者,复位前予以麻醉。Sayegh等[9]提出的快速、可靠、安全的FARES(fast,reliable,and safe)法通过牵引和垂直震荡运动复位肩关节脱位。通过对155例肩关节脱位合并或不合并大结节骨折患者随机采用FARES法、Hippocratic法或Kocher法复位,认为FARES法是快速、有效、少痛的复位方法。Maity等[10]采用前瞻性随机临床对比研究,对FARES法和Eachempati外旋复位法进行比较,发现FARES法复位成功率为95%,Eachempati外旋复位法为91.25%。但在复位的速度、复位过程中的疼痛程度以及尝试复位的次数上FARES法显著优于Eachempati外旋复位法,推荐FARES法为复位肩关节脱位的首选方法。
肩关节脱位并发症较多,常合并肱骨大结节骨折、肱骨头骨折、肩袖损伤、腋神经损伤、臂丛神经损伤、腋动脉损伤等。其中肩关节脱位合并大结节骨折的发生率为15%~30%[11]。当大结节移位>5mm或者从事上臂过度运动的运动员、重体力劳动者移位>3mm者需进行手术治疗[12]。肱骨头骨折首次在1940年被Hill和Sachs报道,又称为Hill-Sachs损伤,大约为肩关节脱位发生率的40%~90%,是引起关节脱位的重要原因[13]。小的缺损不影响肩关节稳定性时可选择保守治疗,大的缺损需要行关节镜和切开治疗[14]。肩关节脱位几乎合并肩袖损伤,由于脱位复位后上肢制动而不能在早期发现,因此晚期出现上肢外展无力、肩关节反复疼痛时,可考虑肩袖损伤,及时行关节镜或开放手法探查修复肩袖损伤[15]。肩关节脱位是腋神经损伤的常见原因。由肩关节脱位引起的腋神经损伤为神经牵拉伤,损伤常位于四边孔间隙[16]。肩关节复位后,腋神经损伤可先行保守治疗,如保守治疗无效,经临床及肌电图检查无恢复表现,应及时手术探查。臂丛神经损伤往往是肩关节脱位牵拉损伤引起,临床上比较少见,保守治疗为主,年轻人比老年人恢复的快[17]。当肩关节脱位出现上肢血肿、苍白、脉搏减弱、麻痹、体温降低时就要高度怀疑腋动脉损伤,即刻行动脉造影检查,及时手术探查[18]。
总之,肩关节脱位手法复位前应对伤情进行充分评估,要认真分析影像资料,进行准确的手法复位,并对相关的并发症进行准确的判断。当手法复位失败时,应进行进一步的影像学检查,在麻醉下或切开复位,切忌盲目自信,避免医源性损伤的发生。因此,当面对肩关节脱位患者,特别是多次手法复位失败的复杂患者,一定要考虑相关上述并发症的发生,如合并肱骨大结节骨折、肱骨头骨折、肩袖损伤、腋神经损伤,臂丛神经损伤、腋动脉损伤等,避免漏诊、误诊的情况发生。
[1] Tamaoki MJ,Faloppa F,Wajnsztejn A,et al.Effectiveness of intra-articular lidocaine injection for reduction of anterior shoulder dislocation:randomized clinical trial[J].Sao Paulo Med J,2012,130(6):367-372.
[2] 严红勇,霍森.足蹬法治疗肩关节脱位致医源性肱骨解剖颈骨折4例[J].中国骨伤,2012,25(8):696-697.
[3] 苏士乐,刘浩,章宏志,等.肩关节脱位医源性并发症失误分析[J].中国矫形外科杂志,2009,(18):1433-1434.
[4] Sahin N,Oztürk A,Ozlan Y,et al.A comparison of thescapular manipulation and Kocher s technique for acute anterior dislocation of the shoulder[J].Eklem Hastalik Cerrahisi,2011,22(1):28-32.
[5] Tamaoki MJ,Faloppa F,Wajnsztejn A,et al.Effectiveness of intra-articular lidocaine injection for reduction of anterior shoulder dislocation:randomized clinical trial[J].Sao Paulo Med J,2012,130(6):367-372.
[6] Hovelius L,Olofsson A,Sandstrm B,et al.Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger.a prospective twenty-five-year follow-up[J].J Bone Joint Surg Am,2008,90(5):945-952.
[7] O'Connor DR,Schwarze D,Fragomen AT,et al.Painless reduction of acute anterior shoulder dislocations without anesthesia[J].Orthopedics,2006,29(6):528-532.
[8] Eachempati KK,Dua A,Malhotra R,et al.The external rotation method for reduction of acute anterior dislocations and fracture-dislocations of the shoulder[J].J Bone Joint Surg Am,2004,86(11):2431-2434.
[9] Sayegh FE,Kenanidis EI,Papavasiliou KA,et al.Reduction of acute anterior dislocations:aprospective randomized study comparing a new technique with the Hippocratic and Kocher methods[J].J Bone Joint Surg Am,2009,91(12):2775-2782.
[10] Maity A,Roy DS,Mondal BC.A prospective randomised clinical trial comparing FARES method with the Eachempati external rotation method for reduction of acute anterior dislocation of shoulder[J].Injury,2012,43(7):1066-1070.
[11] Dimakopoulos P,Panugopoulos A,Kasimatis G,et al.Anlerior traumatic shoulder dislocation associated with displaced greater tuberosity fracture:the necessity of operative treatment[J].J Orthop Trauma,2007,21(2):104-112.
[12] Gruson KI.Ruchelsman DE,Tejwani NC.Isolated tuberosity fractures of the proximal humeral:current concepts[J].Injury,2008,39(3):284-298.
[13] Calandra JJ,Baker CL,Uribe J.The incidence of Hill-Sachs lesions in initial anterior shoulder dislocations [J].Arthroscopy,1989,5(4):254-257.
[14] Provencher MT,Frank RM,Leclere LE,et al.The Hill-Sachs lesion:diagnosis,classification,and management[J].J Am Acad Orthop Surg,2012,20(4):242-252.
[15] Gomberawalla MM,Sekiya JK.Rotator Cuff Tear and Glenohumeral Instability:A Systematic Review [J].Clin Orthop Relat Res,2013.[Epub ahead of print]
[16] Zhao X,Hung LK,Zhang GM,et al.Applied anatomy of the axillary nerve for selective neurotization ofthe deltoid muscle[J].Clin Orthop Relat Res,2001,390:244-251.
[17] Kosiyatrakul A,Jitprapaikulsarn S,Durand S,et al.Recovery of brachial plexus injury after shoulder dislocation[J].Injury,2009,40(12):1327-1329.
The diagnosis and treatment of anterior shoulder dislocations
Cao Liehu,Zhang Hao,Zhang Chuncai,Wong Weizong,Li Haihang,Song Shaojun,Ji Fang,Su Jiacan.Department of Orthopedics,Changhai Hospital Affiliated to Second Military Medical University,Shanghai 200433,China
ObjectiveTo explore the injury assessment and the control measure for the related complication before the manual reduction of anterior shoulder dislocations.MethodsGeneral data:56 patients suffered anterior shoulder dislocations were retrospectively analyzed in our study.31were male and 25were female,and their ages ranged from 23to 85years old with the mean age of 36.5years old.10patients got injured at car accidents.32injuries resulted from falling,8of which fell from the height,and 6were injured in sports.The time before going to hospital ranged from 15minutes to 8 hours with a mean time of 1.6hours.All of the shoulder dislocations were fresh and traumatic.For the dislocation direction,31were subcoracoid dislocations,20were subglenoid dislocations,and 5were subclavicle dislocations,15patients were associated with fractures of greater tuberosity,1humeral head fracture,and 3axillary nerve injuries,2Iatrogenic proximal humeral fractures.Inclusion criteria:Patients had a clear history of shoulder trauma.The squared shoulder deformation was showed by physical examination,and the humeral head could be touched in the axillary,subcoracoid,or subclavicle.The shoulder dislocation was also confirmed by the radiographic diagnosis.Treatment:100 mg lidocaine was injected into the shoulder joint,and then the dislocations were reduced using the Hippocrates method after about 10minutes when the pain was relieved.ResultsAll the patients
closed reduction by the Hippocrates method in the emergency room.48patients had successful reduction,8patients failed.Of these 8cases,closed reduction succeeded in one case with the fracture of greater tuberosity at the operation room with general anesthesia,manual reduction was done in 2cases with brachial plexus block,and open reduction was done in one case with humeral head fracture.ConclusionsA series of careful assessment should be done before gimmick reset of the anterior shoulder dislocation,including the analysis of the image data.If the gimmick reset failed,to avoid the violent iatrogenic damage,further image examination need be done,and the reduction need to be done with general anesthesia of brachial plexus anesthesia when necessary.The accurate judgment of complications was needed to reduce the occurrence of iatrogenic injury.
Shoulder dislocation; Manual reduction; Iatrogenic damage; Open reduction
Su Jiacan,Email:drsujiacan@163.com
2013-11-30)
(本文编辑:胡桂英)
10.3877/cma.j.issn.2095-5790.2014.01.008
200433 上海,第二军医大学附属长海医院骨科
苏佳灿,Email:drsujiacan@163.com
曹烈虎,章浩,翁蔚宗,等.肩关节前脱位的诊治体会[J/CD].中华肩肘外科电子杂志,2014,2(1):41-44.