Quality management in general surgery: a review of the literature
2014-03-22MirceaBeuranIonutNegoiSorinPaunMihaelaVarticBogdanStoicaIoannaseRuxandraIrinaNegoiSorinHostiuc
Mircea Beuran, Ionut Negoi, Sorin Paun, Mihaela Vartic, Bogdan Stoica, Ioan Tănase, Ruxandra Irina Negoi, Sorin Hostiuc
1Carol Davila University of Medicine and Pharmacy Bucharest, Romania
2Emergency Hospital of Bucharest, Romania
3Embriology Department, University of Medicine and Pharmacy Carol Davila Bucharest, Romania
4National Institute of Legal Medicine Mina Minovici, Bucharest Romania
Quality management in general surgery: a review of the literature
Mircea Beuran1,2, Ionut Negoi1,2, Sorin Paun1,2, Mihaela Vartic2, Bogdan Stoica2, Ioan Tănase2, Ruxandra Irina Negoi1,3*, Sorin Hostiuc1,4
1Carol Davila University of Medicine and Pharmacy Bucharest, Romania
2Emergency Hospital of Bucharest, Romania
3Embriology Department, University of Medicine and Pharmacy Carol Davila Bucharest, Romania
4National Institute of Legal Medicine Mina Minovici, Bucharest Romania
Introduction: Total quality management is a systematic approach focused on satisfying customers’ expectations, identifying problems, analytically solving patient’s problems and to implement continuous quality improvement. Method: Systematic review of the English language medical literature, using electronic search of the Pubmed, ProQuest and ScienceDirect databases with different combinations of the keywords: total quality management, healthcare, trauma, and minimally invasive surgery. Results: The assessment of outcomes in surgery represents a part of the quality assurance of patients’ care. Usually, the surgeons have their own set of mental variables that can predict good and bad outcomes Surveys of complication rates and outcome are a poor substitute for quality control. For the reported complications it is impossible to know which complications are real (inherent to surgery and unavoidable) and which are a consequence of a mistake or an error in judgment. For polytrauma patients, optimal outcome requires an initial management fulfilling a high standard of quality assurance. A prerequisite is the availability of adequate resources at all times, including personnel, technical equipment, and special designed emergency room. Conclusions: Romanian hospitals need a more aggressive implementation of total quality management policy, in order to maintain their competitiveness on nowadays European Union competitive market.
ARTICLE INFO
Article history:
Received 3 January 2015
Received in revised form 5 January 2015
Accepted 10 January 2015
Available online 20 January 2015
Quality management
1. Introduction
Total quality management, a concept developed by Edwards Deming, has been used successfully in the healthcare systems of many countries, and in many organizations for improving the quality of processes. The system is based upon the scientific method and provides the ability to solve longstanding, recalcitrating problems. The most widely used definition is “Quality is meeting or exceeding customer expectations”[1]. In the medical literature, the medical teams usually met resistance to behavioral changes and a lack of full support from upper level administrators, but most of them have been quite successful in improving the quality management process[2].
A snapshop in the quality of the healthcare in the United States is showing[3]: (i) In 2003, US Healthcare expenditures totaled $1.679 trillion. (ii) In 2003, the United States spent more on healthcare than did any other country in the world, but out of 30 OECD countries, the US ranked 22nd in male life expectancy and 23rd in female life expectancy and 26th in infant mortality rate. (iii) 55% are dissatisfied with the quality of healthcare in the US. (iv) Adult Americans received 54.9% of recommended preventive care, acute care and chronic care. (v) 44.000-98.000 deaths/year in the US arepreventable medical errors, representing the eighth leading cause of death, causing more deaths than motor vehicle accidents, breast cancer or AIDS. The estimated medical cost for these medical errors is $37.6-$50 billion annually.
Even if most common medical errors are considered to be improper dosage of medication or surgical errors (i.e. Incorrect site amputation), there are many other types, including: diagnostic errors including misdiagnoses leading to an incorrect choice of therapy, failure to use an indicated diagnostic test, failure to properly act on abnormal test results, equipment failures (i.e. a defibrillator without batteries, inadvertent dosing of medication due to intravenous pumps with dislodged valves), infections (i.e. nosocomial and surgical site infections), death due to seclusion or use of restraints. One of the main methods, according to the Institute of Medicine, used to prevent these errors is the use of medical informatics[4].
The research evidence showed that 4% of hospital patients suffer an avoidable injury, 7% experience a medication error, and 45% experience some medical mismanagement. 8% of anaesthetic errors were found to be human error and 92% due to system errors[5].
Nowadays, advances in medical research occur very rapidly, often overpassing our ability to translate new information into the clinical arena[6]. There is a great need to apply new knowledge efficiently and accurately to clinical practice. This is best done by carefully controlled clinical trials[7].
The assessment of outcomes in surgery represents a part of the quality assurance of patients’ care. Usually, the surgeons have their own set of mental variables that can predict good and bad outcomes[8].
It is very difficult to measure the quality of care in surgical practice, knowing that mortality, morbidity and length of inhospital stay are far from perfect in evaluating the standard of quality. Classically, the outcome in surgery has been described by the “five D”: death, disability, dissatisfaction, disease and discomfort[8].
There are two mathematical outcome predictor models: (i) In Europe-POSSUM (Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity). (ii) In United States-NSQIP (National Surgical Improvement Program).
For evaluation of healthcare performance were used hundreds of measures, that can be grouped in three main categories[9]: (i) Structure measures: data describing organizational facilities, environment, equipment, policies, and procedures. (ii) Process measures: data describing the delivery of healthcare services. (iii) Outcome measures: data describing the results of healthcare services.
For example, if the manager of the hospital wants to measure each characteristic of the antibiotic prophylaxis in the trauma department, he could ask the following questions: (i) Structure: Are there a sufficient number of medical personnel to cover 24/24 hours medical assistance in the trauma department? (ii) Process: Do the medical personnel a documented clinical exam of the traumatic wound immediate after patient arrival? (iii) Outcome: What is rate of infected wound necessitating special care due to local infection?
In recent years the healthcare systems throughout the world have changed dramatically, in Europe under the framework of European Foundation for Quality Management Excellence Model, a structure founded in 1988, launching its Model in 1991[10]: (i) The person coming for a medical service is no longer seen as a patient but rather as customer or client. (ii) Healthcare providers operate more and more in a free market system. (iii) For the financial aspects, the covering budgets of the hospitals have moved to prospective plans. (iv) The remuneration has changed in a payment per case.
The quality of care and services provided for patients have become a first priority in various countries such as Israel, Scotland and Spain as well as a legal obligation in Germany[11].
Many hospitals worldwide implemented the ISO 9001 quality management system. The eight principles of ISO 9001 supporting its requirements are: customer focus, leadership, involvement of people, process approach, system approach to management, continuous improvement, factual approach to decision making, mutually beneficial supplier relationships[12]. According to the ISO standard you should[12]:
(i) Document what you do (“Say what you do”)
(ii) Establish a process for the service
(iii) Perform to your documentation (“Do what you say”)
(iv) Provide the service based on the process
(v) Record the results of your work (“Record information”)
(vi) Appropriately maintain all recorded information
(vii) Audit the documentation for effectiveness (“Audit effectiveness”)
(viii) Audit using the process approach
In 2000, investigating the need for introduction of quality management into Greek healthcare, Theodorakioglou et al. found the following recommendations as essential[13]:
(i) A clear, detailed and specific health policy at a central level.
(ii) Changing of the legislative framework for maintaining the hospitals public character but a managerial and administrative flexibility, and an efficient management of human resources.
(iii) Introduction of competent managers who will successfully contribute to a modern and specialized unitaryplan, which will clearly deficit the existing financial and economic situation of hospitals.
(iv) Evaluation of the real final product, and the allocation of available resources to hospitals, on the basis of their effectiveness, efficiency and the real population needs they aim to cover.
(v) Extended use of well-designed information systems.
(vi) The motivation of employees so that their productivity will be increased and the level of services provided by them will be improved.
2. Quality Management in Trauma Care
Optimal outcome in the treatment of polytrauma patients requires an initial management fulfilling a high standard of quality assurance[14]. A prerequisite is the availability of adequate resources at all times, including personnel, technical equipment, and special designed emergency room. Diagnostic measures and therapy for rapid management of the airway, breathing, circulation (including here massive transfusion and surgical hemostasis) have priority[15]. For maintenance and improvement in the quality of care is necessary a standardized documentation, regular analysis, and feedback from an internal quality management process as well as participation in an external audit such a National Registry[16,17].
The essential element of the quality management system implemented at the department of trauma surgery of the University of Essen were the establishment of (a) an adequate protocol for documentation, (b) 20 criteria for the assessment of treatment quality, (c) regular statistical analysis of treatment quality and (d) a quality circle comprising all medical specialties for data discussion[18]. The study revealed that the quality of the early therapy of severely injured patients was significantly improved by the implementation of a multidisciplinary quality management system: (a) significant reduction of time needed for basic radiological and sonographic check-up (from 24±12 min to 14±8 min), for cranial computed tomography in severe traumatic brain injury (from 45±22 min to 28±8 min), (b) the rate of delayed diagnosis remained low (4% to 5%), (c) time savings in transfusions (from 35±20 min to 20±4 min) and emergency operations (from 67±20 min to 48±4 min) in hemorrhagic shock, and craniotomies in severe traumatic brain injuries (from 77±41 min to 54±19 min), (d) decrease in overall mortality (from 17% to 10%)[18].
Santana et al. described the quality indicators that trauma centers use for quality measurement and performance improvement[19]. They surveyed 330 trauma centers from United States, Canada, Australia and New Zealand, obtaining 10 587 quality indicators from 262 centers, of which 1 102 were unique indicators. These quality indicators assessed the safety (49%), effectiveness (32%), efficiency (27%) and timeliness (22%) of hospital process (64%) and outcomes (24%).
Due to growing evidence that for many treatments exist a relationship between the provider volume and patient outcomes, Stelfox et al. evaluated whether a relationship exists between trauma center volume and the nature of quality improvement programs[20]. They surveyed 154 verified adult trauma centers from United States, Canaada, Australia and New Zealand (76% response rate). Low-volume centers used more the quality indicators for evaluating triage and patient flow (18% vs. 13%, P<0.001), effectiveness of care (33% vs. 30%, P = 0.016), and efficiency of care (29% vs. 23%, P<0.001). High-volume centers were more likely to use quality indicators for evaluating medical errors and adverse events (30% vs. 36%, P<0.001) and the use of guidelines/ protocols (2% vs. 3%, P = 0.001)[20]. The same group of researchers compared the quality improvement programs of trauma centers from 4 high-income countries: United States (263 centers), Canada (46 centers), Australia (18 centers) and New Zealand (3 centers)[21]. Trauma centers from United States reported more than those from Canada and Australasia the measuring quality indicators (100% vs 94% vs 93%, P = 0.008), used report cards (53% vs 33% vs 31%, P = 0.033) and benchmarking (81% vs 61% vs 69%, P = 0.019). The centers from all countries used primarily the hospital process and outcome measures for evaluating if the care was safe (98% vs 97% vs 75%, P = 0.008), effective (97% vs 97% vs 92% P = 0.399), timely (88% vs 100% vs 92%, P = 0.055) and efficient (95% vs 100% vs 83%, P = 0.082)[21].
In a systematic review, Stelfox et al. found the following candidate quality indicators for evaluating trauma care[22]: (i) Peer review of trauma deaths to evaluate quality if care and determine whether the death was potentially preventable. (ii) Hospital mortality. (iii) Complications during hospital stay. (v) Patient treated at the scene longer than “X” minutes (range, 10-30 min). (vi) Glasgow Coma Scale score<X (range 9-14) and no CT scan of the head within X h (range 1-4 hours) of arrival. (vii) Time from patient hospital arrival to emergency surgical treatment (range<30 minutes up to<4 hours). (viii) Unscheduled surgical treatment within X h (range 24-48 h) of initial procedure. (ix) Missed injuries: Injuries diagnosed/documented X h, (range 24 h-discharge), after admission. (x) Glasgow Coma Scale score<X (range 8-10) and airway not secured within X (range,<5 minutespatient leave the emergency department). (xi) Length of Emergency Department stay>X h (range, 2-8 h).
Willis et al. investigated the quality indicators for trauma care, analyzing data from the Victorian State Trauma Registry, including 5 104 cases[23]. Three quality indicatorswere associated with increased mortality: (i) abdominal surgery>24 h after arrival, (ii) blunt compound tibial fracture treatment>8 h after arrival, (iii) non-fixation of femoral diaphyseal fracture. Another three quality indicators were associated with increased lengths of stay: (i) cranial or (ii) abdominal surgery>24 hours after arrival, (iii) patients developing deep vein thrombosis, pulmonary emboli or decubitus ulcers[23].
A study comparing the quality control for trauma management between a level I trauma center from Italy and from Romania, found a major problem of the registration and the complete storage if data concerning trauma care[24]. This audit from 2008 proved good results respect to American College of Surgeons audits, but with important gaps in early treatment of fractures[24].
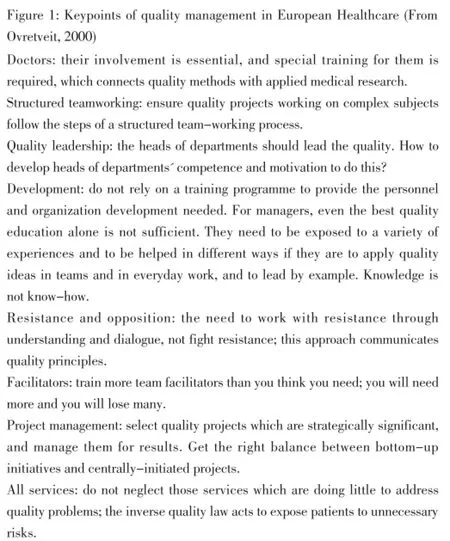
Figure 1: Keypoints of quality management in European Healthcare.
3. Quality Management in Minimally Invasive Surgery
Surveys of complication rates and outcome are a poor substitute for quality control. For the reported complications it is impossible to know which complications are real (inherent to surgery and unavoidable) and which are a consequence of a mistake or an error in judgment[25]. Systematic videorecording of the entire surgical procedures has many advantages for the surgeon and seems to be a good tool for improving quality of the surgical act[25]. First, the videorecording increases the accuracy and precision of surgery, a consequence of the human factor, where alertness is increased and the speed slowed down if the surgeon knows that every mistake will be recoded. Whenever a complication occurs, reviewing the videorecording can be helpful for an early diagnosis and early reintervention. In case of medicolegal problems, the surgeon may prove an accurate, meticulous and precise surgery[25,26].
Kennedy et al. reviewed the database of the American College of Surgeon’s National Surgical Quality Improvement Program[27]. They collected the postoperative complications for patients with laparoscopic or open colonic surgery. They found that laparoscopy decreased overall and individual complications, length of stay and risk for postoperative complications in elderly. The complication rate decreased independently of the probability of morbidity statistic[27].
Analyzing the significant factors that cause delays in surgical operations in a hospital and factors that affect productivity in surgery clinics, Savsar et al. found that delays are unavoidable, but they are associated more with: (i) visiting medical staff than in-house doctors, (ii) missing laboratory or/and radiology tests, (iii) missing pre-anesthesia information, (v) missing informed consent[28]. The authors proposed the following measures to minimize surgery delays: (i) A computer software so that informed consent, pre-anesthesia and lab/radiology procedures are recorded to make sure patients with missing information are not scheduled for surgical procedures. (ii) A policy for enforcing procedures for completing preliminary requirements for surgery and to ensure patients are in hospital enough time to complete all pre-surgery tests and procedures. (iii) A surgery schedule for each doctor should be established along with a linked, checking mechanism so that checks can be made on missing information before surgery. (v) A special checking mechanism for operations assigned to visiting doctors.
4. Conclusions
Romanian hospitals need a more aggressive implementation of total quality management policy, in order to maintain their competitiveness on nowadays European Union competitive market. The total quality management in healthcare heavy support the idea that customer (the patient) satisfaction should exceed the expectations and equal a combination of medical services (diagnoses, medicines, surgery) together with safety, security, an appropriate attitude of the nursing staff, right timing in terms of appointment, delay, service, medical treatment and surgery.
Conflict of interest statement
The authors report no conflict of interest.
Acknowledgement
This paper was supported by the Sectoral Operational Programme Human Resources Development (SOP HTD), financed by the European Social Fund and by the Romanian Government under the contract number POSDRU/159/1.5/ S/137390 for author 2. All authors have equally contributed to this study.
[1] Evans J, Lindsay W. Managing for quality and performance excellence. 8th ed. USA: South-Westeern Cengage Learning; 2008.
[2] Townes C, Petit B, Young B. Implementing total quality management in an academic surgery setting: lessons learned. Swiss Surg. 1995(1):15-23.
[3] Kelly D. Applying quality management in healthcare: a systems approach. 2nd ed. Chicago, Illinois: Health Administrations Press; 2007.
[4] Le Duff F, Daniel S, Kamendjé B, Le Beux P, Duvauferrier R. Monitoring incident report in the healthcare process to improve quality in hospitals. International Journal of Medical Informatics. 2005;74(2-4):111-7.
[5] Ovretveit J. Total quality management in European healthcare. International Journal of Health Care Quality Assurance. 2000;13(2):74-9.
[6] Beuran M, Negoi I, Paun S, Lobontiu A, Filipoiu F, Moldoveanu A, et al. Natural orifice translumenal endoscopic surgery (NOTES) second-look peritoneoscopy for staging of limited peritoneal carcinomatosis. Medical hypotheses. 2013;80(6):745-9.
[7] Holmes EC. General principles of surgery quality control. Chest. 1994;106(6 Suppl):334S-6S.
[8] Shuhaiber JH. Quality measurement of outcome in general surgery revisited: commentary and proposal. Arch Surg. 2002;137(1):52-4.
[9] Spath P. Introduction to healthcare quality management. Chicago, Illinois: Health Administration Press; 2009.
[10] Johannes M, Breinlinger-O’Reilly J, Elser J. Quality management in German health care-the EFQM Excellence Model. International Journal of Health Care Quality Assurance. 2000;13(6):254-8.
[11] Cauchick Miguel PA. Quality management through a national quality award framework. The TQM Magazine. 2006;18(6):626-37.
[12] Levett JM. Implementing an ISO 9001 Quality Management System in a Multispecialty Clinic. Physician Executive. 2005;31(6):46-51.
[13] Theodorakioglou YD, Tsiotras GD. The need for the introduction of quality management into Greek health care. Total Quality Management. 2000;11(8):1153-65.
[14] Beuran M, Negoi I, Paun S, Runcanu A, Gaspar B. [Mechanism of injury--trauma kinetics. What happend? How?]. Chirurgia. 2012;107(1):7-14.
[15] Beuran M, Paun S, Gaspar B, Vartic N, Hostiuc S, Chiotoroiu A, et al. Prehospital trauma care: a clinical review. Chirurgia. 2012;107(5):564-70.
[16] Nast-Kolb D, Waydhas C, Ruchholtz S, Tager G. Trauma care management. Chirurg. 2007;78(10):885-93.
[17] Beuran M, Stoica B, Negoi I, Tanase I, Gaspar B, Turculet C, et al. Trauma registry -- a necessity of modern clinical practice. Chirurgia. 2014;109(2):157-60.
[18] Ruchholtz S, Waydhas C, Aufmkolk M, Tager G, Piepenbrink K, Stolke D, et al. Interdisciplinary quality management in the treatment of severely injured patients. Validation of a QM system for the diagnostic and therapeutic process in early clinical management. Unfallchirurg. 2001;104(10):927-37.
[19] Santana MJ, Stelfox HT. Quality indicators used by trauma centers for performance measurement. J Trauma Acute Care Surg. 2012;72(5):1298-302; discussion 12303.
[20] Stelfox HT, Khandwala F, Kirkpatrick AW, Santana MJ. Trauma center volume and quality improvement programs. J Trauma Acute Care Surg. 2012;72(4):962-7.
[21] Stelfox HT, Straus SE, Nathens A, Gruen RL, Hameed SM, Kirkpatrick A. Trauma center quality improvement programs in the United States, Canada, and Australasia. Ann Surg. 2012;256(1):163-9.
[22] Stelfox H, Bobranska-Artiuch B, Nathens A, Straus SE. Quality indicators for evaluating trauma care: A scoping review. Archives of Surgery. 2010;145(3):286-95.
[23] Willis CD, Stoelwinder JU, Cameron PA. Interpreting process indicators in trauma care: Construct validity versus confounding by indication. International Journal for Quality in Health Care. 2008;20(5):331-8.
[24] Calderale S, Sandru R, Tugnoli G, Di Saverio S, Beuran M, Ribaldi S, et al. Comparison of quality control for trauma management between Western and Eastern European trauma center. World Journal of Emergency Surgery. 2008;3(1):32.
[25] Koninckx P. Videoregistration of surgery should be used as a quality control. Journal of Minimally Invasive Gynecology. 2008;15:248-53.
[26] Beuran M, Paun S, Negoi I, Ganescu R, Runcanu A, Avram M, et al. Laparoscopic approach in gallbladder agenesis--an intraoperative surprise. Chirurgia. 2010;105(4):531-6.
[27] Kennedy GD, Heise C, Rajamanickam V, Harms B, Foley EF. Laparoscopy decreases postoperative complication rates after abdominal colectomy: results from the national surgical quality improvement program. Ann Surg. 2009;249(4):596-601.
[28] Savsar M, Al-Ajmi MM. A quality control application in healthcare management using experimental design criteria. International Journal of Health Care Quality Assurance. 2012;25(1):53-63.
ment heading
10.1016/S2221-6189(14)60057-3
*Corresponding author: Ionut Negoi, MD, PhD, Assistant Professor of Surgery, Carol Davila University of Medicine and Pharmacy Bucharest, General Surgery Department, Emergency Hospital of Bucharest, Romania. No 8 Floreasca Street, Sector 1, 014461, Bucharest, Romania.
Phone number: +40215992308
E-mail: negoiionut@gmail.com
Healthcare
General surgery
Trauma
杂志排行
Journal of Acute Disease的其它文章
- Acute and sub-acute toxicity study of Clerodendrum inerme, Jasminum mesnyi Hance and Callistemon citrinus
- Time-critical AMI Detection: A novel and fast technique using the 12-lead ECG
- Epidemiological survey on scorpionism in Gotvand County, Southwestern Iran: an analysis of 1 067 patients
- The acute effect of the antioxidant drug “U-74389G” on red blood cells levels during hypoxia reoxygenation injury in rats
- Successful treatment of lower urinary tract obstruction with peritonealamniotic and vesicoamniotic shunting
- Simvastatin-induced Toxic Epidermal Necrolysis
