Different profiles of mental and physical health and stress hormone response in women victims of intimate partner violence
2014-03-22ConcepciBlascoRosJoeHerbertManuelaMartinez
Concepción Blasco-Ros, Joe Herbert, Manuela Martinez
1Violence and Health Research Group, Department of Psychobiology, Faculty of Psychology, University of Valencia, Spain
2John van Geest Centre for Brain Repair, Department of Clinical Neurosciences, University of Cambridge, UK
Different profiles of mental and physical health and stress hormone response in women victims of intimate partner violence
Concepción Blasco-Ros1, Joe Herbert2, Manuela Martinez1
1Violence and Health Research Group, Department of Psychobiology, Faculty of Psychology, University of Valencia, Spain
2John van Geest Centre for Brain Repair, Department of Clinical Neurosciences, University of Cambridge, UK
Objectives: To analyse the individual differences in the impact that intimate male partner violence (IPV) has on a woman’s depressive and posttraumatic stress disorder (PTSD) symptomatology, and to determine the association of the different profiles of mental dysfunction with cortisol and dehydroepiandrosterone (DHEA) basal saliva levels as well as physical health symptoms. Methods: A cross-sectional study was carried out in which IPV victims (n=73) and control non-abused (n=31) women participated. Information was obtained through structured interviews and saliva samples were collected for hormonal assays under baseline conditions.
Results: There were three profiles of mental symptoms in IPV subjects: no symptoms (n=19); with depressive symptoms (n=36), and depressive/PTSD symptom (n=18). None of the non-abused women had depressive or PTSD symptoms. The stress hormone response differed between groups. Only the IPV-depressive group had higher evening cortisol, and both morning and evening DHEA, but lower morning cortisol/DHEA ratio than non-abused women. Furthermore, there were differences between the IPV groups. The IPV-depressive group had lower morning cortisol and morning cortisol/DHEA ratio than the IPV-no symptoms and lower morning cortisol/DHEA ratio than the IPV-depressive/PTSD group. With respect to the physical symptoms there was an association between the mean of symptoms and the profile of mental health, the incidence being higher in the depressive/PTSD group than in the other groups. Conclusions: This study demonstrates that there are individual differences in the impact that IPV has on the stress response and health status in women victims.
ARTICLE INFO
Article history:
Received in 19 Dec 2014
Received in revised form 23 Dec 2014
Accepted 9 Jan 2014
Available online 15 Jan 2014
Depression
Dehydroepiandrosterone
Hydrocortisone
Spouse abuse
Symptom assessment
Stress disorders
Post-traumatic
Violence
Women
1. Introduction
Intimate male partner violence (IPV) refers to actual or threatened physically, psychologically or sexually abusive acts committed against women by their current or former male partners. IPV is considered a chronic social stressor for women as this kind of abusive relationships can last for decades[1-3]. Social stress, defined as the stress derived from a social interaction among members in same species, is considered the main source of stress in human beings and, consequently, increases the risk of developing health alterations[4-6]. Cross-sectional, prospective and retrospective studies have consistently demonstrated that living with a violent intimate male partner is a significant contributor to women’s adverse mental and physical health outcomes. Studies which compare women exposed to IPV with those who are not show that common mental sequelae include depression, posttraumatic stress disorder (PTSD), anxiety, suicidal behavior, sleep and eating disorders, low self-esteem, personality disorders, increased likelihood of substance abuse, and social dysfunction[1,7-18]. To our knowledge, there are few studies that have tried to assess mental health profiles on IPV women victims by examining patterns of distress and adjustment[19]. Thus, it is clearly important to assess individual differences to the deleterious effects of IPV on mental health following a person-oriented perspective[17,19-24]. Recent studies have found depressive symptomatology following IPV in 54% to 78%, and PTSD in 18% to 74% ofwomen victims. Furthermore, these women have often comorbid disorders such as mood, anxiety and/or substance abuse disorders[15,17,19,25,26]. IPV has also a great impact on women’s physical health with short- and long-term consequences. First, in case of physical violence, the most common and immediate consequences are injuries, and neurological sequelae of violent acts. However, it is the fear and stress experienced through violence that results in longterm chronic stress-related physical problems. In general, abused women report a low self-perceived health[2,27-29], and higher incidence of different signs somatic symptoms, and illnesses related to the cardiovascular, gastrointestinal, muscular, urinary, and reproductive systems[2,30,31]. The most frequent health problems reported in IPV studies are headaches, nightmares, loss of appetite, back, pelvic, muscular and stomach pain, hypertension, asthma, diabetes, and gynecological symptoms[2,31-34]. Futhermore, other physical disturbances have been studied such as different markers of immune system functioning[35,36], with different results depending on the violence experienced and other mediating factors.
IPV is a chronic stressful experience with high impact on women’s health, as it has been widely endorsed in the literature[2,27,37]. With this in mind, the hypothalamicpituitary-adrenocortical (HPA) axis is the mechanism by which stress regulates its physiological response, and a large number of studies include its markers to measure its impact. This is the main reason why cortisol (and also, but not so far DHEA), the hormone released during the stress response, is one of the most studied biomarker and recognized to have an impact on the rest of body systems[38-40]. In this sense, studies have associated hormone levels with mental health status. It has been demonstrated the impact of IPV on women’s HPA axis[1,25,26,41-45]. Studies that compared nontraumatized healthy women with female victims of IPV found different results. While Griffinet al.[25], reported lower early morning plasma cortisol levels in female victims, Basuet al.[1], found no differences between non-traumatized and female victims. On the other hand, the comparison between female victims of IPV found a variety of results depending on the incidence of PTSD and/or depression. While some studies found higher cortisol levels in women with current PTSD[26] or even remitted PTSD[43], another study reported no difference between female victims with PTSD and those without it[45], and Griffinet al.[25], found lower cortisol levels in female victims with PTSD. Furthermore, those studies that compared female victims with PTSD and those with a comorbid PTSD/depression found no differences[1,25].
The aim of this study was twofold to analyse the individual differences in the impact that IPV has on a woman’s mental and physical health and to determine the association of the different profiles of health impact with cortisol and dehydroepiandrosterone (DHEA) basal saliva levels.
2. Material and methods
2.1. Subjects
The present study is part of a larger research project on the impact of IPV on women’s health carried out in the Valencian Community of Spain[15,46,47]. All participants were of Spanish nationality. Female victims of IPV (n=73) were recruited from the 24 h centers for helping women (which offer information, and help from lawyers and social workers, and some psychological interventions for the women) in the three provinces of the Valencian Community of Spain (Alicante, Castellon and Valencia). A control group of women not exposed to IPV (n=31) was recruited through women’s clubs (a civil organization located in each city and town that only women can join and in which they develop a wide arrange of activities such as receiving information, courses, trips,etc.).
2.2. Ethical considerations
The study was approved by the University of Valencia research ethics committee, and prior informed written consent was obtained from all participants. Subjects did not receive any money or other inducement for their participation.
2.3. Procedure
The study consisted of a structured interview in which trained female psychologists asked women questions about their lives and health. In general, each woman was interviewed four to six times, and the duration of each session was approximately 1.5 h. A comprehensive questionnaire was designed for use in a face-to-faceinterview. The majority of questions were designed to obtain objective factual reports. Additionally, women were asked to provide saliva samples for hormonal assays (details below).
奥苏泊尔认为,知识迁移就是人们已有的认知结构对新知识学习发生影响。而如果已知的知识技能对学习的新知识技能产生干扰,起消极阻碍的影响,称为负迁移。因此,教师应重视负迁移带来的消极效应,尤其是对于容易混淆的计算问题,更需要克服定式思维,通过辨析、纠错等活动突出新知识的内涵、特征和规律,提升学习效率。
2.4. Questionnaires
The questionnaires from which information for the present study was obtained are described below, and more detailed information is given in our previous articles[44,46].
The sociodemographic profile included age, educationlevel and marital status items. The relationship with the aggressor/partner included data on the cohabitation with him at the time of the interviews and during the last year.
2.5. Characteristics of intimate male partner violence
A questionnaire was constructed to obtain detailed information about the different types of violence (physical, psychological and sexual) toward the women perpetrated by their partners (see 46 for more detailed information). Women gave answers of either “yes” or “no” regarding the experience of each act.
2.6. Mental health assessment
The Beck Depression Inventory (BDI) was used to assess depressive symptoms[48], and the total scores on the BDI ranged from 0 to 63. Women with BDI scores ranging from 0 to 8 were considered as having no symptoms of depression, from 9 to 18 as mild, from 9 to 29 as moderate, and from 30 to 63 to severe depressive symptoms. The Spanish version of the BDI that was used in our study has been validated by Conde and Useros[49], who obtained an internal consistency coefficient of 0.88. In our study, the cut-off score was set to 18. The incidence and severity of symptoms of current PTSD were assessed with Echeburúa’s Severity of Symptom Scale of Posttraumatic Stress Disorder[50]. This is a structured interview based on DSM-IV criteria. The instrument has a high internal consistency with a Cronbach’s α coefficient of 0.92 and a high test-retest reliability as well as a good discriminant, concurrent, and construct validity. A stressor was assessed by asking the woman if she had experienced an unusual, extremely distressful event (irrespective of whether or not it was IPV-related). Either type of event was considered a qualifying trauma when it met the DSM-IV criteria for PTSD and when distressing symptoms persisted for at least 4 weeks. Women were also asked about the lifetime incidence of thoughts and attempts of suicide. Detailed information about women’s mental health assessment is given in Picó-Alfonsoet al[15].
2.7. Physical health assessment
Self-report physical health status was assessed using a questionnaire designed by the research team. A symptom is defined as a subjective evidence of physical disturbance observed by the patient. The symptom inventory consisted of 35 symptoms and women were queried about their incidence in the year preceding the study. Furthermore, a total number of symptoms as well as a summatory of specific system symptoms was also calculated.
2.8. Saliva samples
Saliva samples for the analysis of the level of cortisol and DHEA were also collected. The participants provided a minimum of 0.5 mL of saliva in a plastic tube twice a day (between 08:00 and 09:00, and between 20:00 and 21:00) for four consecutive days at home, starting the fourth day after the beginning of menstruation. Saliva samples were frozen in women’s freezer and brought to the freezer of the Department of Psychobiology in a mobile freezer, and then kept frozen at -21℃. Finally, all samples were sent to the Department of Clinical Neurosciences at University of Cambridge, UK, for analysis.
2.8.1. Hormone assays
Cortisol was measured by validated ELISA on 20 μL samples of saliva (antibody Cambio UK) without extraction (intra-assay variation: 4.1%; inter-assay: 7.6%). DHEA was measured by validated radioimmunoassay on 333 μL samples after extraction into hexane/ether (4:1) (antibody Bioclin; intra-assay variation: 5.1%; inter-assay: 11.2%). Details are given in Harriset al.[51]. Data from the four daily morning and evening collections were summed to give a mean value at each time point.
2.9. Statistical analyses
Women were classified into four groups depending on the incidence of IPV and their mental health status: non-abused women, and abused women with no depressive or PTSD symptoms (IPV-no symptoms), with depressive symptoms (IPV-depressive symptoms), and with both depressive and PTSD symptoms (IPV-depressive/PTSD symptoms). The four groups were compared with respect to age, and the profile of physical symptoms and mental health status using Oneway analysis of variance (ANOVAs). Regarding the level of education, marital status, types of IPV, the incidence of clinical depression and PTSD the comparisons were assessed by using Pearson’sChi-square tests. Comparisons between groups with respect to endocrine measures (cortisol and DHEA analysis were carried out after logarithmic transformation of the data) were assessed by ANOVAs withBonferronipost hoccomparisons. When the criteria of ANOVA were not fulfilled, Welch’s tests were calculated, and Games-Howellpost hoccomparisons applied. A significance level ofP<0.05 was established for all analyses. All statistical analyses were conducted using the SPSS for Windows statistical package Version 19.0.
3. Results
3.1. Participant’s characteristics and health profiles
There were no differences between groups in either age (Vw[3, 49.13]=1.25) or education [χ2(18,N=104)=16.60] (Table 1). There was a significant association between the marital status and group [χ2(12,N=104)=33.40,P<0.001]. The percentage of “married” women was higher than expected by chance in the non-abused group, whereas the contrary pattern was observed in the category of “separated/ divorced”. There were no significant association between this variable and any of the three IPV-groups [χ2(8,N= 73)=9.63]. On the other hand, there was a significant association between the cohabitation with the aggressor/ partner at the time of the interviews and the group [χ2(3,N= 104)=19.95,P<0.001]. The proportion of women cohabiting with the aggressor/partner was significantly higher than expected in the nonabused group (96.8%) and lower in the IPV-no symptoms group (42.1%). However, this was not apparent during the year previous to the interviews [χ2(3,N=104)=5.43]. In the IPV-groups, there was no significant association between the cohabitation and the group either during the previous year [χ2(2,N=73)=3.06] or at the time of the interviews: [χ2 (2,N=73)=1.47].
All women (100%) in the IPV groups were exposed to psychological abuse by their partners. Furthermore, over a half of women on each IPV group were physically abused, and around one third of them were sexually abused by their partners. There was no association between the incidence of physical and sexual abuse and the mental health profile of women victims of IPV: physical [χ2(2,N=73)=2.19, n.s.], and sexual [χ2(2,N=73)=1.33].
3.2. Different profiles of depressive and PTSD symptomatology
One hundred and four women participated in this study. Seventy three were female victims of IPV and 31 were women no exposed to IPV (non-abused women). Depending on the incidence of symptoms of depression and PTSD female victims were distributed into three groups: (1) Female victims of IPV with no symptoms of depression or PTSD (IPV-no symptoms group;n=19); (2) Female victims of IPVwith symptoms of depression (IPV-depressive group;n=36), and (3) Female victims of IPV with symptoms of depression and PTSD (IPV-depressive/PTSD group;n=18). None of the non-abused women had either symptoms of depression or PTSD (non-abused group;n=31).

Table 1 Characteristics of nonabused women and women victims of intimate male partner violence with no symptoms, depressive symptoms, and depressive and posttraumatic stress disorder symptoms.
The scores for depression were significantly higher in both the IPV-depressive and the IPV-depressive/ PTSD groups than in the IPV-no symptoms and nonabused groups (P<0.001). Moreover, the IPV-depressive/ PTSD group had higher scores than the IPV-depressive group (P<0.05). In the IPV-depressive group women were distributed mainly among “mild” (72.2%) symptoms, while the highest level of severity was found in IPV-depressive/PTSD group: 38.9% of women suffered “severe”symptoms, these percentages being higher than expected by chance in both groups. On the other hand, PTSD scores were significantly higher, not only in those with clinical PTSD, but also in the IPV-depressive group than in the IPV-no symptoms and non-abused groups (P<0.001). Furthermore, the IPV-depressive/PTSD group had higher scores than all the other groups (P<0.001). Regarding suicide, the incidence of both suicidal thoughts and attempts was associated with the group: thoughts [χ2(3,N=104)=28.67,P<0.001] and attempts [χ2(3,N=104)=12.21,P<0.01]. In the case of thoughts, the incidence was higher than expected in both IPV-depressive and IPV-depressive/PTSD groups, and only in the latter group regarding suicidal attempts. On the contrary, the incidence of both thoughts and attempts of suicide were lower than expected in the nonabused group (Table 2).
3.3. Association of the different profiles of mental health dysfunction with physical health
The four groups of women were compared with regards to the incidence of perceived physical symptoms during the year prior to the interviews. Detailed information of total amount of physical symptoms as well as the incidence of each specific symptom is given in Table 3.
There were differences between groups in the total amount of physical symptoms (Vw[3, 44.14]=52.71;P<0.001).Post hoccomparisons indicated that the IPV-depressive/PTSD group had higher incidence of symptoms than the other three groups (P<0.001), and the IPV-depressive group showed a higher mean than non-abused (P<0.001) and IPV-no symptoms group (P<0.05).
There were differences between groups in the total amount of symptoms of specific systems: nervous (Vw[3, 45.28]= 38.02;P<0.001), muscular (Vw[3, 48.13]=26.39;P<0.001), reproductive (F[3, 103]=4.04;P<0.01), digestive (Vw[3, 44.92] =14.25;P<0.001), circulatory (Vw[3, 44.30]=22.38;P<0.001) and the endocrine system (Vw[3, 41.83]=60.92;P<0.001) with the only exception of urinary system and skin (F[3, 103] =0.60).Post hoccomparisons showed a higher amount of symptoms in both IPV-depressive/PTSD and IPV-depressive groups than in the non-abused group (P<0.001, reproductive system:P<0.05). The IPV-depressive/PTSD group showed a higher amount of symptoms in nervous, muscular and endocrine systems (P<0.001), as well as in digestive and circulatory systems (P<0.05) than the IPV-no symptom group, and a higher number of symptoms in nervous andendocrine systems than the IPV-depressive group (P<0.001). Furthermore, IPV-depressive group showed a higher amount of muscular symptoms than the IPV-no symptom group (P<0.05). The only difference between IPV-no symptoms and the non-abused group was a higher amount of symptoms in the endocrine system in the former group (P<0.05).

Table 3 Physical symptoms suffered by nonabused women and women victims of violence with no symptoms, depressive symptoms, and depressive and PTSD symptoms during the last year.
Twenty-six specific symptoms out of 35 were significantly associated with the group: headache [χ2(3,N=104)=15.87,P<0.001], faintness [χ2(3,N=104)=26.58,P<0.001], numbness [χ2(3,N=104)=27.85,P<0.001], trembling hands [χ2(3,N=104)=27.05,P<0.001], ringing ears [χ2(3,N=104)=21.51,P<0.001], dizziness [χ2(3,N=104)=21.14,P<0.001], blurred vision [χ2(3,N=104)=14.94,P<0.01], nightmares [χ2(3,N=104)=27.95,P<0.001], low energy [χ2(3,N=104)=34.44,P<0.001], fatigue [χ2(3,N=104)=24.83,P<0.001], muscular pain [χ2(3,N=104)=22.35,P<0.001], back pain [χ2(3,N=104)=15.01,P<0.01], pelvic pain [χ2(3,N=104)=8.05,P<0.05], nausea [χ2(3,N=104)=10.88,P<0.05], vomiting [χ2(3,N=104)=14.48,P<0.01], heartburn [χ2(3,N=104)=14.26,P<0.01], stomach pain [χ2(3,N=104)=20.04,P<0.001], diarrhea [χ2(3,N=104)=10.88,P<0.05], bloating [χ2(3,N=104)=9.02,P<0.05], anal bleeding [χ2(3,N=104)=10.55,P<0.05], chest pain [χ2(3,N=104)=27.95,P<0.001], palpitations [χ2(3,N=104)=29.19,P<0.001], shortness of breath [χ2(3,N=104)=20.76,P<0.001], weight change [χ2(3,N=104)=34.18,P<0.001], and appetite lost [χ2(3,N=104)=40.43,P<0.001], with the exception of most symptoms of the reproductive system: amenorrhoea [χ2(3,N=104)=1.23], menstrual pain [χ2(3,N=104)=0.48], vaginal bleeding [χ2(3,N=104)=2.54], vaginal pain [χ2(3,N=104)=6.10], painful intercourse [χ2(3,N=104)=5.32], constipation [χ2(3,N=104)=7.31], leakage of urine [χ2(3,N=104)=5.41], pruritus [χ2(3,N=104)=1.89] and eruptions [χ2(3,N=104)=0.92] (Table 3).

Table 4 Basal saliva levels of cortisol, DHEA (ng/ml, and ratio C/DHEA (nMol/L in the morning and evening in Nonabused women and women victims of Intimate male partner violence with no symptoms, depressive symptoms, and depressive/posttraumatic stress disorder symptoms. (Mean and standard deviation, SD.
The incidence of the following symptoms was higher than expected by chance in the IPV-depressive/PTSD group: headache, faintness, numbness, trembling hands, ringing ears, dizziness, nightmares, low energy, fatigue, muscular pain, back pain, pelvic pain, nausea, vomiting, heartburn, stomach pain, diarrhea, chest pain, palpitations, shortness of breath, weight change, and loose of appetite. Also in the IPV-depressive group eight symptoms had a higher incidence than expected: headache, blurred vision, low energy, muscular pain, bloating, anal bleeding, chest pain, palpitations, and shortness of breath. On the contrary, just two symptoms, vomiting and palpitations, had a lower incidence than expected in IPV-no symptoms group. Regarding nonabused group, almost all symptoms showed a lower incidence than expected, with the exception of vomiting, diarrhea, and bloating.
3.4. Association of the different profiles of mental health dysfunction with cortisol and DHEA basal saliva levels
The four groups of women were compared with regards to the basal level of cortisol and DHEA as well as the ratio cortisol/DHEA (C/DHEA). Mean basal levels and comparisons between groups are given in Table 4. There were significant differences in mean morning and evening cortisol levels between the groups [ANOVA: morning:F[3, 103]=4.14;P=.008; evening: Vw[3, 42.89]=5.34;P=.003F(1, 115)].Post hoccomparisons revealed that morning levels were lower in the IPV-depressive group than in the IPV-no symptoms group (P<0.05), while evening cortisol levels were significantly higher in IPV-depressive group than in the non-abused group (P<0.01). Both morning and evening DHEA were significantly different between groups (morning: F [3, 103]=4.51;P=0.005); evening: Vw[3, 45.19]=4.45;P=0.008).Post hoccomparisons showed that both morning and evening DHEA levels were higher in the IPV-depressive group than in the non-abused group (P<0.01).
As it is shown in Figure 1, morning C/DHEA ratio was significantly different between the groups (Vw[3,48.86]=7.51;P<0.001).Post hoccomparisons indicated that the ratio was lower in the IPV-depressive group than in all the other groups (non-abused:P<0.001; IPV-no symptoms:P<0.05; and IPV-depressive/PTSD:P<0.01).
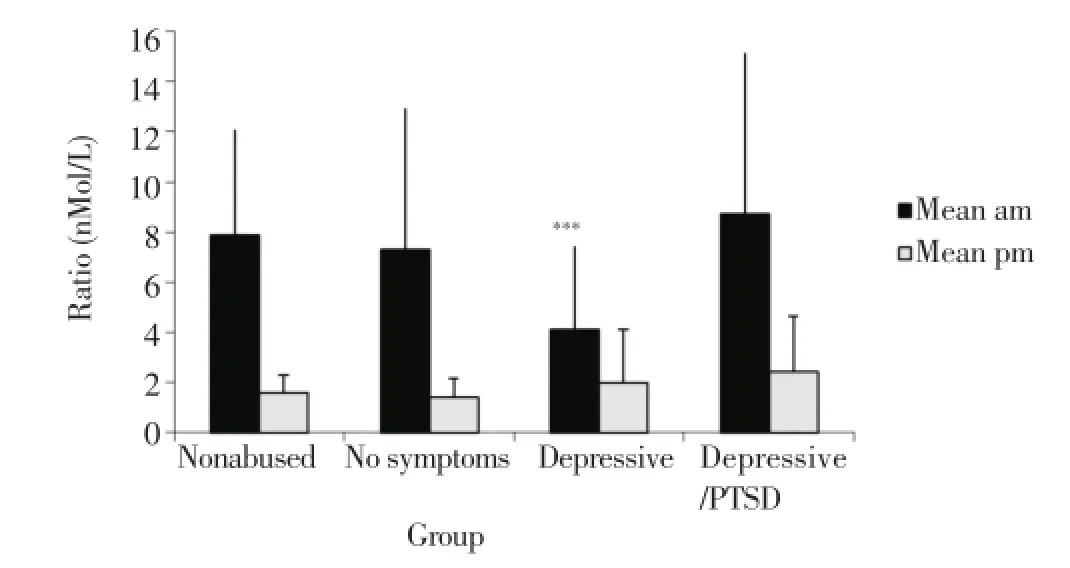
Figure 1. Mean±SD of morning C/DHEA ratio (nMol/L) in evening in nonabused women and women victims of intimate male partner violence with no symptoms, depressive symptoms, and depressive/posttraumatic stress disorder symptoms.***: Differs from nonabused group; P<0.001, IPV-No symptoms; P<0.05, and IPV-depressive/PTSD; P<0.01.
4. Discussion
Our results show that there are individual differences in the impact that the exposure to IPV has on women’s health. Thus, while some women show no symptoms of either depression or PTSD (the IPV-no symptoms group), others develop mostly mild depression (IPV-depressive group), and the rest women a comorbid more severe depression and PTSD (IPV-depressive/PTSD group). Thus, exposure to IPV does not necessarily lead to the development of psychopathology in all women or to a unique pattern of mental ill-health. A more detailed assessment of mental health in female victims may aid the design of appropriate intervention policies[15,19,20,23,24].
With respect to physical health there is an association between the amount of somatic symptoms and mental health deterioration profile. The main results shown that the IPV-depressive/PTSD group had the highest incidence in the total amount of symptoms followed by the IPV-depressive group in comparison with the IPV-no symptoms group and the non-abused group. Furthermore, the incidence of the specific symptoms headache, faintness, numbness, trembling hands, ringing ears, dizziness, nightmares, low energy, fatigue, muscular pain, back pain, pelvic pain, nausea, vomiting, heartburn, stomach pain, diarrhea, chest pain, palpitations, shortness of breath, weight change, and loose of appetite was higher than expected by chance in the IPV-depressive/PTSD group, while headache, blurred vision, low energy, muscular pain, bloating, anal bleeding, chest pain, palpitations, and shortness of breath was higher than expected by chance in the IPV-depressive group. These results are consistent with other studies that analyzed physical symptomatology in women victims[32,34].
Finally, there is also an association between levels of stress hormones and mental health deterioration. A disturbed HPA axis could either reflect or contribute to the array of mental stress-related disorders[40,52-54]. Our results clearly demonstrate that dysregulation of the HPA axis and basal levels of DHEA are particularly associated with depressive symptoms in women exposed to IPV. The IPV-depressive group had lower morning cortisol levels than the IPV-no symptoms group but higher evening cortisol levels and both higher morning and evening DHEA levels in comparison to the nonabused group. More significantly, they had a lower morning cortisol/DHEA ratio than all the other groups. However, no significant alterations compared to non-abused controls were found in those women with neither depressive nor PTSD symptoms (IPV-no symptoms) or those with comorbidity of these two disorders (IPV-depressive/PTSD group). Previous studies reported that female victims of IPV who developed PTSD had higher morning levels of cortisol than those that did not[25,26,43]. However, in general, studies on cortisol in patients with PTSD have revealed inconsistent results, while some studies reported no differences in cortisol levels between individuals with PTSD and controls or between trauma-exposed subjects with and without PTSD, and even others found higher levels[55-58]. On the other hand, the comorbidity of major depressive disorder and PTSD has received scant attention[59], studies reporting a variety of results[60-62]. The meta-analysis conducted by Morriset al.[63], on 47 studies revealed that daily cortisol output was lower in trauma-exposed individuals with comorbid major depressive disorder/PTSD in comparison to controls. Our results suggest that cortisol is altered specifically in those with depressive symptoms alone following IPV. It is not clear whether this indicates a distinct psychopathological state, or whether altered cortisol in some way influences the psychological response to IPV. It is possible that the presence of the two sets of symptoms in our subjects have opposite actions on cortisol, though we had no women with PTSD alone. This cannot be verified from our data. Since the risk for depression as well as depression itself, is associated with higher morning cortisol, it is unclear whether our results reflect an epiphenomenon of depressed state, or an antecedent risk for it.
Both lower and higher levels of DHEA have been reported in depressed subjects in comparison to controls[64-68]. It is interesting, in view of the finding that altered cortisol was restricted to the IPV-depressive group, that this was also the group in which DHEA was altered in comparison to controls. The high levels found in women of the IPV-depressive group in our study may have some protective effects against putative deleterious actions of cortisol[69]. However, as this is a cross-sectional study, it was not possible to assess whetherhigh levels of DHEA predicted a reduced incidence of depressive symptoms. Since altered cortisol and DHEA was limited to the IPV-depressive group, their C/DHEA ratio was also altered, as would be expected. Elevated C/DHEA ratios have reported as a state marker of depressive illness[64,70,71].
The present results indicate that women exposed to IPV show differences in the vulnerability and resilience to the development of psychopathology, somatic symptoms as well to the alterations in the endocrine system[71], and the two may be related. What makes some women more vulnerable to develop specific IPV-related health deterioration and others resilient is not well understood. Thus, discovering those variables that may contribute to the different vulnerability and resilience to develop health deterioration is important for advancing diagnostic screening, prevention and treatment[21,24,72,73].
A limitation of this study consists on the method used for the recruitment of the sample. Women victims of IPV were recruited from the Centers for Helping Women, while the recruitment from other settings such as Primary health care could gather a wider sample of victims.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Acknowledgements
We would like to thank the Conselleria of Social Welfare of Valencia and the 24-h Centers for Helping Women of the Valencia Community of Spain for their assistance in contacting women victims of partner violence.
Funding for this study was provided by The Institute of the Woman, Ministry of Work and Social Affairs (ref: 53/98), FEDER and the Ministry of Science and Innovation (Plan Nacional de Investigación Científica, Desarrollo e Innovación Tecnológica; ref: BSO2001-3134, Spain), and the Conselleria D’Educació (PROMETEO 2011/048). The sponsors had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
[1] Basu A, Levendosky AA, Lonstein JS. Trauma sequelae and cortisol levels in women exposed to intimate partner violence. Psychodyn Psychiatry 2013; 41(2): 247-275.
[2] Campbell JC. Health consequences of intimate partner violence. Lancet 2002; 359(9314): 1331-1336.
[3] Martínez M, García-Linares MI, Picó-Alfonso MA. Women victims of domestic violence: consequences for their health and the role of the health system. In: Klein R, Bernard W, editors. Conflict, gender, and violence. Vienna: Studien-Verlag; 2004. p. 127-155.
[4] Chuang CH, Cattoi AL, McCall-Hosenfeld JS, Camacho F, Dyer AM, Weisman CS. Longitudinal association of intimate partner violence and depressive symptoms. Ment Health Fam Med 2012; 9(2): 107-114.
[5] Martinez M, Calvo-Torrent A, Pico-Alfonso MA. Social defeat and subordination as models of social stress in laboratory rodents: a review. Aggress Behav 1998; 24(4): 241-256.
[6] Poirier GL, Cordero MI, Sandi C. Female vulnerability to the development of depression-like behavior in a rat model of intimate partner violence is related to anxious temperament, coping responses and amygdala vasopressin receptor 1a expression. Front Behav Neurosci 2013; 7: 35.
[7] Aguilar RJ, Nightingale NN. The impact of specific battering experiences on the self-esteem of abused women. J Fam Violence 1994; 9(1): 35-45.
[8] Bergman B, Brismar B. A 5-year follow-up study of 117 battered women. Am J Public Health 1991; 81(11): 1486-1489.
[9] Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med 2002; 23(4): 260-268.
[10] Ehrensaft MK, Moffitt TE, Caspi A. Is domestic violence followed by an increased risk of psychiatric disorders among women but not among men? A longitudinal cohort study. Am J Psychiatry 2006; 163(5): 885-892.
[11] Houry D, Kemball R, Rhodes KV, Kaslow NJ. Intimate partner violence and mental health symptoms in African American female ED patients. Am J Emerg Med 2006; 24(4): 444-450.
[12] Humphreys JC, Lee KA, Neylan TC, Marmar CR. Sleep patterns of sheltered battered women. Image J Nurs Sch 1999; 31(2): 139-143.
[13] McCaw B, Golding JM, Farley M, Minkoff JR. Domestic violence and abuse, health status, and social functioning. Women Health 2007; 45(2): 1-23.
[14] Pico-Alfonso MA, Echeburúa E, Martinez M. Personality disorder symptoms in women as a result of chronic intimate male partner violence. J Fam Viol 2008; 23(7): 577-588.
[15] Pico-Alfonso MA, Garcia-Linares MI, Celda-Navarro N, Blasco-Ros C, Echeburua E, Martinez M. The impact of physical, psychological, and sexual intimate male partner violence on women’s mental health: depressive symptoms, posttraumatic stress disorder, state anxiety, and suicide. J Womens Health (Larchmt) 2006; 15(5): 599-611.
[16] Ruiz-Pérez I1, Plazaola-Castaño J. Intimate partner violenceand mental health consequences in women attending family practice in Spain. Psychosom Med 2005; 67(5): 791-797.
[17] Young-Wolff KC, Hellmuth J, Jaquier V, Swan SC, Connell C, Sullivan TP. Patterns of resource utilization and mental health symptoms among women exposed to multiple types of victimization: a latent class analysis. J Interpers Violence 2013; 28(15): 3059-3083.
[18] Zlotnick C, Johnson DM, Kohn R. Intimate partner violence and long-term psychosocial functioning in a national sample of American Women. J Interpers Violence 2006; 21(2): 262-275.
[19] Hughes HM, Cangiano C, Hopper EK. Profiles of distress in sheltered battered women: implications for intervention. Violence Vict 2011; 26(4): 445-460.
[20] Anderson KM, Renner LM, Danis FS. Recovery: resilience and growth in the aftermath of domestic violence. Violence Against Wom 2012; 18(11): 1279-1299.
[21] Bogat GA, Levendosky AA, von Eye A. The future of research on intimate partner violence: person-oriented and variable-oriented perspectives. Am J Community Psychol 2005; 36(1-2): 49-70.
[22] Karatsoreos IN, McEwen BS. Psychobiological allostasis: resistance, resilience and vulnerability. Trends Cogn Sci 2011; 15(12): 576-584.
[23] Nurius PS, MacY RJ. Heterogeneity among violence-exposed women: applying person-oriented research methods. J Interpers Violence 2008; 23(3): 389-415.
[24] Nurius PS, Macy RJ. Person-oriented methods in partner violence research: distinct biopsychosocial profiles among battered women. J Interpers Violence 2010; 25(6): 1064-1093.
[25] Griffin MG, Resick PA, Yehuda R. Enhanced cortisol suppression following dexamethasone administration in domestic violence survivors. Am J Psychiatry 2005; 162(6): 1192-1199.
[26] Johnson DM, Delahanty DL, Pinna K. The cortisol awakening response as a function of PTSD severity and abuse chronicity in sheltered battered women. J Anxiety Disord 2008; 22(5): 793-800.
[27] Ellsberg M, Jansen HAFM, Heise L, Watts CH, Garcia-Moreno C, WHO Multi-country Study on Women’s Health and Domestic Violence against Women Study Team. Intimate partner violence and women’s physical and mental health in the WHO multicountry study on women’s health and domestic violence: an observational study. Lancet 2008; 371(9619): 1165-1172.
[28] Hellemans S, Buysse A, De Smet O, Wietzker A. Intimate partner violence in Belgium: prevalence, individual health outcomes, and relational correlates. Psychol Belg 2014; 54(1): 79-96.
[29] Vives-Cases C, Torrubiano-Domínguez J, Escribà-Agüir V, Ruiz-Pérez I, Montero-Piñar MI, Gil-González D. Social determinants and health effects of low and high severity intimate partner violence. Ann Epidemiol 2011; 21(12): 907-913.
[30] Campbell JC, Lewandowski LA. Mental and physical health effects of intimate partner violence on women and children. Psychiatr Clin North Am 1997; 20(2): 353-374.
[31] de Sousa J, Burgess W, Fanslow J. Intimate partner violence and women’s reproductive health. Obstet, Gynaecol Reprod Med 2014; 24(7): 195-203.
[32] Ruiz-Pérez I, Plazaola-Castaño J, Del Río-Lozano M. Physical health consequences of intimate partner violence in Spanish women. Eur J Public Health 2007; 17(5): 437-443.
[33] Sanchez-Lorente S, Blasco-Ros C, Martínez M. Factors that contribute or impede the physical health recovery of women exposed to intimate partner violence: a longitudinal study. Womens Health Issues 2012; 22(5): e491-e500.
[34] Watkins LE, Jaffe AE, Hoffman L, Gratz KL, Messman-Moore TL, DiLillo D. The longitudinal impact of intimate partner aggression and relationship status on women’s physical health and depression symptoms. J Fam Psychol 2014; 28(5): 655-665.
[35] Garcia-Linares MI, Sanchez-Lorente S, Coe CL, Martinez M. Intimate male partner violence impairs immune control over herpes simplex virus type 1 in physically and psychologically abused women. Psychosom Med 2004; 66(6): 965-972.
[36] Newton TL, Fernandez-Botran R, Miller JJ, Lorenz DJ, Burns VE, Fleming KN. Markers of inflammation in midlife women with intimate partner violence histories. J Womens Health (Larchmnt) 2011; 20(12): 1871-1880.
[37] Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet 2002; 360(9339): 1083-1088.
[38] Bowes L, Jaffee SR. Biology, genes, and resilience: toward a multidisciplinary approach. Trauma Violence Abuse 2013; 14(3): 195-208.
[39] Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol 2009; 5(7): 374-381.
[40] Koolhaas JM, Bartolomucci A, Buwalda B, de Boer SF, Flügge G, Korte SM, et al. Stress revisited: a critical evaluation of the stress concept. Neurosci Biobehav Rev 2011; 35(5): 1291-1301.
[41] Constantino RE, Sekula LK, Rabin B, Stone C. Negative life experiences, depression, and immune function in abused and nonabused women. Biol Res Nurs 2000; 1(3): 190-198.
[42] Feinberg ME, Jones DE, Granger DA, Bontempo D. Relation of intimate partner violence to salivary cortisol among couples expecting a first child. Aggress Behav 2011; 37(6): 492-502.
[43] Inslicht SS, Marmar CR, Neylan TC, Metzler TJ, Hart SL, Otte C, et al. Increased cortisol in women with intimate partner violencerelated posttraumatic stress disorder. Psychoneuroendocrinology 2006; 31(10): 825-838.
[44] Pico-Alfonso MA, Garcia-Linares MI, Celda-Navarro N, Herbert J, Martinez M. Changes in cortisol and dehydroepiandrosterone in women victims of physical and psychological intimate partner violence. Biol Psychiatry 2004; 56(4): 233-240.
[45] Seedat S, Stein MB, Kennedy CM, Hauger RL. Plasma cortisol and neuropeptide Y in female victims of intimate partner violence. Psychoneuroendocrinology 2003; 28(6): 796-808.
[46] Garcia-Linares MI, Pico-Alfonso MA, Sanchez-Lorente S, Savall-Rodriguez F, Celda-Navarro N, Blasco-Ros C, et al. Assessing physical, sexual, and psychological violence perpetrated by intimate male partners toward women: a Spanish cross-sectional study. Violence Vict 2005; 20(1): 99-123.
[47] Blasco-Ros C, Sánchez-Lorente S, Martinez M. Recovery from depressive symptoms, state anxiety and post-traumatic stress disorder in women exposed to physical and psychological, but not to psychological intimate partner violence alone: a longitudinal study. BMC Psychiatry 2010; 10: 98.
[48] Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961; 4: 561-571.
[49] Conde V, Useros E. Adaptación castellana de la escala de evaluación conductual para la depresión de Beck. Rev Psiquiatr Psicol Med Eur Am 1975; 12: 217-236.
[50] Echeburua E, Corral P, Amor PJ, Zubizarreta L, Sarasúa B. Escala de gravedad de síntomas de trastorno de estrés postraumático: propiedades psicométricas. Anal Modificación Conducta 1997; 23: 503-526.
[51] Harris TO, Borsanyi S, Messari S, Stanford K, Cleary SE, Shiers HM, et al. Morning cortisol as a risk factor for subsequent major depressive disorder in adult women. Br J Psychiatry 2000; 177: 505-510.
[52] Herbert J. Neurosteroids, brain damage, and mental illness. Exp Gerontol 1998; 33(7-8): 713-727.
[53] Dettenborn L, Muhtz C, Skoluda N, Stalder T, Steudte S, Hinkelmann K, et al. Introducing a novel method to assess cumulative steroid concentrations: increased hair cortisol concentrations over 6 months in medicated patients with depression. Stress 2012; 15(3): 348-353.
[54] Herbert J. Cortisol and depression: three questions for psychiatry. Psychol Med 2013; 43(3): 449-469.
[55] Klaassens ER, Giltay EJ, Cuijpers P, van Veen T, Zitman FG. Adulthood trauma and HPA-axis functioning in healthy subjects and PTSD patients: a meta-analysis. Psychoneuroendocrinology 2012; 37(3): 317-331.
[56] Lemieux AM, Coe CL. Abuse-related posttraumatic stress disorder: evidence for chronic neuroendocrine activation in women. Psychosom Med 1995; 57(2): 105-115.
[57] Meewisse ML, Reitsma JB, de Vries GJ, Gersons BP, Olff M. Cortisol and post-traumatic stress disorder in adults: systematic review and meta-analysis. Br J Psychiatry 2007; 191: 387-392.
[58] Pervanidou P, Chrousos GP. Neuroendocrinology of posttraumatic stress disorder. Prog Brain Res 2010; 182: 149-160.
[59] Vythilingam M, Gill JM, Luckenbaugh DA, Gold PW, Collin C, Bonne O, et al. Low early morning plasma cortisol in posttraumatic stress disorder is associated with co-morbid depression but not with enhanced glucocorticoid feedback inhibition. Psychoneuroendocrinology 2010; 35(3): 442-450.
[60] Gill J, Vythilingam M, Page GG. Low cortisol, high DHEA, and high levels of stimulated TNF-alpha, and IL-6 in women with PTSD. J Trauma Stress 2008; 21(6): 530-539.
[61] Oquendo MA, Friend JM, Halberstam B, Brodsky BS, Burke AK, Grunebaum MF, et al. Association of comorbid posttraumatic stress disorder and major depression with greater risk for suicidal behavior. Am J Psychiatry 2003; 160(3): 580-582.
[62] Young EA, Breslau N. Saliva cortisol in posttraumatic stress disorder: a community epidemiologic study. Biol Psychiatry 2004; 2(3): 205-209.
[63] Morris MC, Compas BE, Garber J. Relations among posttraumatic stress disorder, comorbid major depression, and HPA function: a systematic review and meta-analysis. Clin Psychol Rev 2012; 32(4): 301-315.
[64] Goodyer IM, Herbert J, Altham PM, Pearson J, Secher SM, Shiers HM. Adrenal secretion during major depression in 8- to 16-year-olds, I. Altered diurnal rhythms in salivary cortisol and dehydroepiandrosterone (DHEA) at presentation. Psychol Med 1996; 26(2): 245-256.
[65] Heuser I, Deuschle M, Luppa P, Schweiger U, Standhardt H, Weber B. Increased diurnal plasma concentrations of dehydroepiandrosterone in depressed patients. J Clin Endocrinol Metab 1998; 83(9): 3130-3133.
[66] Michael A, Jenaway A, Paykel ES, Herbert J. Altered salivary dehydroepiandrosterone levels in major depression in adults. Biol Psychiatry 2000; 48(10): 989-995.
[67] Lopes RP, Grassi-Oliveira R, de Almeida LR, Stein LM, Luz C, Teixeira AL, et al. Neuroimmunoendocrine interactions in patients with recurrent major depression, increased early life stress and long-standing posttraumatic stress sisorder symptoms. Neuroimmunomodulation 2012; 19(1): 33-42.
[68] Phillips AC, Batty GD, Gale CR, Lord JM, Arlt W, Carroll D. Major depressive disorder, generalised anxiety disorder, and their comorbidity: associations with cortisol in the Vietnam experience study. Psychoneuroendocrinology 2011; 36(5): 682-690.
[69] Yehuda R, Brand SR, Golier JA, Yang RK. Clinical correlates of DHEA associated with post-traumatic stress disorder. Acta Psychiatr Scand 2006; 114(3): 187-193.
[70] Markopoulou K, Papadopoulos A, Juruena MF, Poon L, Pariante CM, Cleare AJ. The ratio of cortisol/DHEA in treatment resistant depression. Psychoneuroendocrinology 2009; 34(1): 19-26.
[71] Young AH, Gallagher P, Porter RJ. Elevation of the cortisoldehydroepiandrosterone ratio in drug-free depressed patients. Am J Psychiatry 2002; 159(7): 1237-1239.
[72] Adams TB, Wharton CM, Quilter L, Hirsch T. The association between mental health and acute infectious illness among a national sample of 18- to 24-year-old college students. J Am Coll Health 2008; 56(6): 657-663.
[73] Olff M, de Vries GJ, Güzelcan Y, Assies J, Gersons BP. Changes in cortisol and DHEA plasma levels after psychotherapy for PTSD. Psychoneuroendocrinology 2007; 32(6): 619-626.
ment heading
10.1016/S2221-6189(14)60066-4
*Corresponding author: Professor Manuela Martinez, Department of Psychobiology, Faculty of Psychology, University of Valencia, Avda Blasco Ibañez, 21, 46010 Valencia, Spain.
Tel: 34-963864633
Fax: 34-963864668
E-mail: Manuela.Martinez@uv.es
猜你喜欢
杂志排行
Journal of Acute Disease的其它文章
- Acute and sub-acute toxicity study of Clerodendrum inerme, Jasminum mesnyi Hance and Callistemon citrinus
- Time-critical AMI Detection: A novel and fast technique using the 12-lead ECG
- Epidemiological survey on scorpionism in Gotvand County, Southwestern Iran: an analysis of 1 067 patients
- The acute effect of the antioxidant drug “U-74389G” on red blood cells levels during hypoxia reoxygenation injury in rats
- Successful treatment of lower urinary tract obstruction with peritonealamniotic and vesicoamniotic shunting
- Simvastatin-induced Toxic Epidermal Necrolysis
