Clinical Study on Electroacupuncture for Cervical Intervertebral Disc Herniation
2013-07-18WuYaochiZhangJunfengSunYijunHuangChengfeiShaoPingLiuGuizhen
Wu Yao-chi, Zhang Jun-feng, Sun Yi-jun, Huang Cheng-fei, Shao Ping, Liu Gui-zhen
1 No.6 People’s Hospital Affiliated to Shanghai Jiaotong University, Shanghai 200233, China
2 Shanghai Municipal Hospital of Traditional Chinese Medicine, Shanghai 200070, China
3 Putuo District Center Hospital, Shanghai 200062, China
Clinical Study on Electroacupuncture for Cervical Intervertebral Disc Herniation
Wu Yao-chi1, Zhang Jun-feng1, Sun Yi-jun1, Huang Cheng-fei1, Shao Ping2, Liu Gui-zhen3
1 No.6 People’s Hospital Affiliated to Shanghai Jiaotong University, Shanghai 200233, China
2 Shanghai Municipal Hospital of Traditional Chinese Medicine, Shanghai 200070, China
3 Putuo District Center Hospital, Shanghai 200062, China
Objective: To compare the therapeutic efficacies between electroacupuncture (EA) and medication for cervical intervertebral disc herniation (CIDH).
Methods: Totally 420 patients with CIDH were randomized into two groups by random number table. 210 patients in the EA group were intervened by EA at Dazhui (GV 14), Dazhu (BL 11), and Houxi (SI 3); 210 patients in the medication group were treated by oral administration of Meloxicam tablets.
Results: The average ranks of both short and long term efficacies in the EA group were significantly lower than that in the medication group (bothP<0.01); there were significant differences in comparing the total effective rates of both short and long terms between the two groups (bothP<0.01). It shows that EA group has better therapeutic efficacy than the medication group.
Conclusion: EA is better than medication in comparing both short-term and long-term therapeutic efficacies in treating CIDH.
Intervertebral Disc Displacement; Neck Pain; Acupuncture Therapy; Electroacupuncture
Cervical intervertebral discs are key structures to facilitate head/neck movement and maintain external-internal balance. Normal neck movement relies on good elasticity and flexibility of the nucleus pulposus at the center of the disc. For some reason, when cervical disc protrudes posterolaterally and compresses spinal nerve root or spinal cord and causes symptoms, cervical intervertebral disc herniation (CIDH)[1]will then develop. CIDH can occur at any age, but people aged over 30 and males run a higher risk. Patients usually experience cervical pain accompanied by numbness of upper limbs, which can be relieved by rest in bed but aggravated by activities in upright posture. The symptoms also alter with the movement of cervical disc. A large amount of clinical literatures have proved the significant efficacy of acupuncturemoxibustion in treating CIDH[2-4]. However, we haven’t found any standardized clinical study across the world. There are various uncertainties especially in the acupoint selection, operation of needling manipulations, and the evaluation of therapeutic efficacy. Therefore, since 2010, we have adopted randomized controlled multi- centered large-sampled method to study the clinical efficacy of electroacupuncture (EA) at Dazhui (GV 14), Dazhu (BL 11), and Houxi (SI 3) in treating CIDH, and compared it to the efficacy of oral administration of Meloxicam tablets. The report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria were referring to the diagnostic criteria of CIDH stipulated at the Second Symposium on Cervical Spondylosis in 1993[5]. Cervical pain radiating to upper limbs and aggravated by stretching neck backward, degenerated sensation of the compressed nerve root, abnormal reflex, amyotrophy, decreased muscle strength, limitation of cervical motion, positive brachial plexus traction test and Spurling test; X-ray reveals vertebral hyperplasia, obvious uncovertebral joint hyperplasia, narrowed intervertebral space, and smaller intervertebral foramen; CT shows vertebral paraphyte and narrowed nerve root canal.
1.2 Inclusion criteria
Conforming to the above diagnostic criteria; aged between 30 and 65 years old; with clear consciousness and coordination to help collect clinical materials; willing to participate in the study and having signed the informed consent.
1.3 Exclusion criteria
Cervical spondylosis of other types; with operation indications; with abnormal radiological findings but without cervical symptoms; non-cervical-spine problems majorly manifested by upper-limb pain; bone tumor, osteoporosis, and/or vertebral fusion confirmed by X-ray; pregnancy; other severe diseases; psychological diseases; patients with poor compliance; incomplete clinical materials which may affect the evaluation of therapeutic efficacy.
1.4 Dropout criteria
Severe adverse events that force the study to be terminated; condition aggravated or occurrence of other symptoms that may influence the observation; severe deviations, such as poor compliance during the study making it difficult to evaluate the efficacy; patients asking to quit from the study.
1.5 General data
Totally 420 eligible subjects were enrolled from the outpatients of No.6 People’s Hospital Affiliated to Shanghai Jiaotong University, East Branch of No.6 People’s Hospital, Shanghai Municipal Hospital of Traditional Chinese Medicine, and Putuo District Center Hospital. They were randomized into an EA group and a medication group by the random number table (with a sealed envelope covering the grouping protocol). There were no significant differences in comparing gender, age, and disease duration between the two groups (P>0.05), indicating the comparability (table 1). During treatment, 3 patients in the EA group and 2 in the medication group dropped out because of loss of contact. The procedure of clinical management is shown in Fig.1.
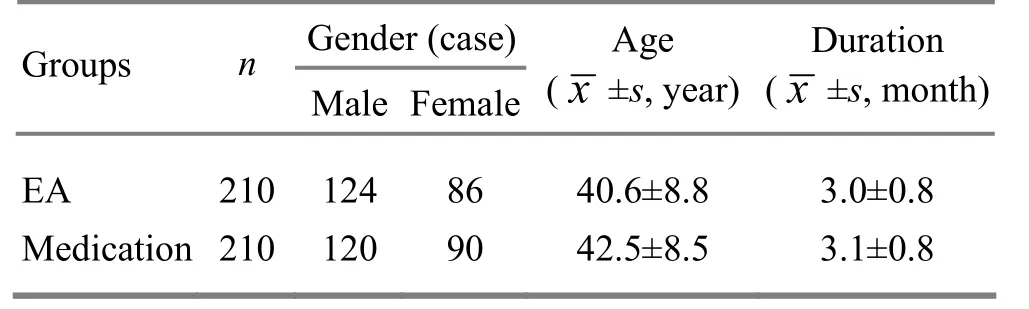
Table 1. Comparison of general data
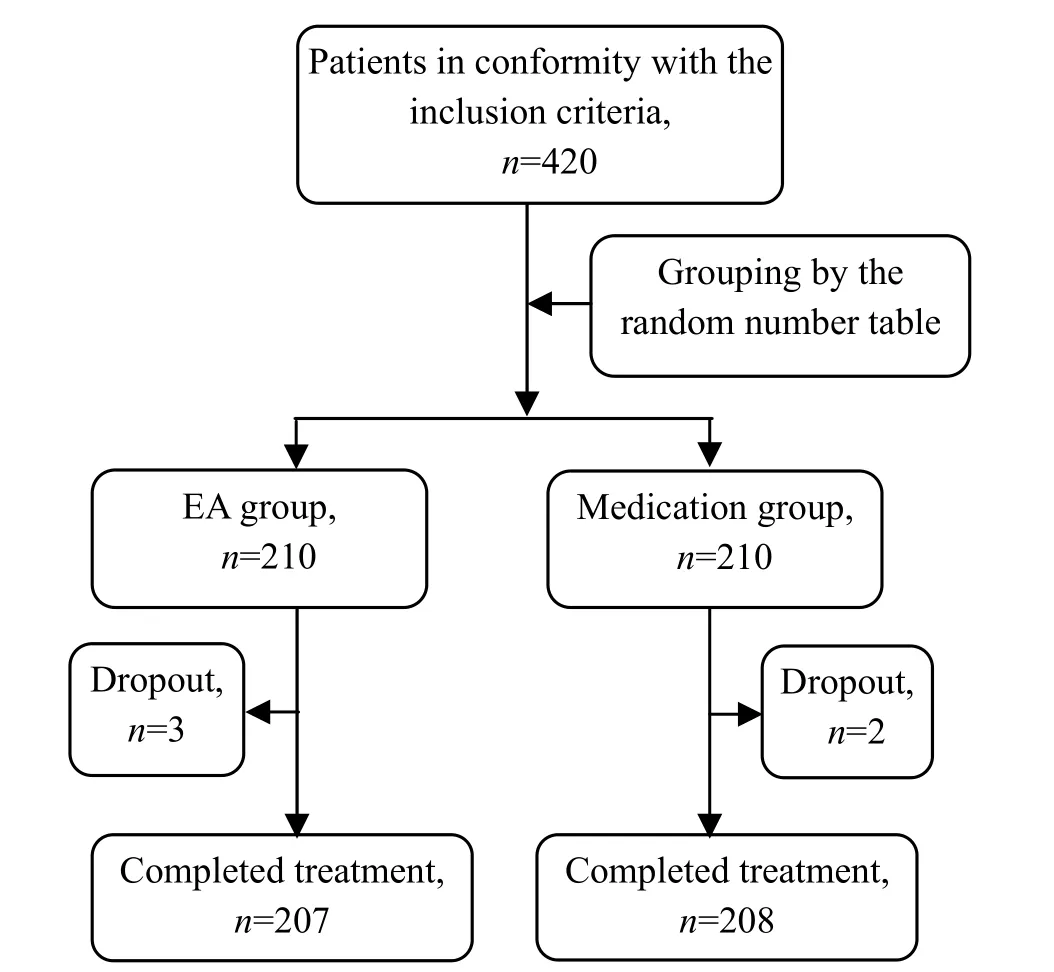
Fig.1 Procedure of clinical management
2 Treatment Methods
2.1 EA group
Acupoints: Dazhui (GV 14), Dazhu (BL 11), and Houxi (SI 3)[6].
Operation: The acupoints were located following the international criteria of acupoint locations. After sterilized by 75% alcohol, the acupoints were punctured by using filiform needles of 0.30 mm in diameter and 40 mm in length. Dazhui (GV 14) was punctured obliquely upward by 0.5-1.0 cun; Dazhu (BL 11) was punctured obliquely towards the spine by 0.5-0.7 cun; Houxi (SI 3) was punctured perpendicularly towards Hegu (LI 4) by 0.5-0.7 cun. When needling sensation was obtained, mild lifting-thrusting manipulations were operated for 1 min each point. The needling sensation at Houxi (SI 3) was required to expand to the whole hand. Dazhui (GV 14) and Dazhu (BL 11) were then connected to the acupoint nerve stimulator [Han’s acupoint nerve stimulator, invented by Peking University Health Science Center, manufactured by Beijing Huawei Industry Development Corporation, qualification No.227066], with continuous wave, frequency at 40 Hz, and current intensity 2 mA, for about 20 min. The treatment was given once per day, 10 sessions as a treatment course, with a day intervalbetween each two courses, for totally 2 treatment courses.
2.2 Medication group
The patients in the medication group were prescribed with Meloxicam tablets, 7.5 mg/tablet, once per day, one tablet each time after dinner, for successive 20 d.
3 Therapeutic Efficacies
3.1 Criteria of therapeutic efficacy
Referring to theShanghai Diagnostic and Therapeutic Guidelines of Traditional Chinese Medicine[7]and the relevant criteria summarized by Sampath P, et al[8], the evaluation was made according to the symptom and sign score, including the following 9 aspects.
Neck and shoulder pain: Absence of pain scored 0; mild pain that didn’t influence life activities scored 1-3; moderate pain that influenced activities but not the independence scored 4-6; severe pain that affected the independence scored 7-9; intolerable intensive pain scored 10.
Cervical tenderness: Absence of pain scored 0; mild tenderness scored 3; moderate tenderness that caused painful expressions (frowning) scored 6; severe tenderness coupled with dodge scored 9.
Upper-limb numbness: No numbness scored 0; occasional numbness which can be relieved rapidly scored 1; consistent numbness that often happened during sleep or in the early morning after getting up but still can be released scored 2; persistent numbness that cannot be released scored 3.
Cervical motion: Lateral flexion, forward flexion, and backward bending ≥40°, side turning ≥75°, scored 0; lateral flexion, forward flexion, and backward bending 30°-39°, side turning 60°-74°, scored 1; lateral flexion, forward flexion, and backward bending 20°-29°, side turning 45°-59°, scored 2; lateral flexion, forward flexion, and backward bending <20°, side turning <45°, scored 3.
Sensory disturbance of upper limb: No sensory disturbance scored 0; mild sensory degeneration scored 1; obvious sensory degeneration scored 2.
Muscle strength of upper limb: Normal muscle strength (degree Ⅴ) scored 0; mild reduction of muscle strength (degree Ⅳ) scored 1; obvious reduction of muscle strength (degree 0-Ⅲ) scored 2.
Tendon reflex: Normal reflex scored 0; decreased reflex scored 1; disappearance of reflex scored 2.
Brachial plexus traction test: Negative scored 0; positive scored 2.
Spurling test: Negative scored 0; positive scored 2.
The total score of the above 9 items ranges from 0 to 35. The higher score represents more significant dysfunction. The decrease rate of the symptom and sign score was used to evaluate the therapeutic efficacy.
Decrease rate of the symptom and sign score = (Pretreatment symptom and sign score – Post-treatment symptom and sign score) ÷ Pre-treatment symptom and sign score × 100%.
A specially assigned trained person was in control of the collection, recording, keeping and analysis of the relevant data. The clinical operators were not involved in the job of evaluation of the therapeutic efficacy.
Recovery: Symptoms were gone, muscle strength was restored to normal level, cervical and limb functions were recovered, patient could go back to work, and the decrease rate of symptom and sign score ≥95%.
Improved: Symptoms were reduced, cervical and limb functions were improved, and the decrease rate of symptom and sign score ≥30%, but <95%.
Invalid: Symptoms were not improved, and the decrease rate of symptom and sign score <30%.
The evaluation of short-term therapeutic efficacy was finished within 21 d after the termination of treatment. The patients were followed up once every month for 6 times via letter and phone to determine the long-term therapeutic efficacy.
3.2 Statistical method
The SPSS 19.0 version software was adopted for data analysis. Fisher’s test was used for the comparison of general information of the two groups. Measurement data such as age and disease duration were analyzed by usingt-test. Enumeration data with normal distribution were analyzed by using Chi-square test, and those with abnormal distribution were by Wilcoxon test.P<0.05 indicated a statistical significance.
3.3 Treatment result
3.3.1 Short-term therapeutic efficacy
The average rank of the short-term therapeutic efficacy in the EA group was significantly lower than that in the medication group (P<0.01), and the total effective rate of the EA group was higher than that of the medication group. It showed that the short-term therapeutic efficacy of the EA group was better than that of the medication group (table 2).
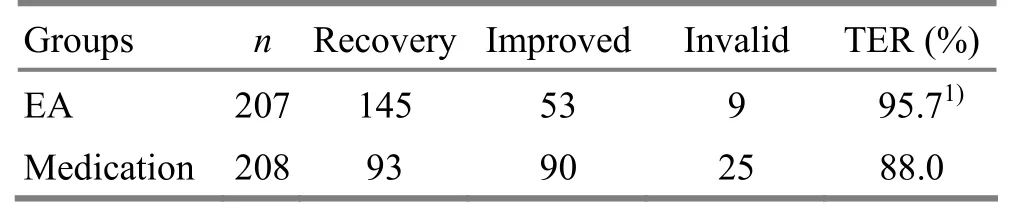
Table 2. Comparison of short-term efficacy (case)
3.3.2 Long-term therapeutic efficacy
The long-term therapeutic efficacy was evaluated after the 6th follow-up study. The average rank of the long-term therapeutic efficacy in the EA group wassignificantly lower than that in the medication group (P<0.01), and the total effective rate of the EA group was higher than that of the medication group. It showed that the EA group had a better long-term therapeutic efficacy compared to the medication group (table 3).
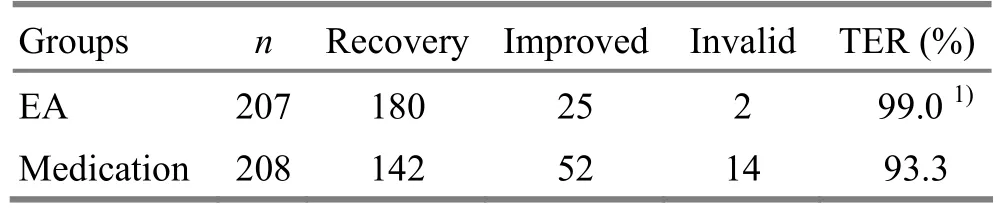
Table 3. Comparison of long-term efficacy (case)
4 Discussion
CIDH falls under the scopes of cervical Bi-Impediment and bone Bi-Impediment in traditional Chinese medicine. It’s either caused by the invasion of cold and wind, blockage of meridians and vessels, and spasm of tendons and vessels; or by liver-kidney deficiency, weak tendons and bones, and loss of control of tendons. Modern medicine holds that CIDH is often caused by acute or repeated mild trauma or strain in addition to the degeneration of cervical disc.
Acupuncture-moxibustion can improve the circulation in neck, soothe and activate the meridians and collaterals, improve the qi activities and kill pain[9]. Dazhui (GV 14) is the crossing point of the Governor Vessel and three yang meridians, governing yang qi of the whole body and boosting the circulation of qi and blood. Dazhu (BL 11) is one of the Eight Influential Points for bones, tonifying liver and kidney and strengthening bones and tendons. Houxi (SI 3) is from the Small Intestine Meridian of Hand Taiyang, working to soothe tendons and unblock collaterals[10-11]. In addition, Houxi (SI 3) is also one of the Confluent Points of the Eight Extraordinary Meridians, connecting to the Governor Vessel, so that it can unblock the meridian qi of the Governor Vessel[12]. The Foot Taiyang Meridian follows the Hand Taiyang Meridian, and meridians can treat the diseases on their paths. Therefore, Houxi (SI 3) is effective for pain on the paths of both Governor Vessel and Foot Taiyang Meridian.
With a randomized controlled multi-centered large-sampled method, this study has shown that the EA group was better than the medication group in comparing both short-term and long-term therapeutic efficacies (P<0.01). It suggests that EA should have a content effect in treating CIDH. Moreover, the operation is easy to be standardized and convenient for promotion in clinic.
[1] Sun SC, Sun ZG. Clinical Orthopaedics and Traumatology. Beijing: People’s Medical Publishing House, 2006: 750.
[2] Xu LB, He YY. The effect of Du Meridian-regulating therapy on immunoglobulins in cervical intervertebral disc herniation. Shanghai Zhenjiu Zazhi, 2011, 30(9): 615-616.
[3] Wang CM, Wu YC, Zhang JF, Huang CF. Observation on efficacy of acupoint injection combined with traction for cervical radiculopathy. J Acupunct Tuina Sci, 2011, 9(6): 380-383.
[4] Cheng SD, Luo JS, Lu NZ, Zhang TW, Hu ZJ, Pu JS, Li W, Xu HL, Wang HF, Huang J. A randomized controlled trial of warm needling moxibustion plus sitting-position pulling and stretching manipulation for the treatment of cervical spondylotic vertebral arteriopathy. Shanghai Zhenjiu Zazhi, 2012, 31(6): 410-413.
[5] Sun Y, Chen QF. The second symposium on cervical spondylosis. Zhonghua Waike Zazhi, 1993, 31(8): 472-476
[6] Cheng XN. Chinese Acupuncture-moxibustion Science. Beijing: People’s Medical Publishing House, 1987: 192-284.
[7] Shanghai Municipal Health Bureau. Shanghai Diagnostic and Therapeutic Guidelines of Traditional Chinese Medicine. 2nd Edition. Shanghai: Publishing House of Shanghai University of Traditional Chinese Medicine, 2003: 386.
[8] Sampath P, Bendebba M, Davis JD, Ducker T. Outcome in patients with cervical radiculopathy: prospective, multicenter study with independent clinical review. Spine (Phila Pa 1976), 1999, 24(6): 591-597.
[9] Chen W, Chen DY, Wu YC, Zhan HS. The clinical research between the manipulation of drawing and stretching in face-upward position and acupuncture on treating cervical spondylopathy. Zhongguo Zhongyi Gushangke Zazhi, 2007, 15(9): 23-24.
[10] Yang L, Pei JC. Function of Houxi (SI 3) and its clinical applications. Zhongyiyao Xuekan, 2004, 22(4): 726, 745.
[11] Yang ZY. Therapeutic observation on the treatment of cervical spondylosis of nerve root type majorly by needling Houxi (SI 3). Shanghai Zhenjiu Zazhi, 2013, 32(1): 34-35.
[12] Li XC, Wang L. Natures of acupoint Houxi (SI 3) and its clinical application. Shanghai Zhongyiyao Zazhi, 2004, 38(5): 44-45.
Translator: Hong Jue
R246.2
A
Date: June 28, 2013
Author: Wu Yao-chi, professor, chief physician, doctoral supervisor.
E-mail: wuyaochi11238@hotmail.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic Efficacy Observation on Combining Herbal Cake-partitioned Moxibustion with Plumblossom Needle Therapy for Cervical Radiculopathy
- Clinical Study on Acupuncture in Treating Perimenopausal Insomnia
- Observation on Clinical Effects of Electroacupuncture Therapy for Apoplexy with Obstructive Sleep Apnea Syndrome
- Clinical Observation on Acupuncture Therapy for Depression at Perimenopause
- Therapeutic Observation on Swift Needling with Fire Needle plus Medication for Herpes Zoster
- Shu-Stream Points for Two Cases with Time-related Disease
