Clinical Study on Acupuncture in Treating Perimenopausal Insomnia
2013-07-18ZhuGuiling
Zhu Gui-ling
Rongcheng Hospital of Traditional Chinese Medicine, Shandong 264300, China
Clinical Study on Acupuncture in Treating Perimenopausal Insomnia
Zhu Gui-ling
Rongcheng Hospital of Traditional Chinese Medicine, Shandong 264300, China
Objective: To observe the clinical efficacy of acupuncture for insomnia in perimenopausal women.
Methods: According to simple randomized controlled principle, sixty female patients with perimenopausal insomnia were randomized into two groups: 30 in the treatment group were intervened by acupuncture and the other 30 in the control group were intervened by taking sleeping pills. Therapeutic efficacies were compared between the two groups at the end of treatment.
Results: The total effective rate was 100.0% in the treatment group versus 83.3% in the control group, and the difference was statistically significant (P<0.05).
Conclusion: Acupuncture has better therapeutic efficacy than taking sleeping pills in treating perimenopausal insomnia.
Acupuncture Therapy; Climacteric Syndrome; Insomnia; Syndrome Differentiation Treatment; Perimenopause Syndrome
In modern society, with more and more women getting involved in social competition, the incidence of perimenopausal insomnia is also constantly increasing. There are many Western medicines for insomnia, but the therapeutic effect is not satisfactory, meanwhile, these medicines may cause side effects or drug dependence. We treated 30 female patients with perimenopausal insomnia, and compared it to the treatment with medication.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria were made based on the diagnostic criteria of insomnia in theChinese Classification and Diagnostic Criteria of Mental Disordersstipulated by Chinese Society of Psychiatry[1]. Sleep disorder is the predominant symptom, and other symptoms, including difficulty falling asleep, light sleep, dream-disturbed sleep, early wake-up, difficulty falling asleep again after wake-up, discomfort after wake-up, lassitude, or daytime fatigue are secondary to sleeplessness; the above sleep disturbances happen at least 3 times a week, constantly for at least 1 month; insomnia has caused clinically significant distress or impairment in social, occupational or other important areas of functioning; it’s due to somatic or psychological disease.
1.2 Grading criteria
It’s referred to theGuiding Principles for Clinical Study of New Chinese Medicines[2].
Mild level: Frequent wake-up during sleep or unsteady sleep, or too early wake-up in the morning. However, work is not influenced.
Moderate level: Sleep duration is less than 4 h, but work can still be sustained.
Severe level: The patient stays up over night and cannot work normally.
1.3 Syndrome types of traditional Chinese medicine
It’s based on theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[3].
Depressed liver qi transforming into fire: Irritation, failure to fall asleep, stuffiness, hypochondriac pain, headache, red face and congestion in eyes, as well as constipation and dark yellow urine. The tongue is red with yellow coating, and the pulse is wiry and rapid.
Internal disturbance of phlegm-heat: Light sleep, irritation and distress, qi-stagnation in chest and stomach, bitter mouth with much phlegm, as well as dizziness and blurred vision. The tongue is red with yellow greasy coating, and pulse is slippery or slippery rapid.
Fire excess due to yin deficiency: Restless, sleepless, or disturbed sleep, heat in palms and soles, dizziness and tinnitus, palpitation, forgetful, red cheekbone and hot flash, dry mouth and lack of saliva. The tongue is red with few coating, and the pulse is thin and rapid.
Deficiency of heart-spleen: Dream-disturbed dream, light sleep, palpitation, forgetful, dizziness, blurred vision, lassitude, pale complexion. The tongue is pale with thin coating, and the pulse is thin and weak.
Heart deficiency with timidity: Dream-disturbed sleep and easy wake-up, palpitation and timidity. The tongue is pale with thin coating, and the pulse is wiry and thin.
1.4 Inclusion criteria
In accordance with the above diagnostic criteria of insomnia; age between 44-55 years old; disease duration within 3-28 months.
1.5 Exclusion criteria
Against inclusion criteria; with severe liver or kidney dysfunction, or in co-morbid with severe diseases of other systems; with severe psychological diseases or malignant tumors; drug addicts; against treatment rules or incomplete medical materials, which will influence the evaluation of therapeutic effects and safety.
1.6 General data
Sixty patients were included from our outpatient and inpatient departments, and then randomized into a control group and a treatment group, 30 each. There were no significant differences in comparing gender, age, disease condition, and syndrome differentiation of traditional Chinese medicine between the two groups (P>0.05).

Table 1. Comparison of general data between the two groups
2 Treatment Methods
2.1 Treatment group
Major acupoints: Yintang (GV 29), Baihui (GV 20), Sishencong (EX-HN 1), Shenmen (HT 7), Neiguan (PC 6), Anmian [midpoint between Yiming (EX-HN 14) and Fengchi (GB 20)].
Adjunctive acupoints: Pishu (BL 20) was added for deficiency of both heart and spleen; Xingjian (LR 2) and Zuqiaoyin (GB 44) for depressed liver qi transforming into fire; Fenglong (ST 40) and Zhongwan (CV 12) for internal disturbance of phlegm-heat; Danshu (BL 19) and Ganshu (BL 18) for Heart deficiency with timidity.
2.2 Control group
The control group was given Diazepam at 2.5 mg, once per day before sleep, and Oryzanol at 30 mg, three times per day.
For both groups, 10-day treatment was considered as a treatment course, and there was a 2-day interval between two courses. They were compared after 3 treatment courses.
3 Therapeutic Efficacies
3.1 Criteria of therapeutic efficacy
It’s based on the criteria of therapeutic effects in treating insomnia in theGuiding Principles for Clinical Study of New Chinese Medicines[2].
Recovery: Sleep duration is restored to normal level, or sleep duration is over 6 h, and sleep is deep and refreshing.
Marked effect: Sleep is obviously improved, sleep duration increases by over 3 h, and sleep is deeper.
Effective: Symptoms are improved, and sleep duration increases by less than 3 h.
Failure: Sleep is not improved or the condition is exacerbated after treatment.
3.2 Treatment result
According to statistical analysis, there was a significant difference between the two groups in the total effective rate (P<0.05), and the treatment group is superior to the control group (table 2).
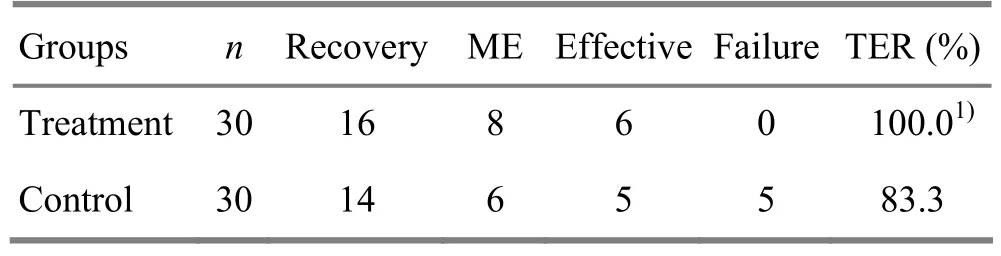
Table 2. Comparison of therapeutic efficacy (case)
4 Discussion
Perimenopausal insomnia can be seen in perimenopausal syndrome and sleeplessness. Traditional Chinese medicine holds that this disease is usually caused by imbalance of the Thoroughfare and Conception Vessels, dysfunction of Zang-fu organs, and yin-yang imbalance. Therefore, the disharmony and failure of interaction between yin and yang is the original reason of insomnia, and thus regulating yin-yang and calming mind is the major treatment method for this disease.
There are profound reports on acupuncturemoxibustion for perimenopausal syndrome, but only a few of them are on perimenopausal insomnia[4-10]. Longterm administration of Western medications often leads to drug resistance, dependence, and addiction. This study has found that acupuncture has higher total effective rate than taking sleeping pills for perimenopausal insomnia, meanwhile without adverse reactions, and it’s easily accepted by patients.
[1] Chinese Society of Psychiatry. Chinese Classification and Diagnostic Criteria of Mental Disorders. 3rd Edition. Jinan: Shandong Science & Technology Press, 2001: 118.
[2] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: People’s Medical Publishing House, 1993: 186.
[3] State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Nanjing: Nanjing University Press, 1994: 19.
[4] Li Y, Xia Y, Liu SM, Ju ZY, Shi XL, Chen MG, Cheng L, He JS. Effect of electroacupuncture on serum sex hormones in patients with perimenopausal syndrome. Shanghai Zhenjiu Zazhi, 2010, 29(4): 199-201.
[5] Sun ZL, Jin YP, Jin HF. A multicenter observational study of the clinical efficacy of ear acupuncture in treating perimenopausal syndrome. Shanghai Zhenjiu Zazhi, 2010, 29(4): 209-211.
[6] Li Y, Xia Y, Liu SM, Ju ZY, Shi XL, Chen MG, Cheng L, He JS. Effect of electroacupuncture on kupperman index scores in patients with perimenopausal syndrome. Shanghai Zhenjiu Zazhi, 2009, 28(10): 559-561.
[7] Ma XP, Wu FD, Shan YH. Clinical observation on treating menopause syndrome with acupuncture therapy. J Acupunct Tuina Sci, 2009, 7(1): 51-54.
[8] Liu H, Yang DN. Clinical observations on treatment of 86 peri-climacteric syndrome cases by point catgut embedding. Shanghai Zhenjiu Zazhi, 2007, 26(2): 5-7.
[9] Chen QB. Clinical research progress of acupuncturemoxibustion in treating perimenopausal syndrome in women. Yixue Xinxi, 2009, (10): 138-139.
[10] Liu DH. Observations on the efficacy of acupuncture and moxibustion plus psychotherapy in treating female climacteric syndrome. Shanghai Zhenjiu Zazhi, 2009, 7(5): 315-320.
Translator: Hong Jue
R246.6
A
Date: July 12, 2013
Author: Zhu Gui-ling, associate chief physician.
E-mail: zjtnyx@126.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Shu-Stream Points for Two Cases with Time-related Disease
- Therapeutic Observation on Swift Needling with Fire Needle plus Medication for Herpes Zoster
- Tuina Is Superior to Electroacupuncture in Treating Thoracic Facet Joint Disorder
- Clinical Study on Electroacupuncture for Cervical Intervertebral Disc Herniation
- Therapeutic Efficacy Observation on Combining Herbal Cake-partitioned Moxibustion with Plumblossom Needle Therapy for Cervical Radiculopathy
- Clinical Observation on Acupuncture Therapy for Depression at Perimenopause
