Therapeutic Observation on Swift Needling with Fire Needle plus Medication for Herpes Zoster
2013-07-18FanYujiangLiuQingguoYinGaizhen
Fan Yu-jiang, Liu Qing-guo, Yin Gai-zhen
1 Xinjiang Urumqi Hospital of Traditional Chinese Medicine, Urumqi 830000, China
2 Beijing University of Traditional Chinese Medicine, Beijing 100029, China
3 School of Traditional Chinese Medicine, Xinjiang Medical University, Urumqi 830000, China
Therapeutic Observation on Swift Needling with Fire Needle plus Medication for Herpes Zoster
Fan Yu-jiang1, Liu Qing-guo2, Yin Gai-zhen3
1 Xinjiang Urumqi Hospital of Traditional Chinese Medicine, Urumqi 830000, China
2 Beijing University of Traditional Chinese Medicine, Beijing 100029, China
3 School of Traditional Chinese Medicine, Xinjiang Medical University, Urumqi 830000, China
Objective: To discuss the effectiveness and safety of swift needling with fire needle plus medication in treating herpes zoster and the change of substance P.
Methods: Seventy-nine patients with herpes zoster were selected and randomized into a fire-acupuncture group (41 cases) and a Westernmedication group (38 cases). The fire-acupuncture group was intervened by swift needling with fire needle, and simultaneously prescribed with Valaciclovir Hydrochloride tablets and Vitamin B1; the Western-medication group was by the same oral medicines alone. The therapeutic efficacies were evaluated afterwards.
Results: The total effective rate was 95.1% in the fire-acupuncture group versus 89.5% in the Western-medication group, and the difference was statistically significant (P<0.05). After treatment, the concentration of substance P and visual analogue scale (VAS) score dropped significantly in both groups (bothP<0.05); the inter-group differences were statistically significant (bothP<0.05).
Conclusion: Swift needling with fire needle plus medication has better therapeutic efficacy than medication alone in treating herpes zoster.
Acupuncture Medication Combined; Fire-needle Therapy; Herpes Zoster; Pricking Needling
Herpes zoster is a painful, blistering skin rash (often in a stripe) caused by viral infection. The virus may spread from one or more ganglia along nerves of an affected segment and affect the corresponding dermatome. Signs and symptoms along the skin lesion include hyperesthesia, a burning sensation, numbness and pricking pain. In some cases, this condition may cause restlessness, poor appetite and difficulty falling asleep, thus greatly affecting the patients’ quality of life. The corresponding term in the traditional Chinese medicine (TCM) is snake-like sores. We adopted swift needling with fire needle to treat 41 cases of herpes zoster, compared to a control group of 38 cases treated with Western medicine. It is now reported as follows.
1 Clinical Materials
1.1 Diagnostic criteria
It’s referred to the diagnostic criteria of the snake-like sores in theCriteria of Diagnosis and Therapeutic Effect of Diseases and Syndromes in Traditional Chinese Medicine. Lesions are mostly mung-bean-sized blisters in stripes and clusters on one side of the body, with tight wall and red base. Bleeding and gangrene may appear in severe cases. Cases with lesions on headare often severe. Before the occurrence of blisters, there first appears pricking pain or burning pain on skin, possibly coupled with general discomfort and fever. The pain is obvious and insufferable. There may also appear postherpetic pain.
1.2 Inclusion criteria
Conforming to the diagnostic criteria of herpes zoster; aged 18-70; with blisters on surface of the body; without use of antivirus and analgesic treatments in 10 d after the onset.
1.3 Exclusion criteria
The special types, including herpes zoster in eye and ear, internal organs, and meninges, generalized zosters, and the one without blisters; women in pregnancy or lactation period; complications of cardiovascular or cerebrovascular diseases, diseases of liver, kidney, or hematopoietic system, diabetes, malignant tumor, mental disease, connective tissue disease, hemophilia, and bleeding tendency; critical condition under which it’s difficult to evaluate the efficacy and safety of the treatment; use of corticosteroid hormone or immunosuppressant in the recent 1 month.
1.4 General data
Seventy-nine subjects were from the outpatients of the Dermatology and Acupuncture Departments, Xinjiang Urumqi Hospital of Traditional Chinese Medicine. By the visiting sequence and random number table, they were randomized into a fireacupuncture group (41 cases) and a Westernmedication group (38 cases). In the fire-acupuncture group, there were 18 males and 23 females, aged 18-70 years, averaged at (46±15) years, and the mean duration was (5.04±1.14) d. In the Western-medication group, there were 20 males and 18 females, aged 21-70 years, averaged at (45±14) years, and the mean duration was (4.87±1.06) d. There were no significant differences between the two groups in comparing age and disease duration (P>0.05), indicating the comparability.
2 Treatment Methods
2.1 Fire-acupuncture group
2.1.1 Fire-acupuncture treatment
Points: Ashi points (1 cm away from the outer edge of the shingles).
Operation: The patient first took a proper position to expose the lesions. Use an alcohol lamp to fire a needle of 0.35 mm in diameter and 25 mm in length. When half burnt red, the needle was swiftly punctured into the Ashi points (surrounding the shingles with an interval of 1 cm) by depth of 3-5 mm. The needle should be fired every time before puncturing. The blisters in clusters were also pricked by the fire needle and the effusion should be wiped away. The patient was treated on the first day, and observed on the following two day to see whether there were new blisters. The new blisters should be treated in the same way. If there were no new blisters, the doctor should carefully search the missed ones and treat them with the fire needle.
Caution: Choose needles of good quality and pay attention to the heating time.
2.1.2 Medication treatment
Valaciclovir Hydrochloride tablets, 0.3 g each time, twice a day, taken on an empty stomach. Vitamin B1tablets, 10 mg each time, three times a day. The medicines were taken from the first visiting day, for continuous 10 d.
2.2 Western-medication group
The oral medicines were taken in the same way as in the fire-acupuncture group.
The two groups both took a 10-day treatment course, and then the therapeutic efficacies were evaluated.
3 Therapeutic Efficacy
3.1 Pain evaluation
The visual analogue scale (VAS) invented by the Pain Society of Chinese Medical Association was adopted. Draw a line of 10 cm on a white paper and mark the two ends with ‘painless’ and ‘severe pain’. The patient was asked to mark on the line according to their own feeling of pain to express the pain intensity. The distance between the beginning and the mark stood for the level of pain.
3.2 Criteria of therapeutic efficacy
The therapeutic efficacy was evaluated according to the therapeutic efficacy index.
Therapeutic efficacy index = (Pre-treatment pain score – Post-treatment pain score) ÷ Pre-treatment pain score × 100%.
Cured: Lesions were basically gone, pain was relieved, and the therapeutic efficacy index was equal or more than 90%.
Remarkable effect: The therapeutic efficacy index was 50%-89%.
Improved: The therapeutic efficacy index was 20%-49%.
Invalid: The therapeutic efficacy index was less than 20%.
3.3 Observation indexes
On the first visit (before treatment) and the 11th day after onset (after treatment), 3 mL morning blood was drawn from the elbow of the same side to test the concentration of substance P.
Add 0.5 mol/L Natrium Adetate 30mL and Aprotinin 1 500 KIU to the blood; centrifuge the plasma for 15 min (2 000 r/min); add 2 mL cold Acetone (4 ℃) to 1 mL plasma and mix them well;centrifuge the mixture at 4 ℃ (2 000 r/min) for 20 min; separate the supernatant and add 4 mL cold Petroleum Benzin to it and then centrifuge the mixture again; clean away the supernatant and blow away the residual Acetone with a fan. The rest liquid was dried by a freeze dry machine, and then sealed and placed at–20℃ for detection. For the long time taken for case collection, the blood of the previous patients was kept at –70℃ (no freeze thawing).
Substance P was tested by using radioimmunity. The kits were purchased from the Beijing Radioimmunity Technique Center of Navy. The automatic gamma counter was produced by Xi’an 262 Factory.
3.4 Statistical method
The SPSS 13.0 statistic software was used for statistical analysis. The enumeration data were analyzed by Chi-square test, and the measurement data were byt-test.
3.5 Treatment result
3.5.1 Comparison of pain
The inter-group difference in evaluating pain was statistically insignificant before treatment (P>0.05); after treatment, the pain scores were reduced in both groups (P<0.05), but the improvement in the fire-acupuncture group was better, and the inter-group difference was statistically significant (P<0.05), indicating that the fireacupuncture group should have a better effect than the Western-medication group in improving pain (table 1).
Table 1. Comparison of VAS score (, point)
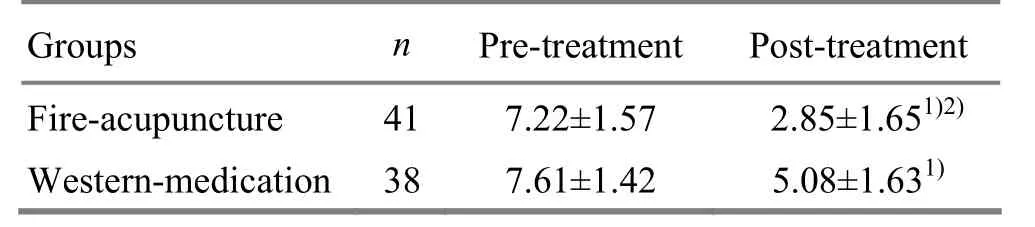
Table 1. Comparison of VAS score (, point)
Note: Intra-group comparison with the result before treatment, 1)P<0.05; compared to the Western-medication group after treatment, 2)P<0.05
Fire-acupuncture 417.22±1.57 2.85±1.651)2)Western-medication387.61±1.42 5.08±1.631)
3.5.2 Comparison of clinical efficacy
The total effective rate was 95.1% in the fireacupuncture group versus 89.5% in the Westernmedication group, and the difference was statistically significant (P<0.05), indicating that the fire-acupuncture group should have a better clinical efficacy than the Western- medication group (table 2).

Table 2. Comparison of clinical efficacy (case)
3.5.3 Comparison of the concentration of substance P
The inter-group difference was statistically insignificant in comparing the concentration of substance P (P>0.05); both groups achieved significant improvements in the concentration of substance P after treatment (P<0.05), but the improvement in the fire-acupuncture group was better (P<0.05), indicating that the improvement of the concentration of substance P in the fire-acupuncture group should be better than that in the Western-medication group (table 3).
Table 3. Comparison of the concentration of substance P (, pg/mL)
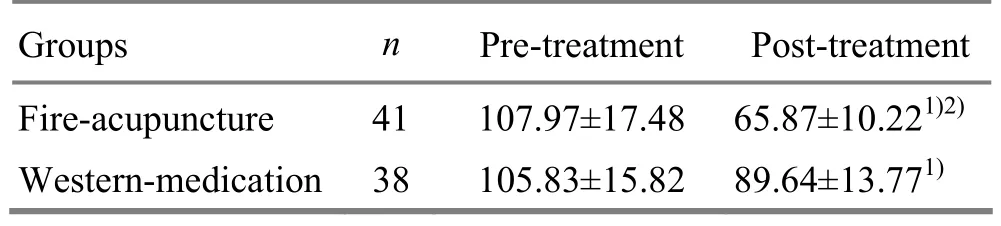
Table 3. Comparison of the concentration of substance P (, pg/mL)
Note: Inner-group comparison, 1)P<0.05; compared to the Western-medication group after treatment, 2)P<0.05
GroupsnPre-treatment Post-treatment Fire-acupuncture 41 107.97±17.48 65.87±10.221)2)Western-medication 38 105.83±15.82 89.64±13.771)
4 Discussion
Modern medicine believes that herpes zoster is caused by the infection of varicella zoster virus. It’s reported that the initial infection of the virus can cause chicken pox, but the virus can remain latent in the nerve cells of the dorsal root for years[1]. When the immune system is compromised, with the stimulation of various inducing factors, the virus will become active again and proliferate, leading to shingles and neuralgia in the dermatome. Most researches show that the incidence rate of herpes zoster increases with the age. It’s commonly treated with antiviral drugs. Valaciclovir Hydrochloride tablet is a kind of nucleotide antivirus and can resist the replication of the virus[2]. It works by competitively inhibiting the DNA polymerases of the virus and getting into the DNA of the virus and host cells to finally stop the extension of the virus DNA[3]. However, it costs high and may induce adverse effects. Inflammation and lesions induce the activation and sensitivity of nociceptors, and then cause the center to become highly excited[4], finally inducing the postherpetic neuralgia. It’s proved by many studies that severe rush and pain at the acute stage and the precursor pain before the occurrence of rush are the risk factors of postherpetic neuralgia. The pathological researches have proved the loss of nerve fibers or cells of peripheral nerves, posterior root ganglion, and spinaldorsal horn[5]. Substance P is a kind of neurogenic inflammation mediator. In the inflammation of spinal nerve root, the degranulation of mast cells will promote the release of substance P, directly stimulate the peripheral nociceptors of lesions, and finally induce the pain[6]. Substance P is a crucial chemical transmitter in the transmission of pain signal from the peripheral tissues to the central nerve system[7]. Li JH, et al[8]also reported that the concentration of substance P is in proportion to the intensity of pain.
As an important part of acupuncture-moxibustion therapy, fire-needle therapy has existed for thousands of years. It’s recorded as early as in the Spiritual Pivot that fire-needle therapy is used to treat Bi-Impediment syndrome. Herpes zoster is majorly due to the residence of wind and fire in Shaoyang and Yangming Meridians, dampness retained in Taiyin and Yangming Meridians, emotional impairment, fire in liver and gallbladder, or blockage of meridians and collaterals. Treating toxic heat with fire-needle therapy conforms to the treatment principle in theHuang Di Nei Jing(Yellow Emperor’s Classic of Internal Medicine) that to reduce the excess and to unblock the stagnation. Fire-needle therapy acts to induce out the toxin, unblock the collaterals to kill pain, drive away wind and disperse the pathogens, and clear away dampness and heat from liver and gallbladder. Therefore, to treat herpes zoster with fire-needle therapy at the early stage can promote the healing of blisters, shorten the duration, and prevent postherpetic neuralgia. Fire-needle therapy is currently an important method in acupuncture clinic. The domestic researches[9-10]indicate that the severe rush at the acute stage, usually runs a higher risk of developing postherpetic neuralgia; swift needling with fire needle can promote the healing of blisters and prevent the happening of postherpetic neuralgia.
Generally speaking, swift needling with fire needle in treating herpes zoster can promote the healing of blisters, shorten the disease duration, relieve the pain at acute stage, reduce the production of substance P, down-regulate the concentration of substance P, and avoid the happening of hypersensitivity of posterior nerve root of spinal cord and the postherpetic neuralgia.
[1] Zhang B, Wang ZQ, He JM, Hu YD. Effect of antiviral therapy combined with analgesics for the treatment of herpes zoster pain. Zhongguo Tengtong Yixue Zazhi, 2006, 12(3): 153-156.
[2] Li Q, Liu Y, Xue WH, Zhang WX, Wang BZ. Therapeutic observation on three methods in treating herpetic neuralgia. Zhongguo Pifu Xingbing Xue Zazhi, 2005, 19(8): 480-482.
[3] Jia DM, Su HH, Zhang Y, Li LL, Sun Y, Luo QL. An open multi-center clinical trial of Ganciclovir of the treatment of herpes zoster. Zhongguo Pifu Xingbing Xue Zazhi, 2006, 20(9): 538-539.
[4] Schader K. Herpes zoster in cycle adult. Clininfeel Dis, 2001, 32(10): 1481-1485.
[5] Chen Y. Research progress of the pathogenesis and treatment of postherpetic neuralgia. Guowai Yixue: Pifu Xingbing Xue Fence, 2002, 28(1): 49-51.
[6] Bethea CL, Hess DL, Widmann AA, Henningfeld JM. Effects of progesterone on prolactin, hypothalamic beta-endorphin, hypothalamic substance P, and midbrain serotonin in guinea pigs. Neuroendocrinology, 1995, 61(6): 695-703.
[7] Ruan HZ, Li XC, Cai WQ, Li HD, Zhao BY, Zhang X. Substance P involved into the expression of spinal c-fos induced by noxious stimulus. Kexue Tongbao, 1994, 39(13): 1237-1240.
[8] Li JH, Guo YJ, Shang YB, Di L, Zhai N, Song FJ. Test of three plasma neuropeptides in elderly patients with herpes zoster. Zhonghua Pifubing Zazhi, 2006, 39(7): 410.
[9] Liu GW, Wang YH, Liu XK. Clinical and pathological study on the trigeminal neuralgia following herpes zoster. Zhongguo Tengtong Yixue Zazhi, 2001, 7(3): 133-135.
[10] Wang JS, Zhu YP. Long term follow up of the therapeutic effect on postherpetic neuralgia. Zhongguo Tengtong Yixue Zazhi, 2001, 7(3): 136-139.
Translator: Hong Jue
R246.7
A
Date: April 16, 2013
Author: Fan Yu-jiang, associate chief physician.
E-mail: zjtnyx@126.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic Efficacy Observation on Combining Herbal Cake-partitioned Moxibustion with Plumblossom Needle Therapy for Cervical Radiculopathy
- Clinical Study on Acupuncture in Treating Perimenopausal Insomnia
- Observation on Clinical Effects of Electroacupuncture Therapy for Apoplexy with Obstructive Sleep Apnea Syndrome
- Clinical Observation on Acupuncture Therapy for Depression at Perimenopause
- Tuina Is Superior to Electroacupuncture in Treating Thoracic Facet Joint Disorder
- Shu-Stream Points for Two Cases with Time-related Disease
