Observation on Clinical Effects of Electroacupuncture Therapy for Apoplexy with Obstructive Sleep Apnea Syndrome
2013-07-18WangYinGengHuiyaoYeYongmingLiJia
Wang Yin, Geng Hui-yao, Ye Yong-ming Li Jia
1 Acupuncture Department of Guang’anmen Hospital, China Academy of Chinese Medical Science, Beijing 100053, China
2 School of Acupuncture and Tuina, Beijing University of Traditional Chinese Medicine, Beijing 100029, China
3 Lugouqiao Health Service Center of Fengtai District, Beijing 100165, China
Observation on Clinical Effects of Electroacupuncture Therapy for Apoplexy with Obstructive Sleep Apnea Syndrome
Wang Yin1,2, Geng Hui-yao1,2, Ye Yong-ming1, Li Jia3
1 Acupuncture Department of Guang’anmen Hospital, China Academy of Chinese Medical Science, Beijing 100053, China
2 School of Acupuncture and Tuina, Beijing University of Traditional Chinese Medicine, Beijing 100029, China
3 Lugouqiao Health Service Center of Fengtai District, Beijing 100165, China
Objective: To observe the clinical effect of electroacupuncture (EA) for stroke with obstructive sleep apnea syndrome (OSAS).
Methods: Thirty cases in conformity with the diagnostic criteria were selected and treated by EA. Before treatment and four weeks after treatment, nocturnal polysomnography, Epworth sleeping scale (ESS), National Institutes of Health stroke scale (NIHSS) were assessed. Two years after treatment, ESS was assessed and the relevant symptoms were examined.
Results: Twenty-one cases completed the observation and 9 cases dropped out. In the 21 cases after treatment, apnea hyponea index (AHI) decreased obviously (P<0.05), and the lowest oxyhemoglobin saturation (SaO2) increased obviously in sleep (P<0.05) and ESS score decreased obviously (P<0.05). NIHSS score didn’t improve obviously (P>0.05). In the follow-up examination two years later, 16 cases completed the observation and 5 cases dropped out. In the 16 cases, ESS score didn’t obviously improve in comparison of those before treatment and four weeks after treatment (bothP>0.05).
Conclusion: EA therapy for stroke with OSAS can reduce AHI, and enhance the lowest SaO2in sleep and improve the clinical symptoms of the patients. In the follow-up examinations two years after treatment, the long-term effect was not obvious.
Acupuncture Therapy; Electroacupuncture; Stroke; Sleep Apnea, Obstructive; Polysomnography
Stroke is a group of acute cerebrovascular diseases jointly characterized by sudden onset and focal neurological deficits. In recent years, a large number of materials have shown that stroke is closely related to sleep apnea syndrome (SAS). We treated stroke with obstructive sleep apnea syndrome (OSAS) with electroacupuncture (EA) and observed the short-term and long-term effects. Now, the report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria of stroke
In reference to the diagnostic criteria stipulated at the Fourth National Conference on Cerebrovascular Diseases[1], cerebral infarction or cerebral hemorrhage was confirmed by cranial CT or MRI.
1.1.2 Diagnostic criteria of OSAS
The diagnostic criteria of OSAS met theDiagnostic and Therapeutic Guidelines for Obstructive Sleep Apnea Syndrome(draft) stipulated by the Academic Group of Sleep Breath Disorder, Society of Respiratory Diseases of Chinese Medical Association[2]. Typical snoring during sleep at night and irregular breathing, excessive somnolence in daytime; polysomnography (PSG) monitoring showed that apnea and hypopnea appeared repeatedly for 30 times during 7-hour sleep every night or apnea hyponea index (AHI) was larger or equaled to five times every hour. By AHI, OSAS was divided into three grades, 5-20 times/h was mild grade, 21-40 times/h was medium grade and >40 times/h was severe grade. Oxyhemoglobin saturation (SaO2) between 85 and 89 was mild condition, between 90-84 was medium condition and less than 80 was severe condition.
1.2 Exclusive criteria
Those patients unable to go on with PSG monitoring, and those patients unable to continue electroacupuncture treatment due to various reasons.
1.3 General data
All the selected 30 cases came from the Acupuncture Department of Guang’anmen Hospital, China Academy of Chinese Medical Science, from July to December of 2008. The duration of stroke with OSAS was more than two weeks, but less than six months.
In the study, 9 cases were rejected, including 8 cases discharged from the hospital due to less than four weeks of EA treatment and unable to continue EA treatment after discharge, and 1 case discharged from the hospital after four weeks of EA treatment and unable to check PSG. In the 21 cases completed treatment and observation, there were 17 males and 4 females, with the age ranging from 46-80 years old, at the average age of (61±2), and with the average body mass index (BMI) at (26.72±0.79) kg/m2, including 10 cases in severe condition, 9 cases in medium condition and 2 cases in mild condition.
In the follow-up examinations of 21 cases by telephone calls two years after the treatment, 16 cases completed examinations, including 12 males and 4 females, with the age ranging from 50-82 years old, at the average age of (64±3), and including 9 severe cases, 6 medium cases and 1 mild case. Five cases dropped out, because telephone calls were not connected.
2 Research Methods
2.1 Treatment methods
Acupoint: Lianquan (CV 23).
Operation: After routine disinfection of the skin at the acupoint area, the filiform needle of 0.30 mm in diameter and 75 mm in length was slowly inserted toward the tongue root obliquely for 40-60 mm, till the patient had a numb and distending sensation in the throat. Another needle was inserted into a non-acupoint spot [20 mm lateral to Lianquan (CV 23)] shallowly (for 20 mm). Then, the handles of the two needles were connected with Great Wall KWD-808 Pulsation Apparatus, with continuous wave, 2 Hz frequency and current intensity within the patient’s tolerance. The stimulation was given for 30 min each time. The treatment was given five times per week, for totally four weeks (twenty sessions).
2.2 Observation indexes
2.2.1 PSG evaluation
The standard polysomnographic recording technology of HypnoPTT Sleep Monitor produced by U.S Tyco International Ltd. was used to monitor sleep before and after treatment. The indexes automatically recorded with the signals of nasal airflow, pulse transit time (PTT), SaO2, ECG, respiratory effort degrees, snoring, and body position were processed by computer, and the conclusion was achieved by manual analysis of the materials.
2.2.2 Score of National Institute of Health stroke scale (NIHSS)[3]
NIHSS scores were assessed respectively before and after treatment.
2.2.3 Evaluation of Epworth sleeping scale (ESS)[4]
ESS was evaluated respectively before the treatment, after the treatment, and two years after the treatment.
2.2.4 Follow-up examination of relevant symptoms
Two years after treatment, the conditions of blood pressure, heart rhythm, with or without esophageal reflux, numbers of nocturia, and recurrence of stroke were followed up.
2.3 Statistical methods
All the data were processed by the SPSS 11.5 version statistic software under Windows XP. The measurement data were processed by the selfcontrolled pairedt-test between before and after treatment.
3 Results
The degrees of AHI improvement were used as the evaluation criteria for the short-term clinical effects. After the treatment, AHI decreased obviously (P<0.05), at 7.34 times/h on average. After treatment, the lowest oxyhemoglobin saturation (SaO2) value during sleep obviously increased (P<0.05). Before treatment, in terms of the lowest SaO2value during sleep, there were 9 severe cases, 8 medium cases and 4 mild cases, and after the treatment, there were 8 severe cases, 4 medium cases, 7 mild cases and 2 cases restored to normal level. The grades of the lowest SaO2valueobviously decreased. After treatment, ESS score obviously decreased (P<0.05), and the clinical symptoms were remarkably improved. There was no obvious improvement in NIHSS score (P>0.05), (table 1).
Table 1. Changes in various indexes after treatment ()
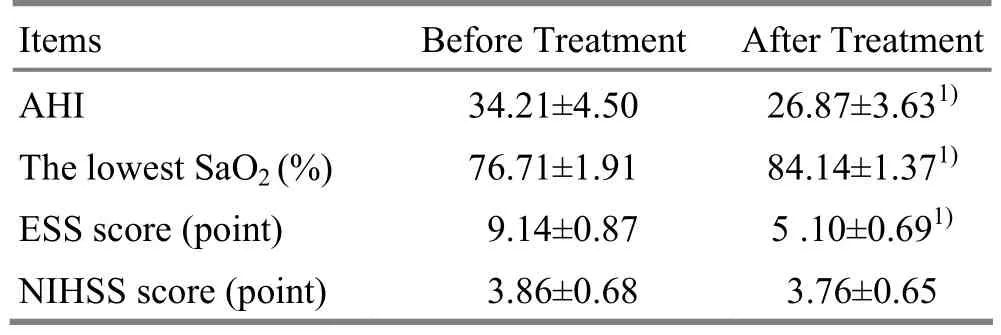
Table 1. Changes in various indexes after treatment ()
Note: In comparison with before treatment, 1)P<0.01
Items Before Treatment After Treatment AHI 34.21±4.50 26.87±3.631)The lowest SaO2(%) 76.71±1.91 84.14±1.371)ESS score (point) 9.14±0.87 5 .10±0.691)NIHSS score (point) 3.86±0.68 3.76±0.65
ESS score was used as one of the criteria for the long-term clinical effects. Please see Fig.1 for follow-up results two years after the treatment. In the 16 cases completed the follow-up examinations, ESS score was (8.56±5.10) before treatment and (5.44±3.35) after treatment, and were (8.69±6.30) two years after the treatment. There was no statistical significance in difference between the ESS score of the follow-up examination and that of before and after treatment (P>0.05). After treatment, ESS score changed obviously in comparison with that of before treatment, increased in the cases with less than 10 points and obviously decreased in the cases with more than 10 points and 15 points. But, in the patients two years after the treatment, the cases with ESS score more than 10 points and 15 points increased, and the cases with less than 10 points decreased. Because ESS score was in certain positive correlation with SAS severity, it can be seen that somnolence degree was somewhat improved after the treatment than before the treatment in the patients of the follow-up examination, and somnolence was aggravated two years after treatment.
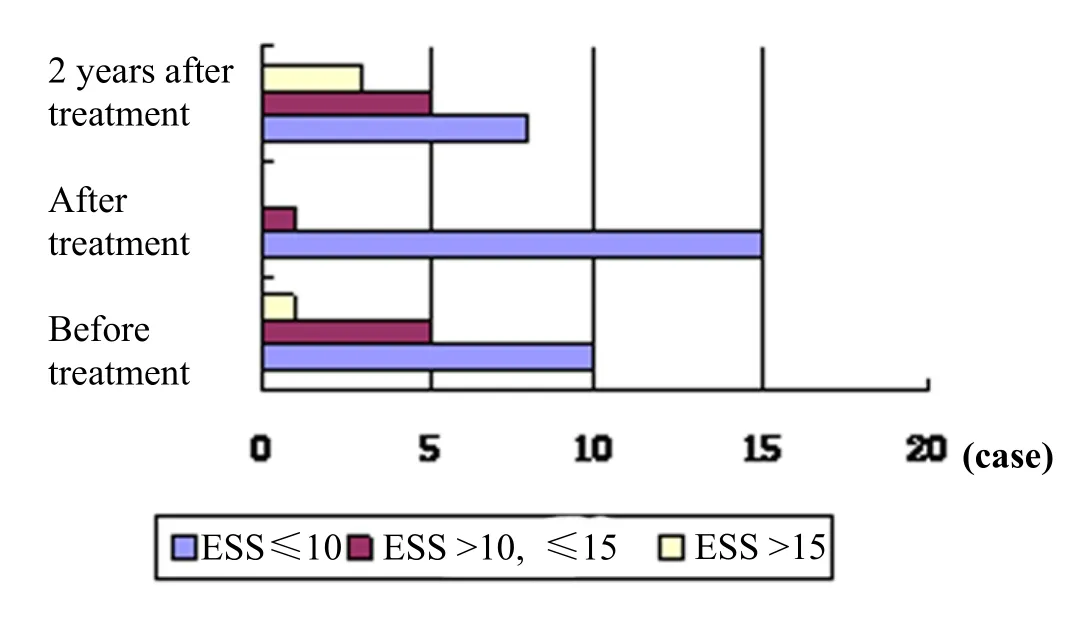
Fig.1 Change of ESS score
In the relevant clinical symptoms, all 16 cases had no recurrence of stroke, with number of nocturia in 2-4 times and good control of blood pressure. Fifteen cases had no esophageal reflux. 15 cases showed normal heart rhythm, and 1 case showed arrhythmia.
It was indicated in the research results that four weeks after EA treatment on Lianquan (CV 23), the patient’s AHI decreased and the lowest SaO2value during sleep increased, and the clinical symptoms of irregular snoring, sleep apnea, suffocated breathing, somnolence in daytime, lassitude, and difficulty concentration were improved. But, the results of the follow-up examination two years after the treatment showed that the long-term clinical effects were not obvious.
4 Discussion
OSAS is the most common category of SAS. The most commonly obstructive position is the throat. It is believed in modern medicine that there are the hypoglossal nerve, glossopharyngeal nerve and branches of the glossopharyngeal nerve under Lianquan (CV 23). During sleep, the pharyngeal portion repeatedly collapses, causing the obstruction of the upper airway, mainly in the soft palate and the airway behind the tongue[5-6]. In the patients with stroke and SAS, the activities of the tongue muscles, throat muscles, genioglossus muscles decrease and are unable to balance the negative pressure inside the airway. Moreover, the backward fall of the tongue is easy to induce the obstruction in the upper airway. In this study, it is able to function on the hypoglossal nerves and muscles under Lianquan (CV 23), intensify the contraction of the throat muscles, maintain certain tenacity of the lumen, move the tongue forward with the dilator muscles of the upper airway, predominantly the genioglossus muscles, and open the airway behind the tongue effectively, so as to keep opening the upper airway and enhance SaO2, by deep insertion into Lianquan (CV 23) plus continuous low-frequency stimulation of EA. Stimulating the branches of the hypoglossal nerve that control the genioglossus muscles can selectively elevate the activities of the genioglossus muscles to extend the tongue forward, and avoid the increase of the muscle tone in retracting the tongue, so that the effect to retract the tongue will not appear[7-8].
There is no such a term of SAS in traditional Chinese medicine. SAS belongs to the scope of somnolence in traditional Chinese medicine. Now, it is mostly listed in snoring. In stroke patients, the throat muscles are flaccid and weak and the airways are not smooth, plus failure of the lung in dominating qi and respiration, so that the patients will present thunder-like snoring and apnea during sleep. In severe cases, the respiratory disorders will occur due to the failure of the kidney in accepting qi, so that paroxysmal snoring and apnea will appear alternatively during the sleep, and the patient will wake up due to suffocation and present with laziness, somnolence, dizziness, and heavy sensation inthe four limbs in the daytime. EA on Lianquan (CV 23) is able to dredge the meridian qi of the Conception Vessel and regulate qi dynamics, so as to normalize the lung in cleaning and descending ability and the kidney in accepting ability and dredge the airways for normal outflow and inflow of yin and yang to restore the normal respiration.
Because ESS scores are in certain positive correlation with SAS severity[9], the scholars abroad believe that ESS <5 is normal, and 5-10 is mild somnolence, and 10-15 is medium somnolence and 16-24 is severe somnolence[10]. We regard ESS score as one of the judging criteria for the follow-up examination two years after the treatment. Judging from the entire situation, ESS score of two years after the treatment is slightly increased than those before the treatment, and obviously increased than those after the treatment. And the relevant clinical symptoms of blood pressure control, cardiac rhythm, with or without esophageal reflux, and nocturia cannot correctly reflect the severity of SAS.
EA treatment is remarkably effective for stroke with SAS. But, the clinical symptoms of somnolence, lassitude and poor concentration in the daytime two years after the treatment are not statistically different than those before the treatment, and are aggravated than those after the treatment.
Judging from the results in the follow-up examination two years later, this treatment protocol is not ideal in the long-term effects. There are the following five reasons. The first is age. With the increase of the age, the muscles become further flaccid and the patency of the airways decreases further, so as to induce the aggravation of OSAS clinical subjective symptoms[11]and influence the assessment of the therapeutic effects. The second is the severity of the disease of the recruited patients. Because the recruited patients were mostly in severe condition and less in medium condition, in the evolution of the diseases, the symptoms in the severe patients might develop more obviously than the patients in medium and mild condition, so that the long-term effects of EA would be certainly influenced. The third is stroke. SAS is closely related to stroke[12]. It has proved in the relevant study that the stroke patients without sleep and respiratory disturbance previously had been found out to present very high incidence rate in the multiple PSG examinations within one year of stroke[13]. In this study, the follow-up patients are all apoplectic patients, influential to OSAS symptoms. The fourth is the course of the treatment. In this study, the course is made of five sessions per week and the treatment is given for four weeks. As for the assessment of two-year long-term clinical effects, the four weeks of the treatment may be short, so as to influence the long-term clinical effects. The fifth is the contents of the follow-up examination. The indexes of AHI, the lowest SaO2value during sleep and BMI of the patients two years after the treatment cannot be obtained due to the limitation of the conditions, leading to incomplete assessment of the follow-up examination, and hence influencing the assessment results.
It has proved in this study that the short-term clinical effect is precise in treatment of OSAS by EA on Lianquan (CV 23), but the assessment of the long-term clinical effect needs to be further studied.
[1] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjingke Zazhi, 1996, 29(6): 379-380.
[2] Academic Group of Sleep Breath Disorder, Society of Respiratory Diseases of Chinese Medical Association. Diagnostic and therapeutic guidelines for obstructive sleep apnea syndrome (draft). Zhonghua Jiehe He Huxi Zazhi, 2002, 25(4): 195-198.
[3] Kothari R, Hall K, Brott T, Broderick J. Early stroke recognition: developing an out-of-hospital NIH stroke scale. Acad Emerg Med, 1997, 4(10): 986-990.
[4] Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep, 1991, 14(6): 540-545.
[5] Levin BC, Becker GD. Uvulopalatopharyngoplasty for snoring: long-term results. Laryngoscope, 1994, 104(9): 1150-1152.
[6] Lin C, Wang Y, Wang SS, Li XL, Ye YM. Follow-up study on electroacupuncture for cognitive impairment due to obstructive sleep apnea-hypopnea syndrome. Shanghai Zhenjiu Zazhi, 2012, 31(9): 649-650.
[7] Schwartz AR, Eisele DW, Hari A, Testerman R, Erickson D, Smith PL. Electrical stimulation of the lingual musculature in obstructive sleep apnea. J Appl Physiol, 1996, 81(2): 643-652.
[8] Decker MJ, Haaga J, Arnold JL, Atzberger D, Strohl KP. Functional electrical stimulation and respiration during sleep. J Appl Physiol, 1993, 75(3): 1053-1061.
[9] Li X, Ping F. Clinical significance of Epworth sleeping scale to screening diagnosis of obstructive sleep apnea syndrome. Hebei Yiyao, 2005, 27(10): 737-738.
[10] Strollo Jr PJ. Sleep Disorders in Primary Care Sleep Disorders. Totowa: Human Press, 1998: 20.
[11] Zhang P, Zhao ZX. Obstructive sleep apnea hypopnea syndrome: a review of clinical research. Chin J New Drugs Clin Rem, 2007, 26(8): 606-611.
[12] Mohsenin V. Is sleep apnea a risk factor for stroke? A critical analysis. Minerva Med, 2004, 95(4): 291-305.
[13] Cai BQ. Respiratory Internal Medicine. Beijing: China Union Medical University Press, 2002: 533-529.
Translator: Huang Guo-qi
R246.6
A
Date: June 18, 2013
Author: Wang Yin, M.M.
Ye Yong-ming, deputy chief physician.
E-mail: zjtnyx@126.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Shu-Stream Points for Two Cases with Time-related Disease
- Therapeutic Observation on Swift Needling with Fire Needle plus Medication for Herpes Zoster
- Tuina Is Superior to Electroacupuncture in Treating Thoracic Facet Joint Disorder
- Clinical Study on Electroacupuncture for Cervical Intervertebral Disc Herniation
- Therapeutic Efficacy Observation on Combining Herbal Cake-partitioned Moxibustion with Plumblossom Needle Therapy for Cervical Radiculopathy
- Clinical Observation on Acupuncture Therapy for Depression at Perimenopause
