Clinical Study on Electroacupuncture for Perimenopausal Insomnia
2013-07-18ChenXiulingXuKaiQinXiaohong
Chen Xiu-ling, Xu Kai, Qin Xiao-hong
1 Fangcun Hospital of Traditional Chinese Medicine, the Third Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine, Guangzhou 510360, China
2 Guangdong Second Provincial Traditional Chinese Medicine Hospital, Guangzhou 510095, China
Clinical Study on Electroacupuncture for Perimenopausal Insomnia
Chen Xiu-ling1, Xu Kai2, Qin Xiao-hong2
1 Fangcun Hospital of Traditional Chinese Medicine, the Third Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine, Guangzhou 510360, China
2 Guangdong Second Provincial Traditional Chinese Medicine Hospital, Guangzhou 510095, China
Objective: To observe the clinical efficacy of electroacupuncture in treating perimenopausal insomnia.
Methods: Seventy eligible subjects were randomized into two groups, 38 subjects in the treatment group were intervened by electroacupuncture, 30 min each session; 32 subjects in the control group were intervened by Alprazolam, 0.4 mg each time before sleep. Athens insomnia scale (AIS) was adopted to evaluate sleep quality.
Results: The therapeutic efficacy in the treatment group was significantly better than that in the control group (P<0.05).
Conclusion: Electroacupuncture can produce a content therapeutic efficacy in treating perimenopausal insomnia.
Acupuncture Therapy; Electroacupuncture; Climacteric Syndrome; Perimenopausal Syndrome; Complications; Sleep Initiation and Maintenance Disorders
Due to physiologic decline of ovarian function, decreased production of estrogen and subsequent poor adaptability to external environment and hypersensitivity to various psychological factors and somatic diseases, as well as poor tolerance, premenopausal woman will present with a series of symptoms such as hot flash, perspiration, anxiety, and insomnia, which are generally termed as perimenopausal syndrome. Sleep disorder is a very common symptom of perimenopausal syndrome, and it can influence the patient’s work and life in severe cases. Under the guidance of traditional Chinese medicine (TCM) and combining years of clinical experience, the author has conducted a randomized controlled trial among 70 patients with perimenopausal insomnia by using electroacupuncture and oral Western medication. The report is now present as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria of Western medicine
It’s based on the diagnostic criteria of primary insomnia in theDiagnostic and Statistical Manual of Mental Disorders(DSM-Ⅳ)[1]by the American Psychiatric Association and the diagnostic criteria of female menopause in theGuiding Principles for Clinical Study of New Chinese Medicines[2].
1.1.2 Diagnostic criteria of TCM
It’s based on the TCM diagnostic criteria of perimenopausal syndromes in theGuiding Principles for Clinical Study of New Chinese Medicines[2]and the diagnostic criteria of sleeplessness in theCriteria of Diagnosis and TherapeuticEffects of Diseases and Syndromes in Traditional Chinese Medicine[3].
1.2 Inclusion criteria
In accordance with the above diagnostic criteria of Chinese and Western medicines; without using any sleeping pills in the last 1 week; aged 45-55 years old.
1.3 Exclusion criteria
Against the above diagnostic and inclusion criteria; patients with a history of gynecological operation, or insomnia caused by organic diseases, neural or mental system diseases; in co-morbid with primary diseases of cardiocerebrovascular, liver, kidney, or hematopoietic systems which may threaten the life; under other treatment or being taking other medicines, which may influence the evaluation of therapeutic effects.
1.4 General data
Seventy eligible female patients were divided into two groups by simple randomized-controlled method. Of the 38 subjects in the treatment group, 27 were 45-50 years old, 11 were 50-55 years old, and their disease durations were 1-12 months. Of the 32 subjects in the control group, 20 were 45-50 years old, 12 were 50-55 years old, and their disease durations were 0.5-12 months. There were no statistically significant differences between the two groups in age and disease duration (P>0.05), indicating that the two groups were comparable.
Table 1. Comparison of general data ()
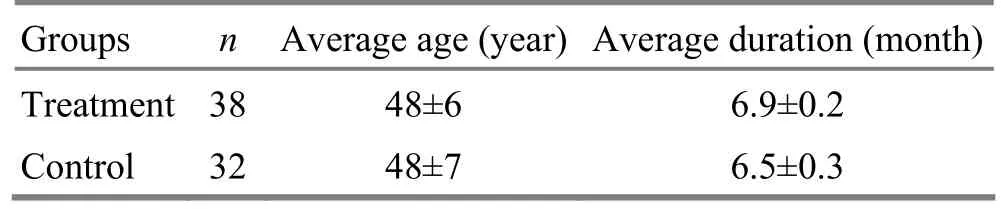
Table 1. Comparison of general data ()
GroupsnAverage age (year) Average duration (month) Treatment 38 48±6 6.9±0.2 Control 32 48±7 6.5±0.3
2 Treatment Methods
2.1 Treatment group
Major acupoints: Bilateral Yingu (KI 10) and Fuliu (KI 7).
Adjunct acupoints: Anmian [Extra, located at the midpoint between Yiming (EX-HN 14) and Fengchi (GB 20)], Shenmen (HT 7), Neiguan (PC 6), Baihui (GV 20), Yinlingquan (SP 9), Sanyinjiao (SP 6), Xuehai (SP 10).
Supplementary points based upon syndrome differentiation: Xinshu (BL 15) and Pishu (BL 20) were added for deficiency of heart-spleen; Danshu (BL 19) and Xinshu (BL 15) were added for qi deficiency of the heart and gall bladder; Xingjian (LR 2) and Taichong (LR 3) were added for depressed liver qi transforming into fire; Fenglong (ST 40) and Neiting (ST 44) were added for internal disturbance of phlegm-heat; Taixi (KI 3) and Daling (PC 7) were added for fire excess due to yin deficiency; Geshu (BL 17) and Danzhong (CV 17) were added for qi-blood stagnation.
Operation: All major acupoints and 8 of the adjunctive acupoints were selected every time, and the adjunctive acupoints were selected alternately. Yingu (KI 10) was initially needled. Patient was asked to take a supine position, with hip abducted. After routine sterilization, a filiform needle of 0.30 mm in diameter and 40 mm in length was obliquely inserted into the point for 0.8-1 cun along the direction of the meridian. Fuliu (KI 7) was then punctured perpendicularly for 0.5-0.8 cun. The two points were given reinforcing needling manipulations. After needling sensation was obtained, G6805-2 electroacupuncture apparatus was connected to the needle handles, with dense wave, frequency at 0.7 Hz, intensity within patient’s endurance, and the electroacupuncture stimulation lasted 30 min. The rest acupoints were given conventional acupuncture, with even reinforcingreducing manipulation, and the needles were retained for 30 min after needling qi was obtained. The treatment was given once every day, interval at weekends, 10 sessions as a treatment course. Therapeutic effects were evaluated after 2 treatment courses, and there was a 7-day interval between the two courses.
2.2 Control group
The control group was intervened by taking Alprazolam 0.4 mg, once every night, 30 min before sleep. Therapeutic effects were evaluated after continuous 5-week treatment.
3 Therapeutic Efficacies
3.1 Criteria of therapeutic efficacy[4]
Recovery: Sleep duration is restored to normal level or night sleep duration is >6 h, and sleep is tight and refreshing.
Marked effect: Sleep is obviously improved, sleep duration is increased by ≥3 h, and sleep is deeper.
Effective: Symptoms are improved, while sleep duration is increased by <3 h.
Invalid: Insomnia is not improved or even deteriorated after treatment.
3.2 Evaluation scale
The internationally recognized Athens insomnia scale (AIS)[5]was adopted to evaluate insomnia patients’sleep quality before and after treatment.
3.3 Statistical method
The SPSS 11.0 software was used for statistical analyses. The ranked data were processed by Rank-sum test, enumeration data were by Chi-square test, and measurement data were byt-test.
3.4 Treatment result
After 2 treatment courses, the total effective rate was 89.5% in the treatment group versus 75.0% in thecontrol group, and the treatment group was significantly superior to the control group in therapeutic effect (P<0.05).
The difference in AIS score was statistically insignificant between the two groups before treatment (P>0.05), indicating that they were comparable. The intra-group comparison of AIS showed statistically significant differences in both groups after treatment (P<0.05), indicating that the insomnia symptoms were improved in both groups; after treatment, there was statistically significant difference in AIS between the two groups (P<0.05), indicating that the therapeutic effect of the treatment group is better than that of the control group (table 2 and table 3).
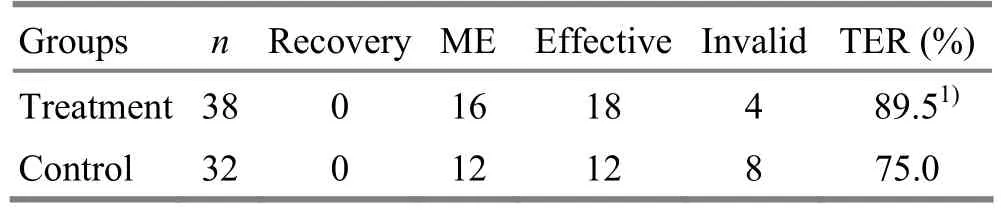
Table 2. Comparison of therapeutic efficacy (case)
Table 3. Comparison of AIS scores before and after treatment (, point)
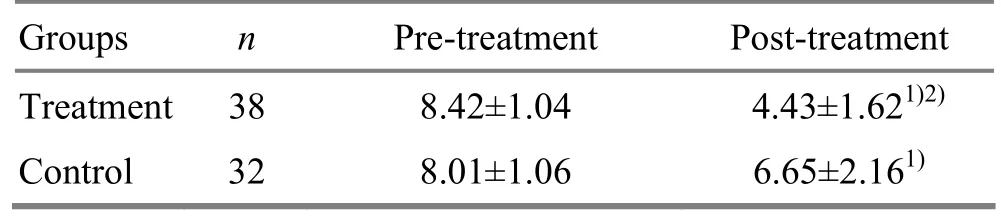
Table 3. Comparison of AIS scores before and after treatment (, point)
Note: Intra-group comparison with pre-treatment result, 1)P<0.05; compared with the control group after treatment, 2)P<0.05
GroupsnPre-treatment Post-treatment Treatment 38 8.42±1.04 4.43±1.621)2)Control 32 8.01±1.06 6.65±2.161)
3.5 Adverse reaction
Subjects in the treatment group didn’t show any adverse reactions. Subjects in the control group present various discomforts such as fatigue, lassitude, and dizziness in the morning after taking medicine, which can be relieved by rest, and 8 patients showed drug dependence of Western medication.
4 Discussion
Perimenopausal insomnia falls under the scope of perimenopausal syndromes in TCM. It is located in the heart, closely related to the liver and kidney. Therefore, the treatment should be focused on regulating the liver and kidney. This study selected acupoints from the Kidney Meridian for acupuncture. Yingu (KI 10) is the He-Sea acupoint of the Kidney Meridian, belonging to water according to five-element theory; Fuliu (KI 7) belonging to metal according to five-element theory, and is the mother-point of Yingu (KI 10). According to the principle that the mother-point should be tonified in deficiency and the child-point should be reduced in excess, these two points were selected as the major acupoints to supplement kidney yin and produce kidney water. When water is sufficient, fire can be restricted, and there approaches balance between yin and yang, water and fire. And therefore, the heart can be nourished by kidney water to relieve deficient heat, and a normal sleep state is then restored. Taixi (KI 3) and Taichong (LR 3) can tonify yin and reduce fire, clear heart fire and calm mind; Anmian (Extra) works to tranquilize and calm mind, and is a experiential effective point for insomnia; Shenmen (HT 7), the Yuan-Primary acupoint of the Heart Meridian, and Neiguan (PC 6), the Luo-Connecting acupoint of the Pericardium Meridian, can both tranquilize mind; Sanyinjiao (SP 6) and Yinlingquan (SP 9) can supplement yin and so as to restrict yang; Baihui (GV 20) works to clear and tranquilize mind; Xuehai (SP 10) and Sanyinjiao (SP 6) work to tonify blood and soothe liver. The heart, liver, and kidney are simultaneously treated to supplement yin of the three organs, and hence a satisfactory effect can be achieved.
Modern medicine holds that insomnia basically results from the imbalance between the inhibition and excitation of brain. In electroacupuncture, dense wave is used to treat insomnia because it can lower the neural reaction and modulate the central nervous system. AID is an important measurement index in evaluating sleep quality, and provides reliable evidence for the evaluation of therapeutic effect. The current study shows that electroacupuncture can regulate the body in a systematic way, and can produce a content therapeutic effect in relieving perimenopausal insomnia without adverse reactions, and it’s worth promoting in clinic.
[1] American Psychiatric Association. The Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington DC: American Psychiatric Press, 1994: 25.
[2] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: People’s Medical Publishing House, 1997: 98.
[3] State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Nanjing: Nanjing University Press, 1994: 19-20.
[4] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: People’s Medical Publishing House, 1993: 186.
[5] Weng M, Liao HQ. Therapeutic analysis of electroacupuncture for insomnia in elderly. Zhenjiu Linchuang Zazhi, 2007, 23(5): 33-34.
Translator: Hong Jue
R246.6
A
Date: July 25, 2013
Author: Chen Xiu-ling, associate chief physician.
E-mail: zjtnyx@126.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Clinical Study on Electroacupuncture for Cervical Intervertebral Disc Herniation
- Observation on Clinical Effects of Electroacupuncture Therapy for Apoplexy with Obstructive Sleep Apnea Syndrome
- Clinical Observation on Acupuncture Therapy for Depression at Perimenopause
- Therapeutic Efficacy Observation on Combining Herbal Cake-partitioned Moxibustion with Plumblossom Needle Therapy for Cervical Radiculopathy
- Therapeutic Observation on Swift Needling with Fire Needle plus Medication for Herpes Zoster
- Shu-Stream Points for Two Cases with Time-related Disease
