Efficacy Observation on Auricular Point Sticking Combined with Cupping in Treating Insomnia
2013-07-18LiJianpingZhangHuiHePeida
Li Jian-ping, Zhang Hui, He Pei-da
Xuhui District Central Hospital, Shanghai 200031, China
Efficacy Observation on Auricular Point Sticking Combined with Cupping in Treating Insomnia
Li Jian-ping, Zhang Hui, He Pei-da
Xuhui District Central Hospital, Shanghai 200031, China
Objective: To observe the clinical efficacy of auricular point sticking combined with cupping in treating insomnia.
Methods: Sixty-four patients with chronic insomnia were randomly divided into two groups. Thirty-two patients in the treatment group were treated with auricular point sticking combined with cupping therapy; while thirty-two patients in the control group were treated by Diazepam. The Pittsburgh sleep quality index (PSQI) were observed before and after treatment, and the data were statistically analyzed to evaluate the clinical effect.
Results: After treatment, PSQI scores in both groups after treatment significantly decreased (P<0.05), and there was a significant difference between the two groups (P<0.05). In the improvement of daytime function, the treatment group was more efficient than the control group (P<0.05). The total effective rate of the treatment group was higher than that of the control group (P<0.05).
Conclusion: Auricular point sticking combined with cupping therapy for insomnia is more effective than oral Diazepam, and it has a better effect in improving the patient's daytime function.
Auricular Point Sticking; Cupping Therapy; Insomnia
Insomnia means an inability to fall asleep or to stay asleep in a suitable environment; the majority of patients suffer from chronic insomnia longer than six months[1]. A survey has found that about 10%-15% of adults suffer from chronic insomnia[2]. Chronic insomnia can not only reduce the quality of life and affect work efficiency, but also increase the risks of accidents and mental illness. Western medicine for insomnia is mainly based on sedative hypnotic drugs, which may have severe side effects, drug dependence and tolerance. Auricular point sticking combined with cupping along the Bladder Meridian on the back is a special way for chronic insomnia, and the study is summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
The relevant literatures are referenced to develop the diagnostic criteria for insomnia[3]. There are typical symptoms of insomnia such as difficulty falling asleep, frequent awakening, difficulty staying asleep or inability to sleep after waking up, waking up too early and inability to sleep at night, and drowsiness or sleepiness in daytime; sleep duration is less than 6 h a day; the disease duration is longer than 6 months.
1.2 Inclusion criteria
Their disease durations are more than 6 months, and they meet the following conditions. Their chief complaint is sleep dysfunction (caused by sleep disruption or reduced sleep duration); they are suffering from symptoms caused by sleep dysfunction such as daytime fatigue, distention in the head, dizziness and so on; their ages are between 18 and 70 years old.
1.3 Exclusion criteria
Those who do not meet the inclusion criteria; insomnia caused by the systemic diseases such as pain (neuralgia and joint pain etc.), fever, cough, as well as surgery or external environmental disturbances; aged between 18 and 70 years old; pregnant or lactating women; those complicated with severe primary diseases of cardiovascular, lung, liver, kidney and hematopoietic system; psychopath; short sleepers who just have reduced amount of sleep without daytime discomfort; patients who fail to be treated according to the guideline or have incomplete information as a result in affecting the judges of efficacy.
1.4 Withdrawal criteria
Those who cannot adhere to complete the treatment; failure to be treated according to protocol; having serious adverse events or adverse reactions; having severe complications or disease condition worsening during treatment.
According to the above withdrawal criteria, if some patients drop out, the reasons and their relation to clinical research will be carefully recorded.
1.5 General data
Sixty-four cases were enrolled including 24 males and 40 females, and all of them were our patients from October 2009 to October 2010. Enrolled patients were randomly divided into a treatment group and a control group by visiting sequence according to random number table. During the observation, both groups had two cases drop out due to loss of contact, and there were 60 patients completing the treatment in the two groups, including 23 males and 37 females. The differences in gender, disease duration and Pittsburgh sleep quality index (PSQI) score before treatment between the two groups had no statistical significance (allP>0.05), (table 1). It indicated that the two groups were comparable. The clinical procedure was shown in Fig.1.
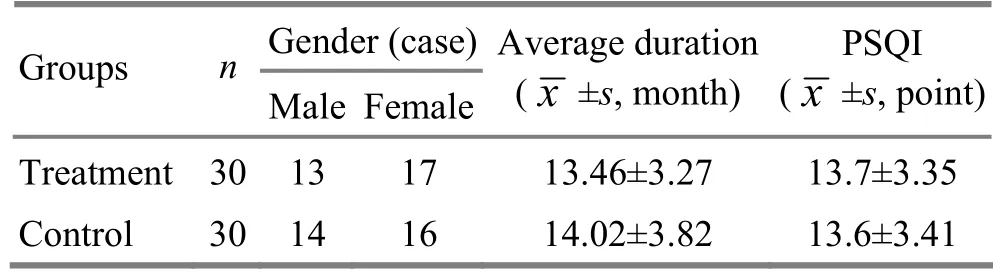
Table1. Comparison of general data between the two groups

Fig.1 Clinical management flow chart
2 Treatment Methods
2.1 Treatment group
2.1.1 Auricular point sticking
Acupoints: Shenmen (TF4), Subcortex (AT4), Heart (CO15), Liver (CO12), Kidey (CO10), Occiput (AT3) and Anterior Ear Lobe (LO4), (Fig.2).
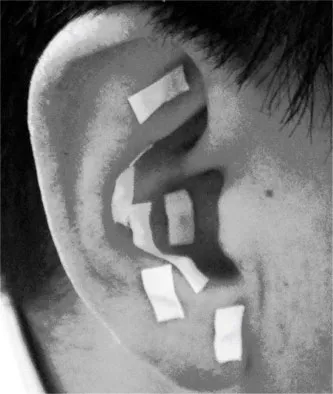
Fig.2 Auricular point
Operation: StickWang Bu Liu XingZi(Semen Vaccariae) to the above mentioned auricular points, one ear for each time and change alternatively. Ask patients to press those stickers 3-5 times every day with an intensity of stimulation that the patient can tolerate. In addition, strengthen pressing before bedtime, and press 10 times for each point.
2.1.2 Cupping
Ask the patients to take a prone position. Choose cupping jars of different sizes according to the patient’s weight, physical constitution and lesion location, and make cupping jars suck on the Bladder Meridian lines on both sides of spine by flash cupping, and retain cups for 5-10 min each time (Fig.3).
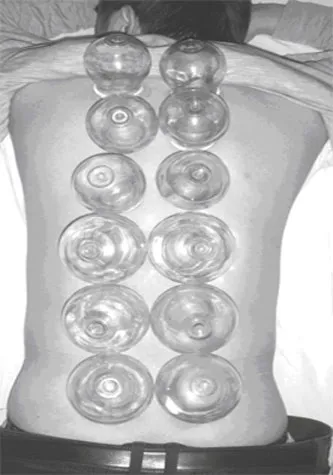
Fig.3 Cupping on the back
After auricular point sticking, apply cupping therapy once every other day, and 10 times in total.
2.2 Control group
Patients in the control group were treated with oral Diazepam tablets, 5 mg each time, and once per night for 20 d.
3 Therapeutic Results
3.1 Observation indexes
PSQI scores were assessed before and after treatment[4], including sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance and daytime dysfunction. Each item was scored by 0-3 points. The sum of their scores composes of global PSQI score (0 to 21 points), and the higher the score, the poorer the quality of sleep.
3.2 Therapeutic criteria
TheGuiding Principles for Clinical Study of New Chinese Medicinesis referenced[5].
Cure: Sleep duration returns to be normal or night sleep duration is more than 6 h, and the patient has deep sleep and is energetic after waking up.
Marked effect: The patient’s sleep quality improves significantly, and his or her sleep duration increases by more than 3 h, and so does the quality of sleep.
Improvement: The symptoms relieve, and sleep duration increases by less than 3 h.
Failure: There is no relief of insomnia symptoms or the symptoms get even worse after treatment.
3.3 Statistical methods
The SPSS 13.0 statistical software was used for all data analysis, and measurement data were expressed by mean ± standard deviation (). The intra-group comparison was analyzed by pairedt-test, while inter-group comparison was analyzed by analysis of variance. The enumeration data were compared using Chi-square test.P<0.05 indicates statistically significant difference.
3.4 Treatment results
3.4.1 Comparison of therapeutic efficacy
The total effective rate was 90.0 % in the treatment group versus 83.3 % in the control2group, and the difference was statically significant (χ=4.23,P<0.05), showing that the treatment group was more effective than the control group (table 2).
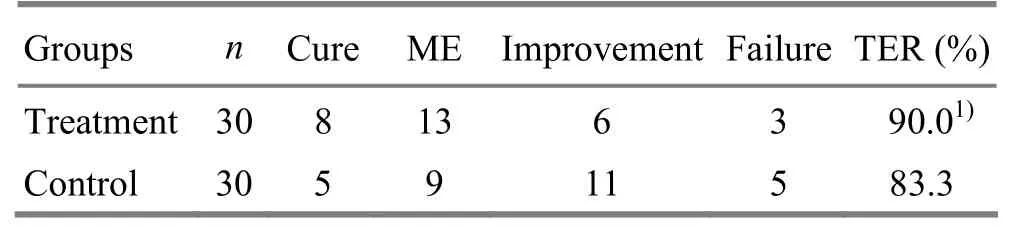
Table 2.Comparison of therapeutic efficacy between the two groups (case)
3.4.2 Comparison of PSQI scores between the two groups before and after treatment
After treatment, the different item scores and global score of PSQI in the treatment group were significantly different from those before treatment, and the different items included sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance and daytime dysfunction (P<0.05), indicating that auricular point sticking combined with cupping along the Bladder Meridian on the back can effectively relieve the symptoms of chronic insomnia.
After treatment, different item scores and global score of PSQI in the control group were also significantly different from those before treatment (P<0.05), showing that Diazepam can also relieve the symptoms of chronic insomnia. After treatment, the treatment group was more efficient than the control group in improving daytime dysfunction (P<0.05), indicating auricular point sticking combined with cupping along the Bladder Meridian on the back can relieve various symptoms of chronic insomnia as well as Diazepam, and should have better efficacy in the improvement of daytime function than Diazepam (table 3).
Table 3. Comparison of PSQI scores between the two groups before and after treatment (, point)
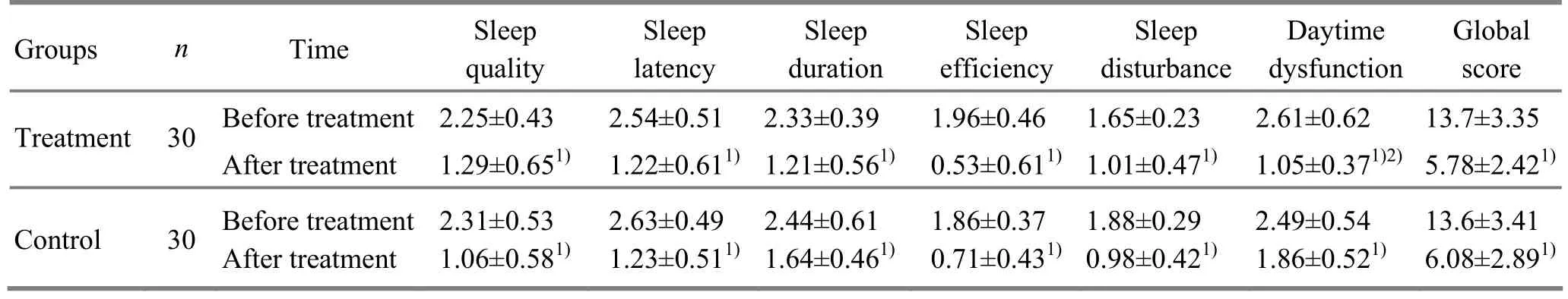
Table 3. Comparison of PSQI scores between the two groups before and after treatment (, point)
Note: Compared to the result of same group before treatment, 1)P<0.05; compared to the control group after treatment, 2)P<0.05
GroupsnTime Sleep quality Sleep latency Sleep duration Sleep efficiency Sleep disturbance Daytime dysfunction Global score Treatment 30 After treatment1.29±0.651)1.22±0.611)1.21±0.561)0.53±0.611)1.01±0.471)1.05±0.371)2)5.78±2.421)Before treatment2.25±0.43 2.54±0.51 2.33±0.39 1.96±0.46 1.65±0.23 2.61±0.62 13.7±3.35 Control 30 Before treatment After treatment 2.31±0.53 1.06±0.581)2.63±0.49 1.23±0.511)2.44±0.61 1.64±0.461)1.86±0.37 0.71±0.431)1.88±0.29 0.98±0.421)2.49±0.54 1.86±0.521)13.6±3.41 6.08±2.891)
4 Discussion
The pathogenesis of insomnia is closely related to sleep-wake cycle. A more generally accepted mechanism is that raphe nuclei and nucleus of solitary tract in brainstem induce sleep occurrence, while Locus Coeruleus of pars dorsalis pontis has an effect in staying awake. Suprachiasmatic nucleus is the body’s basic biological clock, which includes an oscillator keeping circadian itself and can make endogenous circadian system and the external light-dark cycle phase coupling. Thalamus is also one of the important parts involved in sleep-wake rhythm, including both the induction of sleep and awakening mechanisms. Besides, as the body’s senior center, cerebral cortex can produce awareness activities to affect the sleep-wake rhythm. The diminished or enhanced inhibition effect of above mentioned nerve physiological function can lead to the occurrence of insomnia, as well as the pathological changes of participating neuroanatomical structure[6].
Insomnia belongs to the category of sleeplessness in traditional Chinese medicine, which mainly results from yin and yang imbalance, Ying-Nutrient and Wei-Defensive disharmony, qi and blood deficiency and dysfunctions of Zang-fu organs. Auricular acupuncture is one type of the micro-needle therapy. Meridian’s paths are closely related to ears. Among the twelve meridians, Six Yang Meridians go into ears, run on the front of them and finally reach the tips of ears respectively; although six yin meridians have no direct relation with the ears, they coincide with yang meridians by the branch of them to reach ears. Inthis study, acupoints including Shenmen (TF4), Subcortex (AT4), Heart (CO15), Liver (CO12), Kidey (CO10), Occiput (AT3) and Anterior Ear Lobe (LO4) were selected to regulate yin and yang, Zang-fu, Ying-Nutrient and Wei-Defensive as well as qi and blood, to relieve the symptoms of insomnia by the meridians’ function[7-9].
Modern medicine believes that there is a physiological internal relation between the auricle and the human body. Clinical observation shows that when there is a lesion in a body part or an organ, there is tenderness in a specific ‘reaction point’ in the ear[10]. Auricle is not only innervated by great auricular nerve and lesser occipital nerve from cervical spinal cord, but also the branches from the 5th,7th,9th,10th pairs of cranial nerves, while the 7th, 9th and 10th nerves contain the most complex nerve fibers. Good stimulation to the ear spreads impulses to the related nucleus, so that the ecological inhibition occurs to block the original pathological afferent impulses and intense excitement generation. Therefore, according to advantage principle, the original pathological excitement lesion is inhibited and replaced by normal physiological regulation, so that the patient’s symptoms can be reduced or cured[11-15]. On the base of auricular anatomy and physiological function combined with the pathogenesis of insomnia in modern medicine, the mechanism of auricular acupuncture in treating insomnia is revealed.
Zang-fu organs connect with the meridian qi of Back-Shu acupoints on the Foot Meridian of Taiyang on the back, thus Zang-fu diseases can be cured through Back-Shu acupoints as well as the five sense organs and the nine orifices diseases associated with Zang-fu organs. Cupping on the back can regulate Foot Taiyang Meridian, and harmonize Ying-Nutrient, Wei-Defensive, qi and blood of organs and systems. Finally, the insomnia symptoms can be relieved.
Meanwhile, back area is closely linked to the spinal nerves and sympathicus, and paraspinal sympathetic ganglia located in its deep areas. Cupping effect can excite different nerve fibers, resulting in a variety of bio-electrical activities. On one hand, impulses can be transmitted to different levels of the centrum and spread out along the descending fibers after integration in order to regulate the functions of related organs; on the other hand, it can play a regulatory role by local reflex arc[16-17]. And this can explain the mechanism of the cupping on back in treating insomnia from the perspective of modern medicine.
In a word, the total effective rate of auricular point sticking combined with cupping along the Bladder Meridian on the back in treating insomnia is higher than oral Diazepam; and the therapy is almost equally effective with Diazepam in relieving different symptoms of chronic insomnia, and better in the improvement of daytime function than Diazepam.
[1] Tian HJ, Huang LQ, Zhao ZX. Assessment and treatment of insomnia. Acad J Sec Mil Med Univ, 2006, 27(5): 538-540.
[2] Roth T. New developments for treating sleep disorders. J Clin Psychiatry, 2001, 62(Suppl 10): 3-4.
[3] Experts group of expert consensus for the definition, diagnosis and treatment of insomnia. Expert consensus for the definition, diagnosis and treatment of insomnia (draft). Zhonghua Shenjingke Zazhi, 2006, 39(2): 141-143.
[4] Liu XC, Tang MQ, Hu L, Wang AZ, Xi HX, Zhao GF, Gao CN, Li WS. Reliability and validity of the Pittsburgh sleep quality index. Zhonghua Shenjingke Zazhi, 1996, 29(2): 103-107.
[5] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medico-Pharmaceutical Science & Technology Publishing House, 1993: 186-187.
[6] Xu ZP, Chen WJ, Li HH, Li YH. Study and treatment of insomnia. Zhongguo Linchuang Kangfu, 2006, 10(22): 151-153.
[7] Huang QF. Exploration of the clinical regularity of acupuncture and moxibustion treatment for insomnia. J Acupunct Tuina Sci, 2010, 8(1): 12-16.
[8] Pei Y, Wang WM. Observations on the efficacy of acupuncture plus auricular point magnetic bead plaster therapy in treating insomnia. Shanghai Zhenjiu Zazhi, 2009, 28(11): 629-631.
[9] Yuan X. Clinical observation on acupuncture plus auricular point sticking in treating insomnia. J Acupunct Tuina Sci, 2010, 8 (5): 302-303.
[10] Wei CJ. Concise Science of Auricular Acupuncture. Hefei: Anhui Science and Technology Publishing House, 1987: 5.
[11] Shi YQ. Textbook of Clinical Neurology. 2nd Edition. Shanghai: Shanghai Science and Technology Publishing House, 1994: 1124.
[12] Wang GL. Clinical observations on auricular point plaster therapy for insomnia. Shanghai Zhenjiu Zazhi, 2012, 31(10): 725-726.
[13] Shao M, Wen LJ, Huang WY. The observations on the curative effect of acupuncture plus auricular-plaster therapy on insomnia. Shanghai Zhenjiu Zazhi, 2002, 21(5): 14-15.
[14] Zhang XM, Shen PF, Chen DY. Clinical study progress on auricular points for insomnia. Jiangxi Zhongyiyao, 2012, 43(9): 59-61.
[15] Wang XY, Huo YF. Review of insomnia treated by auricular-plaster therapy. Shanghai Zhenjiu Zazhi, 2007, 26(4): 47-48.
[16] Hong SH, Liu YY, Guo Y. Study progress on action mechanism of cupping therapy. Henan Zhongyi, 2012, 32(2): 261-263.
[17] Yan JT. Science of Tuina. Beijing: China Press of Traditional Chinese Medicine, 2003: 180.
Translator: Deng Ying
R246.6
A
Date: August 12, 2013
Author: Li Jian-ping, M.D., associate chief physician.
E-mail: zjtnyx@126.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Clinical Study on Electroacupuncture for Cervical Intervertebral Disc Herniation
- Observation on Clinical Effects of Electroacupuncture Therapy for Apoplexy with Obstructive Sleep Apnea Syndrome
- Clinical Observation on Acupuncture Therapy for Depression at Perimenopause
- Therapeutic Efficacy Observation on Combining Herbal Cake-partitioned Moxibustion with Plumblossom Needle Therapy for Cervical Radiculopathy
- Therapeutic Observation on Swift Needling with Fire Needle plus Medication for Herpes Zoster
- Shu-Stream Points for Two Cases with Time-related Disease
