Serum parameters predict the severity of ultrasonographic findings in non-alcoholic fatty liver disease
2012-06-11
Kashan,Iran
Introduction
Non-alcoholic fatty liver disease (NAFLD) is a common cause of chronic liver damage.[1]It can lead to end-stage liver disease and hepatocellular carcinoma.[2]The prevalence of nonalcoholic steatohepatitis (NASH) in a sample of the general population of Iran is reported to be 2%.[3]The prevalence of viral hepatitis is decreasing,meanwhile the NAFLD prevalence seems to be increasing due to the epidemic of obesity.[4-6]
Although liver biopsy is the gold standard method for diagnosis and prognosis of NAFLD,the possible risks and invasiveness have limited its use in common practice.Liver biopsy is not obligatory for the diagnosis of NAFLD; and is not always necessary to differentiate simple fatty liver from the more severe form (NASH).[7]
Imaging techniques are safe,reliable,and acceptable methods for the diagnosis of NAFLD.[8]They are becoming popular for estimating the severity of NAFLD and the diagnosis of patients in the early (preclinical)stage of disease,even before the liver function tests show any abnormality.Because of the cost-effectiveness and availability,ultrasonography is widely used to detect NAFLD.Although somewhat subjective,a radiologist can identify the severity of fatty liver by visual assessment of hepatic echogenicity.[9]We used liver ultrasonography for the diagnosis of NAFLD and the evaluation of disease severity in this study.
Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are among the most common markers of hepatocyte damage and are elevated in NASH.NASH seems to be a more advanced stage of the disease than simple fatty liver that includes patients with normal laboratory data and only evidence of fatty liver at ultrasonography.Their healthy ranges are proposed to be lower than the cut-off points advised by the manufacturer's kit.[10]Because of a healthy range of ALT that is lower than the reference range currently used by laboratories (40 U/L),more patients with mild fatty liver disease can be diagnosed; therefore laboratory data alone are limited in diagnosing NAFLD.Alkaline phosphatase(ALP) is a liver enzyme and its elevation raises the suspicion of infiltrative liver disease.It may be elevated in advanced NAFLD.[11]Since NAFLD is considered the hepatic manifestation of metabolic syndrome,[12]insulin resistance biomarkers like serum triglyceride (TG),cholesterol (CHOL),low density lipoprotein (LDL) and high density lipoprotein (HDL) might be correlated with the extent of liver involvement.[13,14]
Controversy exists over the correlation between liver ultrasonography and serum parameters for evaluating the severity of liver involvement in NAFLD.Therefore,this study was designed to:1) determine the association between the severity of fatty liver at ultrasonography and serum parameters correlated with the severity of NAFLD according to previous studies; and 2) set optimal cutoff points for those serum parameters correlated with the severity of fatty liver at ultrasonography,in order to differentiate the ultrasonographic groups (USGs).
Methods
This study was carried out in accord with the ethical standards for human experimentation (Helsinki Declaration) and was approved by the Ethics Committee of Kashan University of Medical Sciences (5764).The purpose of the study was explained to the participants and written informed consent was given.
Study design
Considering the mean prevalence of NAFLD in previous studies and using the formula of estimation of sample size,N=(t/d)2*(1-p)/p (t=1.96,p=0.28 and d=0.2),we defined a sample size of 245 in our study.[15-17]All patients with evidence of fatty liver in ultrasonography who were referred to the gastroenterology clinic in a general hospital from January to June 2010 were enrolled in the study (Step 1).Patients who agreed to participate in the study were interviewed.Those with a history of any hepatotoxic medication during the past 6 months,any amount of alcohol consumption or any other known liver diseases (including viral,autoimmune and metabolic causes),severe systemic co-morbidities,or neoplasm were excluded (Step 2).Then the remaining participants were checked for serum hepatitis B surface antigen,hepatitis B core antigen,hepatitis C antibody (enzyme-linked immunosorbent assay method),ceruloplasmin,and gamma-globulin levels.Those with either positive viral markers,decreased ceruloplasmin level (<20 mg/dL) or increased gamma-globulin level (>1.5 g/dL) were excluded from the study (Step 3).
Study measurements
The height (m) and weight (kg) of participants were measured and body mass index (BMI) was calculated.
Ultrasonography of the liver
All participants underwent liver ultrasonography for the grading of fatty change using a 3.5-MHz probe (Logiq 200 PRO,Tokyo,Japan).A single expert radiologist (to avoid inter-operator discordance)performed all ultrasonographic evaluations.The ultrasonography was repeated in one hundred participants by the same radiologist for evaluation of intra-observer reliability.The ultrasonography was performed on two separate days spaced less than one week apart for the staging of fatty liver in this group of participants.The radiologist was blinded to the results of laboratory and other clinical data.
A fatty liver scatters the ultrasound beam more than a non-fatty liver,so the fatty liver appears hyperechogenic.[18]Because there is no absolute echogenicity that denotes liver fat,comparison of echogenicity with internal structures known to be void of fat,such as the kidneys or the spleen,is required.[19]Therefore in this study,the radiologist obtained a sagittal view of the right liver lobe and right kidney for the evaluation of fatty liver.
The ultrasonographic findings were graded from one to three according to the echogenicity of the liver.In grade one (mild),echogenicity was slightly increased,with normal visualization of the diaphragm and intra-hepatic vessel borders.In grade two (moderate),echogenicity was moderately increased,with slightly impaired visualization of the diaphragm or intrahepatic vessels.In grade three (severe),echogenicity was markedly increased,with poor or no visualization of the diaphragm,intra-hepatic vessels,and the posterior portion of the right lobe.[8]
Laboratory investigations
On the day of liver ultrasonography,and after an overnight fast,the sera of participants were tested for fasting blood sugar (FBS),ALT,AST,ALP,TG,CHOL,LDL and HDL levels using an Erba Mannheim auto analyzer XL-640 (Erba Diagnostics Mannheim,Germany)with a Pars Azmoon reagent kit (Tehran,Iran).ALT,AST,and ALP levels were reported as U/L and TG,CHOL,LDL and HDL levels were reported as mg/dL.
Diabetes mellitus (DM) was diagnosed according to either previous diagnosis by a physician,or the use of drugs to control it,or if FBS was ≥126 mg/dL,checked twice.TG and ALT levels >150 mg/dL and >40 U/L and an HDL level <45 mg/dL for men and <50 mg/dL for women were considered abnormal.[10,20,21]
Statistical analysis
We assessed the intra-observer reliability of ultrasonographic staging.The reliability of ultrasonographic findings was evaluated by their reproducibility[intraclass correlation coefficient (ICC)],and internal consistency (Cronbach's α).We also calculated κ to define the agreement level of two ultrasonographic findings in the same participant.The frequency of gender and DM in different USGs were compared by the Chi-square test.Analysis of variance (ANOVA) was performed for the comparisons of mean age,BMI and laboratory concentrations between USGs using Tukey's post-hoc test (considering the ultrasonographic mild group as the reference category).Based on the results of the subgroup analysis (post-hoc tests),the USGs were revised and changed to "mild" and "moderate to severe"groups.The "mild" group consisted of participants with mild fatty infiltration (grade 1) at ultrasonography and the "moderate to severe" group consisted of participants with either moderate or severe fatty infiltration (grade 2 or 3) at ultrasonography.Multivariate logistic regression analysis was carried out to evaluate the variables independently associated with the revised USGs.All variables were included in a multivariate forward stepwise procedure.Odds ratios (ORs) with their 95%confidence intervals (CIs) were calculated for each independent variable.
Then optimal cut-off values of ALT,TG and HDL were calculated for differentiating between the "mild"and "moderate to severe" USGs,using receiver operating characteristic (ROC) curve analysis.The optimal cutoff value was calculated through the contact point of the ROC curve and the line with slope equal to one in which the sum of sensitivity and specificity was the highest.
Statistical analyses were performed using SPSS version 17 (SPSS,Chicago,IL,USA).The probability of a difference between the dependent and independent variables was considered significant if the P value was <0.05.
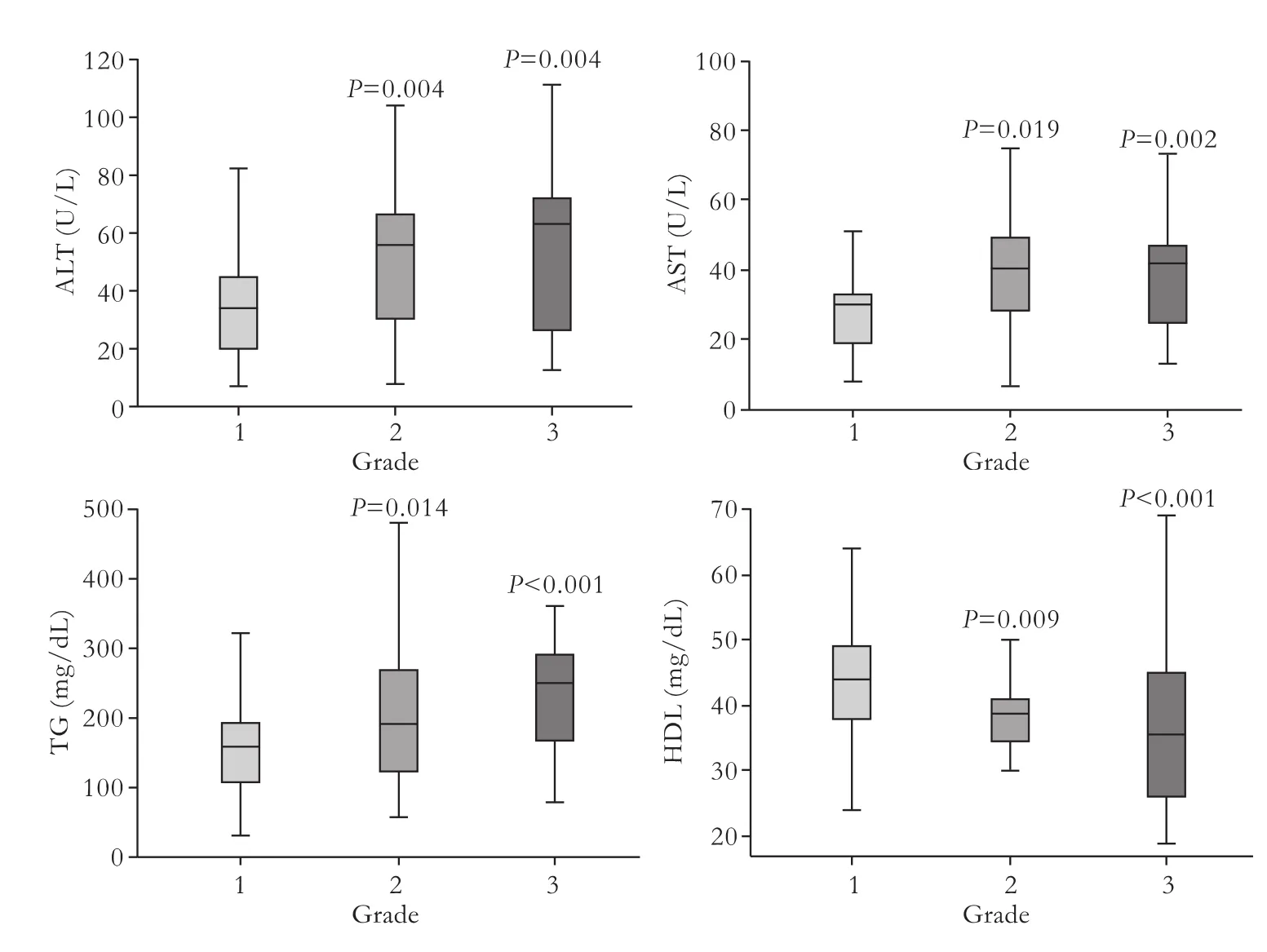
Fig.1.Serum alanine aminotransferase(ALT),aspartate aminotransferase(AST),triglyceride (TG) and high density lipoprotein (HDL) levels in different ultrasonographic groups.P values are for analysis of variance(post-hoc comparisons) considering the mild ultrasonographic group as the reference category.
Results
Among the 300 patients referred to the gastroenterology clinic,256 agreed to participate in the study and were interviewed (Step 1).Chronic liver diseases,alcohol consumption,and history of any hepatotoxic medications were recognized in 7 participants who were excluded (Step 2).After checking for the viral markers,4 participants were positive and were excluded (Step 3).Two hundred and forty-five participants,ranging from 18 to 77 years(108 males and 137 females) were included in the study.The reproducibility (ICC) and internal consistency(Cronbach's α) for ultrasonographic findings in two sessions ranged from 0.81 to 0.91 and 0.89 to 0.95 with medians of 0.87 and 0.93,respectively.The measure of agreement (κ) for ultrasonographic findings in two sessions in the same participant was 0.74 (P<0.01).
A comparison of age,BMI,laboratory concentrations(mean±standard deviation),gender,and presence of DM in the different USGs is shown in Table 1.
The ANOVA (post-hoc tests) comparisons of mean serum ALT,AST,TG and HDL levels in different USGs are shown in Fig.1.There was no statistically significant difference between mean ALT,AST,TG and HDL levels when the moderate and severe groups were compared(P=0.71,0.85,0.21 and 0.44,respectively).
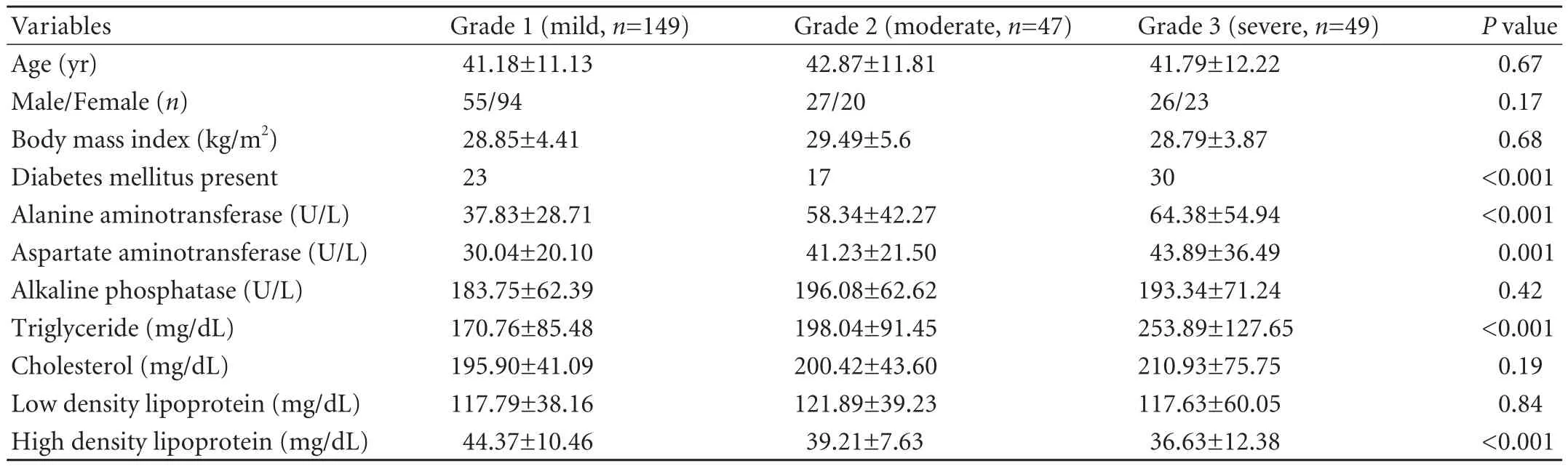
Table 1.Comparison of age,gender,body mass index,laboratory concentrations,and presence of diabetes mellitus in ultrasonographic groups (mean±SD)
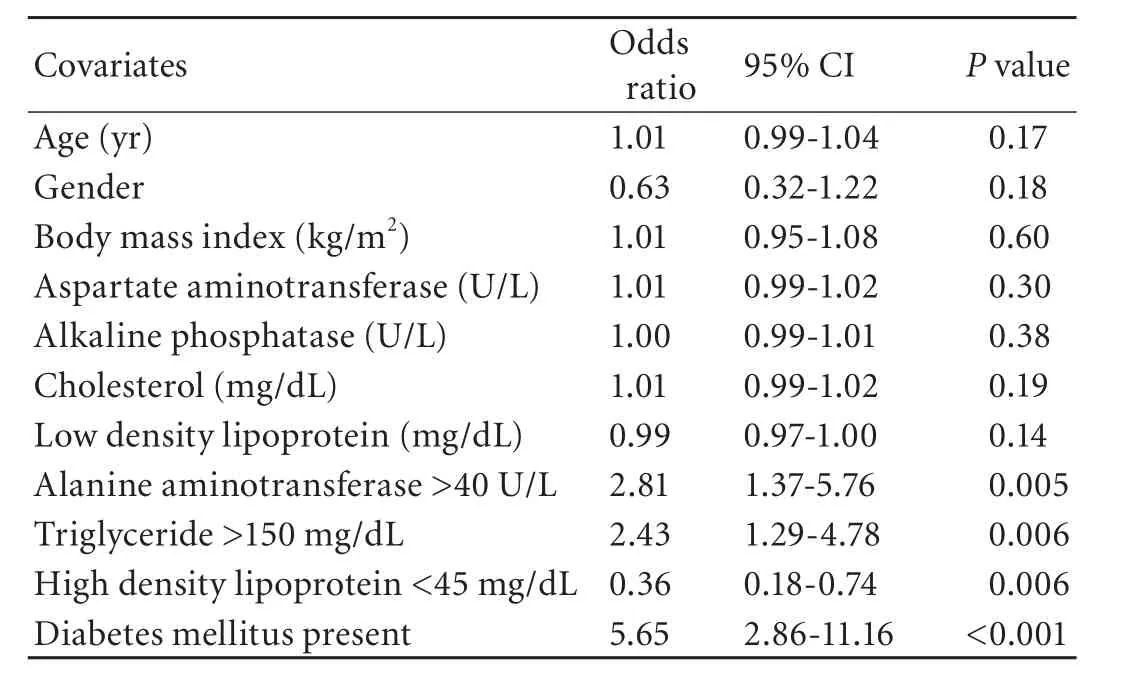
Table 2.Multivariate logistic regression analysis results for determination of variables independently associated with revised ultrasonographic groups
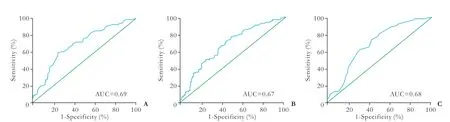
Fig.2.Optimal cut off values of serum alanine aminotransferase (A),triglyceride (B),and high density lipoprotein (C) concentrations in revised ultrasonographic groups by ROC curve analysis.AUC:area under the curve.
The multivariate logistic regression analysis results for determination of the variables independently associated with the revised USGs are shown in Table 2.
The optimal cut-off values of ALT,TG and HDL for differentiating between "mild" and "moderate to severe"USGs using ROC curve analysis are shown in Fig.2.The cut-off values of 32.5,162.5,and 38.5 mg/dL for ALT,TG,and HDL gave a sensitivity of 70%,72%,and 73.2%and a specificity of 62%,57%,and 59% respectively for differentiating between the revised USGs.
Discussion
This study,with an adequate sample size,evaluated the correlation between serum parameters and the severity of liver involvement at ultrasonography in a sample of NAFLD outpatients referred to a general hospital.Serum ALT,TG,and HDL levels were correlated with the severity of fatty liver at ultrasonography.Proper cutoff values were calculated for these serum parameters to differentiate "mild" from "moderate to severe" USGs.The results of our study are consistent with those showing that serum TG and ALT were correlated with the presence of fatty liver on ultrasonography.[22]Hamaguchi et al[23]declared that the abdominal ultrasonography scoring system was associated with the presence of metabolic syndrome components.Meanwhile,Rafeey et al[24]concluded that the severity of NAFLD at liver ultrasonography was correlated with elevation of ALT,AST,and total CHOL,and not with FBS and TG.We suggest that the controversy in the association of ultrasonographic staging with serum parameters in the previous studies might be due to inter-observer variability bias or limitations of the visual scaling system in grading the severity of liver involvement at ultrasonography.Liver ultrasonography was introduced as part of the routine examination and is required for early diagnosis of NAFLD complementary to laboratory investigations.[25]Ultrasonographic grading is based on the visual grading system and can identify the extent and severity of liver disease.This system has limitations and there is overlap between the ultrasonographic grades.Sometimes patients with the borderline ultrasonographic findings of moderate or severe might be misclassified as to either group.[26]
Subgroup analysis (post-hoc tests) in this study showed no statistically significant difference between the laboratory values when comparing the moderate and severe USGs.Therefore,the patients with moderate or severe ultrasonographic findings were merged and reclassified as the advanced group and then were compared with the less advanced group with mild fatty change in ultrasonography to overcome this visual grading system limitation.The mean laboratory values were not different when moderate and severe USGs were compared in this study.A previous study mentioned the weak points of the visual grading system for the separation of patients with moderate and severe ultrasonographic findings.[26]Therefore,we recommend that the currently used ultrasonographic grading of NAFLD has some limitations in differentiating the moderate and severe ultrasonographic groups.
There is a large body of evidence that increased ALT and TG and decreased HDL levels are associated with the severity of NAFLD.[20,22,27-29]In this study,the ultrasonographic findings were correlated with increased levels of ALT and TG and a decreased level of HDL,indicating that ultrasonography can be used properly to estimate the severity of disease.Serum ALP was not associated with the severity of fatty infiltration at ultrasonography in this study,in accord with the results of Altlparmak et al.[30]Total CHOL and LDL alone cannot be considered as indicators of insulin resistance and the newer metabolite,oxidized LDL,is proposed to be a better measure.Considering this fact,the lack of correlation between ultrasonographic grading and total CHOL and LDL in this study is not surprising.[31,32]AST is an intracellular enzyme that is released into serum when tissue injury and cell death occur.It is not a specific marker of hepatocyte damage and may be elevated in many other conditions unrelated to liver disease.[33,34]Therefore,the lack of correlation between the AST level and ultrasonographic grading in this study is reasonable.
Clinical findings are not sensitive methods for the diagnosis of NAFLD,especially at the early stage of disease.However,anthropometric measures like BMI and waist-to-hip ratio are believed to be helpful in this regard.BMI was previously considered as an important determinant for the severity of insulin resistance,however it is recognized that waist-to-hip ratio and abdominal fat content are more related to the survival of patients with metabolic syndrome.[35]So,the lack of association of ultrasonographic grading with BMI in this study suggests a search for newer techniques for the detection of visceral fat involved in the pathogenesis of NAFLD and not measuring the total body fat content.
Strengths and limitations
A radiologist and not a sonologist performed the liver ultrasonography in this study,giving more accurate and reliable results.In order to avoid inter-observer variability bias we used one expert radiologist to assess all liver sonographies.The intra-observer reliability of the ultrasonographic findings was good in this study according to the results of ICC and Cronbach's α.The κ value in this study showed good agreement between the two ultrasonographic findings in the same participant.We did not check for serum ferritin,anti-mitochondrial antibody,antinuclear antibody,and α-1 antitrypsin,which can be responsible for elevated serum ALT,as they are too infrequent to have had a major impact on our results.[3]
Liver biopsy is not always necessary to differentiate simple fatty liver from the more severe form (NASH).[7]In this study,liver biopsy was not performed,so the correlation of laboratory findings with ultrasonographic grading could not be separately evaluated in the simple fatty liver and NASH patients.In fact,the study population consisted of simple fatty liver patients and NASH patients with different severity.The lack of liver biopsy is a main limitation of this study,since evaluating the correlation of laboratory findings with ultrasonographic grading needs to be compared with a gold standard.
The ultrasonographic findings cannot differentiate fatty infiltration from hepaticfibrosis.[36]Sometimes the fat accumulation in the liver is not distributed homogenously and a localized fatty change may masquerade as a hepatic lesion.[37]The sensitivity and specificity of ultrasonography in detecting NAFLD is decreased in obese patients.[38]The operator dependency and inability to detect small changes in liver fat content over time are the limitations of B-ultrasonography in the diagnosis and follow-up of patients with NAFLD.[38]
Several sonographic indices,like hepato-renal contrast and spleen longitudinal diameter,for the better evaluation of NAFLD,were not assessed in this study.The hepato-renal contrast is an ultrasound index for the quantification of liver steatosis.Normal liver exhibits an echostructure similar to that of renal parenchyma.In fatty liver,the increased hepatic echogenicity creates hepato-renal contrast.Webb et al[39]assessed the severity of liver steatosis in a study of 93 patients with positive histology for chronic liver disease,according to the discrepancy in ultrasonographic liver-kidney densities.They reported that the hepato-renal index can quantify the severity of liver steatosis to a lower limit of 5%.
Another simple parameter,noninvasive and easy to measure,is spleen longitudinal diameter.As the study of Tarantino et al[40]showed,spleen diameter can differentiate between NAFLD and NASH better than both IL-6 and vascular endothelial growth factor,with values >116 mm predicting NASH.
Proton magnetic resonance spectroscopy is a newer technique that is already considered as the gold standard non-invasive method for detecting fatty liver.Kotronen et al[41]developed a liver fat score using proton magnetic resonance spectroscopy that predicted increased liver fat content with a sensitivity of 86% and a specificity of 71%.They also introduced a liver fat equation from which the liver fat percentage could be estimated.Bedogni et al[42]developed a fatty liver index based on BMI,waist circumference,TG and γ-glutamyl transferase that accurately predicted NAFLD in the general population.They suggested that the index might help physicians to select subjects for liver ultrasonography and intensified lifestyle counseling.
Serum high-sensitivity C-reactive protein,pentraxin 3,interleukin-6,cytokeratin-18,and tissue polypeptidespecific antigen are among the recent serum biomarkers that might be applied for the diagnosis and response to treatment in NAFLD.[43]
In conclusion,serum ALT,TG,and HDL concentrations seem to be associated with the staging of NAFLD at liver ultrasonography and might be used to predict the staging in these patients.Further investigations are recommended for the development of noninvasive methods like newer laboratory biomarkers and advanced imaging techniques to determine the extent of liver fat and the early diagnosis of the disease.
Acknowledgement:The authors extend their gratitude to the laboratory staff in Kashan Shahid Beheshti Hospital for their special help and support of this study.
Contributors:RM proposed the study.JR wrote the first draft.RM and JR analyzed the data.All authors contributed to the design and interpretation of the study and to further drafts.JR is the guarantor.
Funding:This study was supported by a grant from the Kashan University of Medical Sciences (5764).
Ethical approval:This study was carried out in accord with the ethical standards for human experimentation (Helsinki Declaration)and was approved by the Ethics Committee of Kashan University of Medical Sciences (5764).
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Neuschwander-Tetri BA,Caldwell SH.Nonalcoholic steatohepatitis:summary of an AASLD Single Topic Conference.Hepatology 2003;37:1202-1219.
2 Qian Y,Fan JG.Obesity,fatty liver and liver cancer.Hepatobiliary Pancreat Dis Int 2005;4:173-177.
3 Jamali R,Khonsari M,Merat S,Khoshnia M,Jafari E,Bahram Kalhori A,et al.Persistent alanine aminotransferase elevation among the general Iranian population:prevalence and causes.World J Gastroenterol 2008;14:2867-2871.
4 Merat S,Rezvan H,Nouraie M,Abolghasemi H,Jamali R,Amini- Kafiabad S,et al.Seroprevalence and risk factors of hepatitis A virus infection in Iran:a population based study.Arch Iran Med 2010;13:99-104.
5 Merat S,Rezvan H,Nouraie M,Jamali A,Assari S,Abolghasemi H,et al.The prevalence of hepatitis B surface antigen and anti-hepatitis B core antibody in Iran:a population-based study.Arch Iran Med 2009;12:225-231.
6 Fan JG,Peng YD.Metabolic syndrome and non-alcoholic fatty liver disease:Asian definitions and Asian studies.Hepatobiliary Pancreat Dis Int 2007;6:572-578.
7 Tarantino G,Conca P,Riccio A,Tarantino M,Di Minno MN,Chianese D,et al.Enhanced serum concentrations of transforming growth factor-beta1 in simple fatty liver:is it really benign? J Transl Med 2008;6:72.
8 Pacifico L,Celestre M,Anania C,Paolantonio P,Chiesa C,Laghi A.MRI and ultrasound for hepatic fat quantification:relationships to clinical and metabolic characteristics of pediatric nonalcoholic fatty liver disease.Acta Paediatr 2007;96:542-547.
9 Saadeh S,Younossi ZM,Remer EM,Gramlich T,Ong JP,Hurley M,et al.The utility of radiological imaging in nonalcoholic fatty liver disease.Gastroenterology 2002; 123:745-750.
10 Jamali R,Pourshams A,Amini S,Deyhim MR,Rezvan H,Malekzadeh R.The upper normal limit of serum alanine aminotransferase in Golestan Province,northeast Iran.Arch Iran Med 2008;11:602-607.
11 Verrijken A,Francque S,Mertens I,Talloen M,Peiffer F,Van Gaal L.Visceral adipose tissue and in flammation correlate with elevated liver tests in a cohort of overweight and obese patients.Int J Obes (Lond) 2010;34:899-907.
12 Tarantino G,Saldalamacchia G,Conca P,Arena A.Nonalcoholic fatty liver disease:further expression of the metabolic syndrome.J Gastroenterol Hepatol 2007;22:293-303.
13 Tarantino G,Colicchio P,Conca P,Finelli C,Di Minno MN,Tarantino M,et al.Young adult obese subjects with and without insulin resistance:what is the role of chronic in flammation and how to weigh it non-invasively? J In flamm(Lond) 2009;6:6.
14 Alavian SM,Mohammad-Alizadeh AH,Esna-Ashari F,Ardalan G,Hajarizadeh B.Non-alcoholic fatty liver disease prevalence among school-aged children and adolescents in Iran and its association with biochemical and anthropometric measures.Liver Int 2009;29:159-163.
15 Pendino GM,Mariano A,Surace P,Caserta CA,Fiorillo MT,Amante A,et al.Prevalence and etiology of altered liver tests:a population-based survey in a Mediterranean town.Hepatology 2005;41:1151-1159.
16 Vernon G,Baranova A,Younossi ZM.Systematic review:the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults.Aliment Pharmacol Ther 2011;34:274-285.
17 Zhang H,He SM,Sun J,Wang C,Jiang YF,Gu Q,et al.Prevalence and etiology of abnormal liver tests in an adult population in Jilin,China.Int J Med Sci 2011;8:254-262.
18 Charatcharoenwitthaya P,Lindor KD.Role of radiologic modalities in the management of non-alcoholic steatohepatitis.Clin Liver Dis 2007;11:37-54.
19 Schwenzer NF,Springer F,Schraml C,Stefan N,Machann J,Schick F.Non-invasive assessment and quantification of liver steatosis by ultrasound,computed tomography and magnetic resonance.J Hepatol 2009;51:433-445.
20 Kashyap SR,Diab DL,Baker AR,Yerian L,Bajaj H,Gray-McGuire C,et al.Triglyceride levels and not adipokine concentrations are closely related to severity of nonalcoholic fatty liver disease in an obesity surgery cohort.Obesity (Silver Spring) 2009;17:1696-1701.
21 Anderson KM,Odell PM,Wilson PW,Kannel WB.Cardiovascular disease risk profiles.Am Heart J 1991;121:293-298.
22 Leite NC,Salles GF,Araujo AL,Villela-Nogueira CA,Cardoso CR.Prevalence and associated factors of nonalcoholic fatty liver disease in patients with type-2 diabetes mellitus.Liver Int 2009;29:113-119.
23 Hamaguchi M,Kojima T,Itoh Y,Harano Y,Fujii K,Nakajima T,et al.The severity of ultrasonographic findings in nonalcoholic fatty liver disease re flects the metabolic syndrome and visceral fat accumulation.Am J Gastroenterol 2007;102:2708-2715.
24 Rafeey M,Mortazavi F,Mogaddasi N,Robabeh G,Ghaffari S,Hasani A.Fatty liver in children.Ther Clin Risk Manag 2009;5:371-374.
25 Fu CC,Chen MC,Li YM,Liu TT,Wang LY.The risk factors for ultrasound-diagnosed non-alcoholic fatty liver disease among adolescents.Ann Acad Med Singapore 2009;38:15-17.
26 Lee SS,Park SH,Kim HJ,Kim SY,Kim MY,Kim DY,et al.Non-invasive assessment of hepatic steatosis:prospective comparison of the accuracy of imaging examinations.J Hepatol 2010;52:579-585.
27 Oh SY,Cho YK,Kang MS,Yoo TW,Park JH,Kim HJ,et al.The association between increased alanine aminotransferase activity and metabolic factors in nonalcoholic fatty liver disease.Metabolism 2006;55:1604-1609.
28 Ozkol M,Ersoy B,Kasirga E,Taneli F,Bostanci IE,Ozhan B.Metabolic predictors for early identification of fatty liver using doppler and B-mode ultrasonography in overweight and obese adolescents.Eur J Pediatr 2010;169:1345-1352.
29 Jin HB,Gu ZY,Yu CH,Li YM.Association of nonalcoholic fatty liver disease with type 2 diabetes:clinical features and independent risk factors in diabetic fatty liver patients.Hepatobiliary Pancreat Dis Int 2005;4:389-392.
30 Altlparmak E,Koklu S,Yalinkilic M,Yuksel O,Cicek B,Kayacetin E,et al.Viral and host causes of fatty liver in chronic hepatitis B.World J Gastroenterol 2005;11:3056-3059.
31 Thomopoulos KC,Arvaniti V,Tsamantas AC,Dimitropoulou D,Gogos CA,Siagris D,et al.Prevalence of liver steatosis in patients with chronic hepatitis B:a study of associated factors and of relationship withfibrosis.Eur J Gastroenterol Hepatol 2006;18:233-237.
32 Nakhjavani M,Khalilzadeh O,Khajeali L,Esteghamati A,Morteza A,Jamali A,et al.Serum oxidized-LDL is associated with diabetes duration independent of maintaining optimized levels of LDL-cholesterol.Lipids 2010;45:321-327.
33 Ye J,Chen Z,Wang T,Tong J,Li X,Jiang J,et al.Role of tissue disorder markers in the evaluation of disease progress and outcome prediction:a prospective cohort study in noncardiac critically ill patients.J Clin Lab Anal 2010;24:376-384.
34 Wu SW,Wu LF,Wang Q,Zhang WY.Risk factors of adverse pregnancy outcomes during expectant management of early onset severe pre-eclampsia.Zhonghua Fu Chan Ke Za Zhi 2010;45:165-169.
35 Czernichow S,Kengne AP,Huxley RR,Batty GD,de Galan B,Grobbee D,et al.Comparison of waist-to-hip ratio and other obesity indices as predictors of cardiovascular disease risk in people with type-2 diabetes:a prospective cohort study from ADVANCE.Eur J Cardiovasc Prev Rehabil 2011;18:312-319.
36 Joy D,Thava VR,Scott BB.Diagnosis of fatty liver disease:is biopsy necessary? Eur J Gastroenterol Hepatol 2003;15:539-543.
37 Wang SS,Chiang JH,Tsai YT,Lee SD,Lin HC,Chou YH,et al.Focal hepatic fatty infiltration as a cause of pseudotumors:ultrasonographic patterns and clinical differentiation.J Clin Ultrasound 1990;18:401-409.
38 Mottin CC,Moretto M,Padoin AV,Swarowsky AM,Toneto MG,Glock L,et al.The role of ultrasound in the diagnosis of hepatic steatosis in morbidly obese patients.Obes Surg 2004;14:635-637.
39 Webb M,Yeshua H,Zelber-Sagi S,Santo E,Brazowski E,Halpern Z,et al.Diagnostic value of a computerized hepatorenal index for sonographic quantification of liver steatosis.AJR Am J Roentgenol 2009;192:909-914.
40 Tarantino G,Conca P,Pasanisi F,Ariello M,Mastrolia M,Arena A,et al.Could in flammatory markers help diagnose nonalcoholic steatohepatitis? Eur J Gastroenterol Hepatol 2009;21:504-511.
41 Kotronen A,Peltonen M,Hakkarainen A,Sevastianova K,Bergholm R,Johansson LM,et al.Prediction of nonalcoholic fatty liver disease and liver fat using metabolic and genetic factors.Gastroenterology 2009;137:865-872.
42 Bedogni G,Bellentani S,Miglioli L,Masutti F,Passalacqua M,Castiglione A,et al.The Fatty Liver Index:a simple and accurate predictor of hepatic steatosis in the general population.BMC Gastroenterol 2006;6:33.
43 Fierbinteanu-Braticevici C,Dina I,Petrisor A,Tribus L,Negreanu L,Carstoiu C.Noninvasive investigations for non alcoholic fatty liver disease and liverfibrosis.World J Gastroenterol 2010;16:4784-4791.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Disease spectrum and use of cholecystolithotomy in gallstone ileus
- Xanthogranulomatous cholecystitis mimicking gallbladder cancer and causing obstructive cholestasis
- Liver transplantation in Crigler-Najjar syndrome type I disease
- High-intensity focused ultrasound ablation as a bridging therapy for hepatocellular carcinoma patients awaiting liver transplantation
- Laparoscopic distal pancreatectomy with or without splenectomy:spleen-preservation does not increase morbidity
- Expression of HBx protein in hepatitis B virusinfected intrahepatic cholangiocarcinoma