Double inferior vena cava does not complicate para-aortic nodal dissection for the treatment of pancreatic carcinoma
2012-06-11
Rome,Italy
Introduction
Duplication of the inferior vena cava (IVC)involves large veins on both sides of the aorta that join anteriorly at the level of the renal arteries to become the suprarenal IVC.This anomaly has a prevalence of 0.2% to 0.5%.It occurs because the left supracardinal vein fails to regress and both postrenal segments of the supracardinal veins persist.The left IVC mostly ends at the level of the left renal vein,which crosses anteriorly to the aorta to join the right IVC.[1]
Double IVC complicating para-aortic lymphadenectomy has been reported in patients suffering from gynecological malignancy.[2,3]The prevalence of paraaortic lymph node metastasis in carcinoma of the pancreatic head has been reported to range from 13%to 19%.In pancreatic cancer,with respect to longterm survival,the benefit of pancreaticoduodenectomy with extended lymphadenectomy in comparison with pancreaticoduodenectomy with standard lymphadenectomy has not been demonstrated.[4,5]Even if the prognosis of patients with para-aortic nodal metastasis is worse than that of patients without para-aortic nodal involvement,[6]the occurrence of para-aortic (i.e.,nonregional) nodal disease,particularly if not apparent preoperatively,cannot be considered a contraindication for radical surgery because long-term survivors after resection have been reported.[7,8]In addition,adjuvant postoperative chemotherapy may contribute to improving the outcome of patients with para-aortic nodal involvement.[6,7]Moreover,the lymph node ratio (i.e.,ratio of metastatic to examined nodes) and the number of metastatic nodes have been reported to be independent prognostic factors after potentially curative resections of pancreatic carcinoma.[9-11]Hellan and colleagues reported that the resection and examination of higher numbers of lymph nodes are associated with improved survival after pancreatectomy in node-negative pancreatic cancer.[12]However,the lymph node ratio,the number of metastatic nodes,as well as the number of excised nodes,are dependent upon the extent of lymphadenectomy as limited dissection provides a smaller number of lymph nodal retrieval and may overlook potential metastatic nodes.[10,11]Then,apart from debatable therapeutic impact,the attempt to resect and examine an adequate number of lymph nodes in pancreatic carcinoma is essential for accurate prognostic evaluation.[10,11]
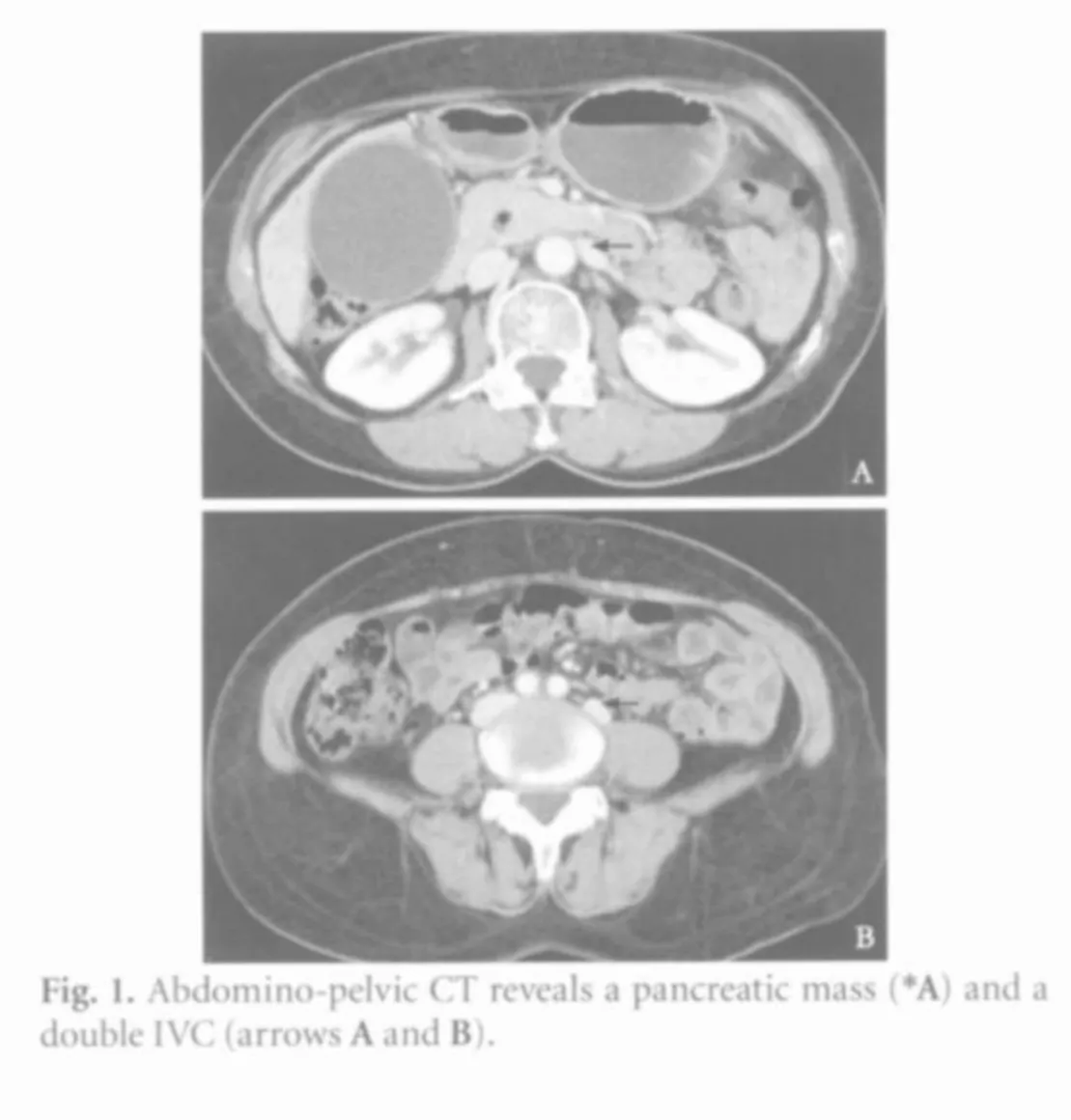
We report CT scan and intraoperative images of a patient with duplication of the IVC who underwent pancreaticoduodenectomy with extended lymphadenectomy for carcinoma of the pancreatic head.
Clinical images
A 66-year-old female with a history of intermittent abdominal pain,weight loss,nausea and anorexia presented at our department.Clinical and imaging findings were suggestive of malignancy of the head of the pancreas.CT showed a hyper-vascularized pancreatic mass (maximum diameter 2.6 cm) involving the periampullary region with dilation of the biliary duct,gallbladder and intra-hepatic biliary tree.The diameter of the main pancreatic duct was normal.Regional nodal or distant metastasis was not observed.A double IVC was shown (Fig.1).
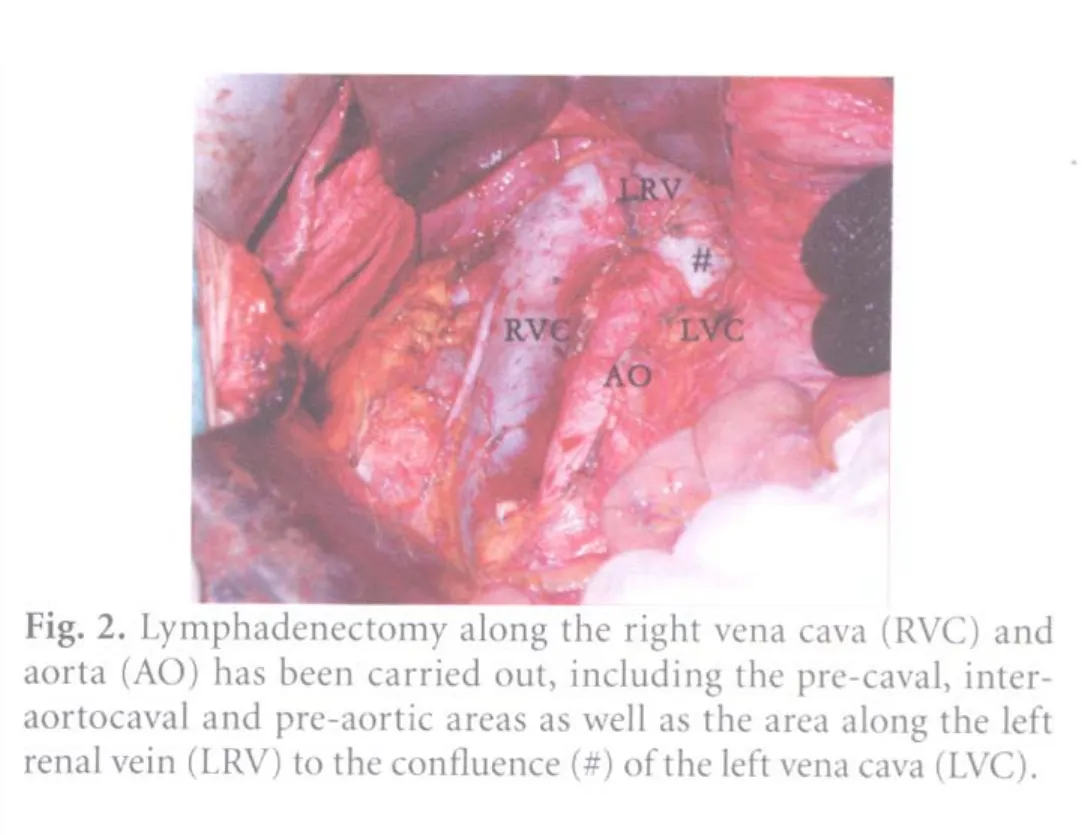
A pancreaticoduodenectomy with extended lymphadenectomy was undertaken.Para-aortic lymphadenectomy of the 16a1,16a2 and 16b1 areas along the right vena cava and aorta was done,including the pre-caval,interaortocaval and pre-aortic areas,as well as the area along the left renal vein to the con fluence of the left caval vein(Fig.2).Lymphadenectomy along the left IVC including the left inter-aortocaval area (left latero-aortic area) was not carried out.
Definitive histology confirmed the intraoperative diagnosis of pancreatic carcinoma:moderately differentiated pancreatic adenocarcinoma with lymphatic invasion but no involvement of excised regional (16 in number) and para-aortic (13 in number) lymph nodes (G2 pT1N0M0 L1 V0 Pn0).The patient had an uneventful postoperative recovery and was disease-free at a 17-month follow-up.
Discussion
Several cases of double IVC complicating para-aortic lymphadenectomy for gynecological malignancy have been reported;[2,3]in these cases lymph node dissection was performed along both the right IVC in its normal position as well as the abnormal left IVC running laterally to the aorta.According to TNM classification[13]para-aortic lymph nodes are regional lymph nodes for gynecological carcinomas:lymphatics which flow from the ovary,endometrium or cervix uteri reach the abdomino-pelvic lymph nodes running together with the respective blood vessels.In case of double IVC,venous out flow from the left side of the pelvis drains mainly into the left IVC,and venous blood flow from the right side of the pelvis drains into the right IVC;[14]then for radical dissection in patients with gynecological carcinomas and double IVC,a bilateral para-aortic lymphadenectomy including the area of the left IVC is necessary.[2,3,14]
In the absence of caval anatomic anomalies,the highest incidence of para-aortic nodal metastasis in cancer of the head of the pancreas has been shown to be in the inter-aortocaval and pre-aortic 16a2 and 16b1 areas; in particular the 16b1 inter-aortocaval segment is considered to be the most important site in the early stage of para-aortic metastasis.[15]The study by Deki and Sato on minute dissection of four adult cadavers showed that the lymphatics of the anterior surface of the head of the pancreas and the lymphatics of the neck of the pancreas through different pathways terminate in lymphonodus celiacomesentericus dexter superficialis which is situated to the right of the origins of the celiac trunk and the superior mesenteric artery and is connected with lymphonodus celiacomesentericus dexter profundus:this last,which is found behind the former,receiving the lymphatics which arise from the posterior surface of the pancreatic head,drains almost all vessels derived from the right half of the pancreas.The efferents of this lymph node reach the inter-aortocaval nodes lying in the upper and lower angles formed by the IVC and the left renal vein (i.e.,the 16a2 and 16b1 interaortocaval areas).Lymphatics from the left half of the pancreas terminate in lymphonodus celiacomesentericus sinister located to the left of the origins of the celiac trunk and superior mesenteric artery; the efferents of this lymph node arrive at the left latero-aortic nodes lying above and below the left renal vein (i.e.,16a2 and 16b1 latero-aortic areas).[16]Then,unlike para-aortic lymphadenectomy for gynecological carcinomas in patients with double IVC,in the case of patients with double IVC who undergo pancreaticoduodenectomy with extended lymphadenectomy for carcinoma of the pancreatic head,particularly in the absence of preoperative appearance of para-aortic disease,lymphadenectomy along the left caval vein including the left inter-aortocaval area (left latero-aortic area) is not necessary and not carried out.
Contributors:PN proposed the study,analyzed the data and wrote the first draft.MRL and FG collected the data.All the authors contributed to the design and conclusions of the study.CP supervised the study and the further drafts.
Funding:None.
Ethical approval:Not needed.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Giordano JM,Trout HH 3rd.Anomalies of the inferior vena cava.J Vasc Surg 1986;3:924-928.
2 Strauss A,Kuemper C,Mundhenke C,Schaefer F,Jonat W,Hilpert F.Congenital retroperitoneal vascular anomalies:impact on pelvic surgery.Arch Gynecol Obstet 2011;284:1169-1173.
3 Ashraf M,Secrist RD.Bilateral paraaortic lymphadenectomy in the presence of double inferior vena cava.Gynecol Oncol 1989;33:251-254.
4 Pavlidis TE,Pavlidis ET,Sakantamis AK.Current opinion on lymphadenectomy in pancreatic cancer surgery.Hepatobiliary Pancreat Dis Int 2011;10:21-25.
5 Yokoyama Y,Nagino M.Role of extended surgery for pancreatic cancer:critical review of the four major RCTs comparing standard and extended surgery.J Hepatobiliary Pancreat Sci 2011 Aug 12.
6 Kanda M,Fujii T,Nagai S,Kodera Y,Kanzaki A,Sahin TT,et al.Pattern of lymph node metastasis spread in pancreatic cancer.Pancreas 2011;40:951-955.
7 Murakami Y,Uemura K,Sudo T,Hashimoto Y,Yuasa Y,Sueda T.Prognostic impact of para-aortic lymph node metastasis in pancreatic ductal adenocarcinoma.World J Surg 2010;34:1900-1907.
8 Yamada S,Nakao A,Fujii T,Sugimoto H,Kanazumi N,Nomoto S,et al.Pancreatic cancer with paraaortic lymph node metastasis:a contraindication for radical surgery?Pancreas 2009;38:e13-17.
9 Bhatti I,Peacock O,Awan AK,Semeraro D,Larvin M,Hall RI.Lymph node ratio versus number of affected lymph nodes as predictors of survival for resected pancreatic adenocarcinoma.World J Surg 2010;34:768-775.
10 Sahin TT,Fujii T,Kanda M,Nagai S,Kodera Y,Kanzaki A,et al.Prognostic implications of lymph node metastases in carcinoma of the body and tail of the pancreas.Pancreas 2011;40:1029-1033.
11 Murakami Y,Uemura K,Sudo T,Hayashidani Y,Hashimoto Y,Nakashima A,et al.Number of metastatic lymph nodes,but not lymph node ratio,is an independent prognostic factor after resection of pancreatic carcinoma.J Am Coll Surg 2010;211:196-204.
12 Hellan M,Sun CL,Artinyan A,Mojica-Manosa P,Bhatia S,Ellenhorn JD,et al.The impact of lymph node number on survival in patients with lymph node-negative pancreatic cancer.Pancreas 2008;37:19-24.
13 Sobin L,Gospodarowicz M,Wittekind C,eds.TNM classification of malignant tumors.Oxford:Wiley-Blackwell;2009.
14 Strauss A,Kuehnle E,Hilpert F,Kanzow M,Jonat W,Kuemper C.Double inferior vena cava:a crucial finding complicating para-aortic lymphadenectomy.Eur J Obstet Gynecol Reprod Biol 2011;154:228-289.
15 Nagakawa T,Kobayashi H,Ueno K,Ohta T,Kayahara M,Miyazaki I.Clinical study of lymphatic flow to the paraaortic lymph nodes in carcinoma of the head of the pancreas.Cancer 1994;73:1155-1162.
16 Deki H,Sato T.An anatomic study of the peripancreatic lymphatics.Surg Radiol Anat 1988;10:121-135.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Clinical outcome in patients with hilar malignant strictures type II Bismuth-Corlette treated by minimally invasive unilateral versus bilateral endoscopic biliary drainage
- Cerebral protective effect of nicorandil premedication on patients undergoing liver transplantation
- Steroid elimination within 24 hours after orthotopic liver transplantation:effectiveness and tolerability
- Association of polymorphisms in non-classic MHC genes with susceptibility to autoimmune hepatitis
- Correlation of the occurrence of YMDD mutations with HBV genotypes,HBV-DNA levels,and HBeAg status in Chinese patients with chronic hepatitis B during lamivudine treatment
- Efficacy and factors in fluencing treatment with peginterferon alpha-2a and ribavirin in elderly patients with chronic hepatitis C