Clinical outcome in patients with hilar malignant strictures type II Bismuth-Corlette treated by minimally invasive unilateral versus bilateral endoscopic biliary drainage
2012-06-11
Belgrade,Serbia
Introduction
Endoscopic drainage of hilar tumors has been the palliative method of choice for most patients for the last several decades.[1-3]Among all malignant biliary obstructions caused by a heterogeneous group of tumors,<30% are suitable for curative resection.[4]The extent of duct involvement may be classified as suggested by Bismuth and Corlette who divided all hilar tumors into groups I-IV.[5]Although endoscopic drainage has proven itself as the means of relieving symptoms and increasing the quality of life,it has been associated with the potential introduction of complications,some being life-threatening,like cholangitis.Over the years,many studies have been conducted to assess the best way to maintain bile drainage and at the same time avoid complications.[6-9]There were some con flicting results concerning unilateral versus bilateral stenting.While some authors strongly suggested bilateral stenting,[6,7]others did not demonstrate the advantages of bilateral drainage.[8]There is also a question of the percentage of liver volume be drained in order to relieve jaundice and prolong survival.[9,10]A pre-ERCP (endoscopic retrograde cholangiopancreatography) assessment of liver volume distribution by cross-sectional imaging has been considered a way to optimize endoscopic procedures.[9,11]MRCP has so far shown itself to be most informative and valuable help for the therapist in procedure planning as described by Hintze et al.[11]The primary endpoint of this study was to compare unilateral versus bilateral drainage in hilar malignant strictures Bismuth type II by a combination of non-invasive imaging (MRCP) and therapeutic ERCP,and by following the clinical picture and biochemical parameters.The secondary endpoint regarded assessment of the justifiability of a blind cannulation method in this specific group of patients.
Methods
A two-center prospective study was conducted from 2007 to 2009 in the "Dr Dragisa Misovic-Dedinje" Clinical Hospital Center,Belgrade,Serbia and in the "Danilo I" General Hospital,Cetinje,Montenegro.The study included 39 consecutive patients with malignant hilar stenosis due to cholangiocarcinoma or gallbladder cancer,all being unsuitable for surgical resection because of general condition or extent of the malignant process.Full and informed consent was obtained from all patients for the clinically-indicated procedure and for participation in the study.The study was approved by the Ethics Committee of the Internal Review Board followed by definitive approval from the Ministry of Health(decision 01-235/2).Prior to therapeutic intervention,all patients were subjected to non-invasive imaging,abdominal ultrasound,computed tomography scan and MRCP,in order to assess the extent of malignancy,to classify patients by Bismuth-Corlette grade,and to facilitate cannulation by comparing MRCP images with the fluoroscopic picture.The 64-slice multislice computed tomography (MSCT) was performed in two Clinical Centers in Belgrade and one in Podgorica which were equipped with 1.5 Tesla devices.Bismuth type II malignant hilar obstruction was considered as the morphological form with involvement of the bifurcation without involvement of the secondary intrahepatic ducts.
Only Bismuth type II malignant hilar obstructions were included in the study.The inclusion criteria were:inoperability,Bismuth type II stenosis,pre-procedural MRCP to assess the extent of the lesion and plan the procedure,and successful cannulation of at least one hepatic duct during ERCP.The exclusion criteria were:previous surgical intervention on the biliary tree,and severe coagulopathy or cardiopulmonary comorbidity.Preoperative cholangitis was excluded by clinical examination and measuring the biochemical parameters of in flammation.Liver function tests were performed routinely in all patients.In one patient who also had alcoholic liver cirrhosis,the Child-Turcotte-Pugh score(CTPS) was calculated.In other patients,previous chronic viral liver disease or cirrhosis was excluded so there was no need to classify them according to CTPS.Only patients with successful stent placement were included.
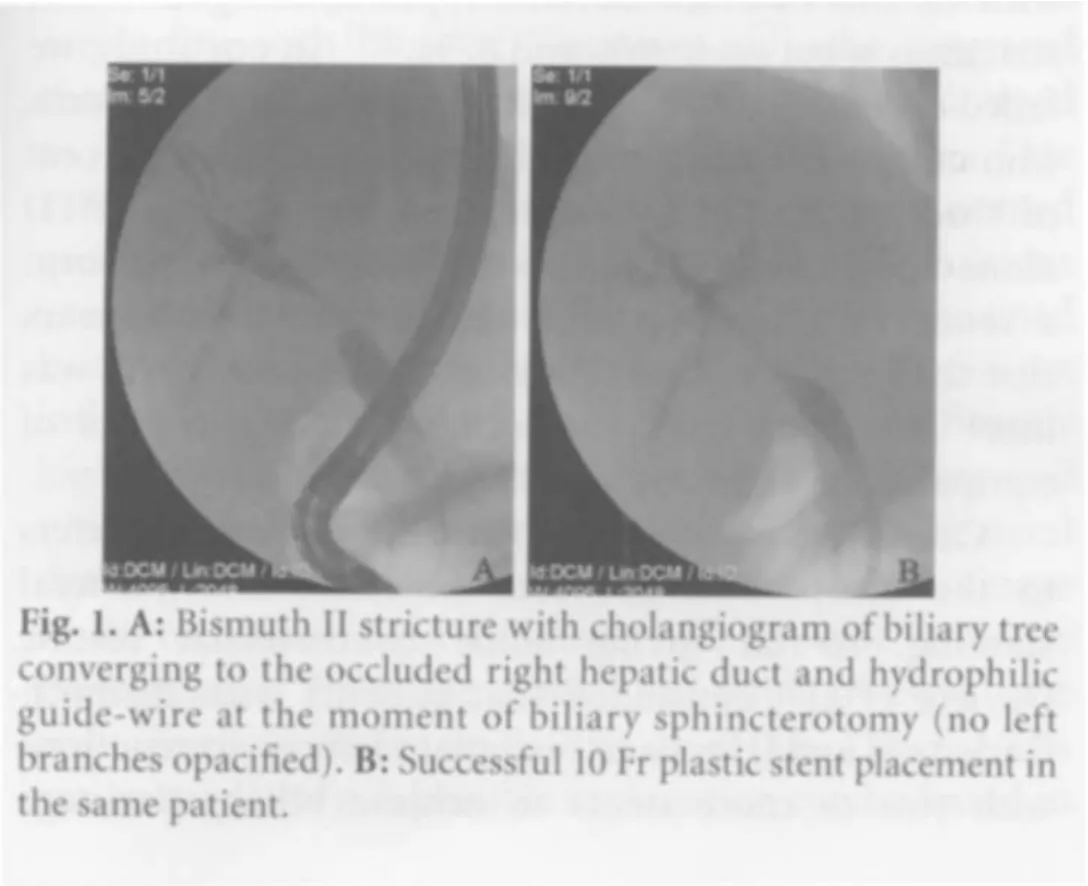
The included patients were treated by placing unilateral or bilateral biliary stents via therapeutic ERCP to relieve jaundice.All procedures were conducted by three skilled and experienced endoscopists,each performing more than 300 ERCPs yearly and with more than 10 years of ERCP experience.Premedication consisted of 3-5 mg midazolam and 0.5 mg fentanyl.The procedure started with a deep common bile duct cannulation with a standard double-lumen sphincterotome followed by an attempt to cannulate both occluded hepatic ducts with a sterile with a sterile fully coated hydrophilic RF-GS35403M radio focus guide wire M Terumo.The water-soluble contrast medium (Ultravist-300,Bayer) was never used before cannulation and was successfully achieved with the guide-wire in order to prevent possible contamination of occluded bile ducts.Then the cannulated bile ducts were opacified with contrast.Subsequently biliary sphincterotomy was performed in all patients to facilitate stent placement (Fig.1A).Dilatation of the stenosis was accomplished with a mechanical catheter or pneumatic dilatators.Hydromer-coated polyurethane angled asymmetric stents (10 Fr and 11.5 Fr) were then inserted via a guide-wire,guiding catheter (6 Fr) and pusher tube (10 Fr) system (Fig.1B).The stents were inserted in the bile ducts that had been opacified.A guide-wire exchange from soft to stiff was performed in some cases in order to facilitate stent placement.Successful stent insertion was defined as passage of the stent across the stricture,followed by the flow of contrast and bile through it.Every bile duct which had been opacified was drained.In cases of failed bile duct cannulation,the patients were referred for a further percutaneous transhepatic drainage procedure (PTD),followed by an eventual rendezvous approach.During the ERCP,endoscopic biopsies were obtained to determine the histological type of the tumor.Prophylactic treatment with broad-spectrum antibiotics was continued for 7 days after the procedure(Amoxicillin 1.5 g/day,oral).The patients were followed up for the next 12 months,with stent exchange every 3 months.If the symptoms of jaundice worsened,an earlier stent exchange was considered.Follow-up consisted of previously scheduled abdominal ultrasound examination and analyses of biochemical parameters.
Patients were divided into two groups.Group A had unilateral and group B had bilateral drainage.Unfortunately,this was not a randomized control study and patients were allocated to the groups during the procedure,depending on whether one or two bile ducts were cannulated.Parameters followed were bilirubin level before and 7 days after the procedure and the incidence of early and late complications.Early complications (within 48 hours) were cholangitis and acute pancreatitis while late complications were stent migration and stent clogging.Additional statistical analyses were conducted to compare some characteristics of unilateral left versus unilateral right drainage as well as between each versus bilateral drainage.The primary outcome was assessed by patient survival in the first 12 months after the procedure.
The SPSS 17.0 program was used for statistical analyses.Data were analyzed using Student's t test,the chi-square test,the Kruskal-Wallis test,the Mann-Whitney U test and Wilcoxon's rank-sum test.A P value<0.05 was considered statistically significant.
Results
All the 49 patients were treated with ERCP while 39(79.59%) had successful stent placements,so 39 were included in the per-protocol analyses.The patient who also had alcoholic liver cirrhosis was classified as CTPS class B (increased bilirubin level,slight ascites,mild hypoalbuminemia,9 points).The patients with unsuccessful ERCP were further treated by PTD.In two patients from this group,a rendezvous technique was performed,showing that the strictures in these patients could not have been resolved by the initial ERCP procedure.
In the 39 patients,ERCP confirmed the Bismuth-Corlette staging previously done on the basis of MRCP.Of these patients,32 had hilar cholangiocarcinoma (82%)while 7 had gallbladder cancer (18%).The diagnosis was confirmed in 8 patients by fluoroscopy guided endoscopic biopsies during the ERCP and in the rest was assumed on the basis of imaging and clinical outcome.
Unilateral drainage was performed on 21 patients(group A) while 18 had bilateral drainage (group B).There was no statistically significant difference in age and sex structure as well as in histological type of tumor distribution between the groups (Table 1).A total of 57 plastic stents were used (10 Fr,89%,%; 11.5 Fr,11%).
A marked decrease of serum bilirubin was recorded in both groups.Pre-treatment levels of bilirubin were not different between the groups,and group B showed a significantly lower level 7 days after the procedure(Table 2).The incidences of early complications were not different between the groups (Table 2).In groupA,2 cases of cholangitis were noted versus 1 case in group B,while in each group 1 case of pancreatitis was noted.The patients with cholangitis were successfully treated by repeated ERCP and antibiotic therapy (2 g/day ceftriaxone and 1.5 g/day metronidazol).The patients with mild post-ERCP pancreatitis were treated conservatively and followed by regular abdominal computed tomography scans.There was a significant difference in the incidence of late complications,being more often in group B (Table 2).Stent migration was noted in 1 case in group A versus 4 in group B,while stent clogging occurred in 2 members of group A,and 4 in group B.All were regularly treated with stent replacement.The first stent replacement after 3 months was successful in 87% of patients (four died from disease progression and one from cardiopulmonary insufficiency),showing no statistical difference between the groups.The second stent replacement 6 months after the procedure was done in 72% patients,with no statistical difference in survival rate between the groups.Atfinal follow-up the survival rate was 18%(7):4 patients from group A and 3 from group B (no significant difference).
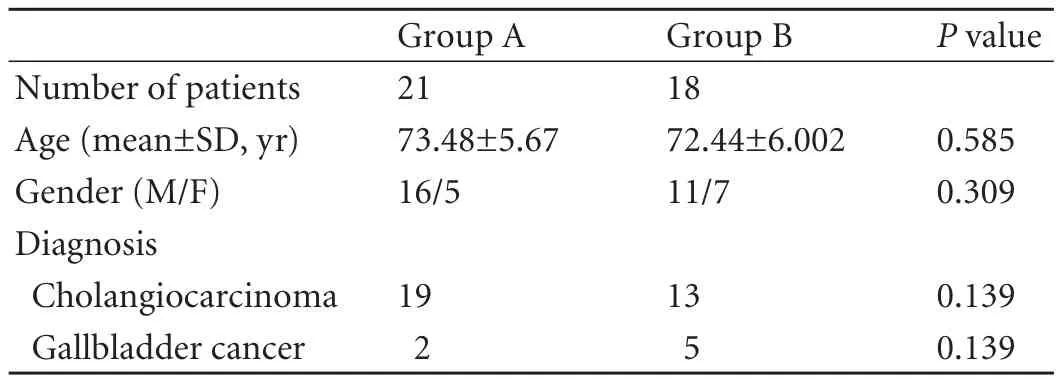
Table 1.Epidemiological characteristics of patients included in this study
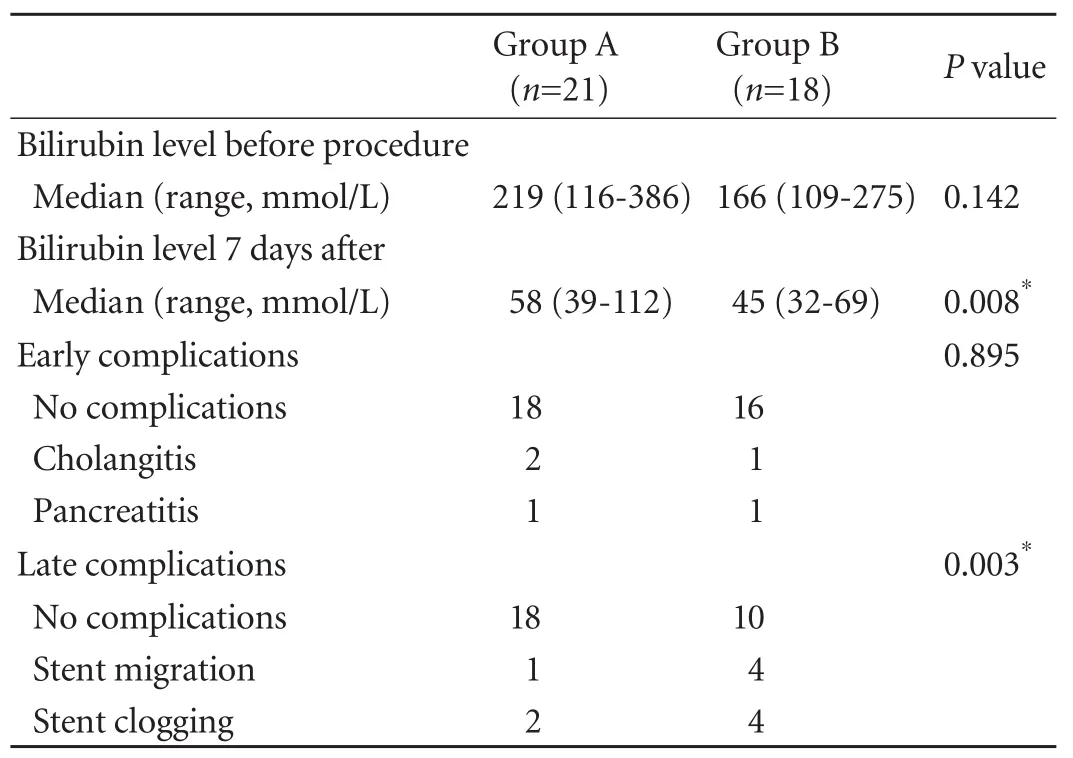
Table 2.Drainage performance in unilateral versus bilateral drainage of malignant hilar strictures Bismuth-Corlette type II
The serum bilirubin values were also compared among the groups of patients who underwent only unilateral left,only unilateral right or bilateral drainage(Fig.2).The analyses showed no statistical difference between the groups with unilateral left and unilateral right drainage in pre-procedure bilirubin level (P=0.293)as well as at 7 days after the procedure (P=0.507).Both bilirubin levels were not different between the unilateral left drainage group and the bilateral drainage group(P=0.083 and 0.142).On the other hand,the unilateral right drainage group showed no difference from the bilateral drainage group in pre-procedure bilirubin level(P=0.416),they did differ at 7 days after the procedure(P=0.007),bilirubin level being higher in patients with unilateral right drainage.
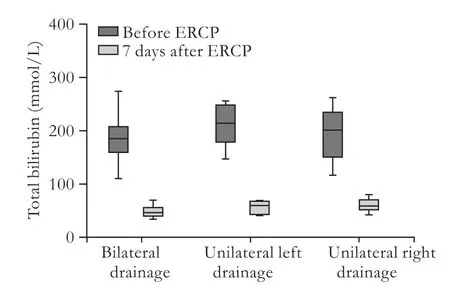
Fig.2.Unilateral left versus unilateral right drainage.
Discussion
Malignant hilar obstructions are associated with poor prognosis with <10% of patients surviving 5 years after diagnosis and most patients dying in the first year.[12,13]Less that 30% of all hilar tumors are suitable for surgical resection[4]while the resection itself is associated with a high operative mortality.[14-17]
Endoscopic drainage is the palliative method of choice[1-3]prolonging patient survival and increasing quality of life.Endoscopic stent placement is now accepted as the first-line palliative treatment for these patients,[8]and may play a future role in chemotherapy with the development of stents carrying chemotherapeutic drugs as some predict.[18]
Since the introduction of endoscopic drainage,many studies have been conducted to assess the best way to accomplish biliary drainage and avoid complications.[6-10,19]
Unsuccessful stent placement in studies dealing with various Bismuth-Corlette types of malignant hilar strictures is between 96% and 87%.[6-9]In our study,we failed to cannulate occluded bile ducts in 10 patients,who underwent a further PTD approach.Eighty percent of these patientsfinished treatment by external PTD alone and in only 2 patients we were able to perform a rendezvous technique as well.However,it appears that the morphological tightness of these strictures was more important than the technical characteristics of equipment or endoscopic skills.
One of the main questions needing an answer refers to the comparison between unilateral and bilateral stenting,so far giving some controversial results.Deviere et al[6]concluded that patients with Bismuth-Corlette II and III type of malignant biliary obstructions with two or more stents to achieve biliary drainage have an improved survival rate and a lower procedurerelated mortality as well as the lower incidence of early and late complications.Chang et al[7]have also provided results in favor of bilateral drainage.Contrary to this,Polydorou et al[19]compared the results of right versus left hepatic duct stent insertion,and concluded that more than 1 stent is not justified as a routine procedure.A similar conclusion was reached by De Palma et al[8]who found that insertion of more than one stent is no more effective and increases the risk of further procedure-related complications and mortality.Our study was limited to Bismuth-Corlette type II malignant biliary obstructions treated by the insertion of plastic stents.We attempted to contribute to a consensus in therapeutic approach in this particular question.The study was designed to compare unilateral and bilateral drainage in patients with successfully inserted plastic stents.Following the recommendations,[11,20-22]preprocedural MRCP evaluation of lesions was performed to determine the obstruction type and plan the procedure.
The results showed that serum bilirubin levels were significantly lower 7 days after the procedure in patients treated with bilateral stenting,but the incidence of late complications in the bilateral stented group was higher.The incidence of early complications,especially cholangitis,was not different between the groups.A probable explanation of this is that we tried to follow the criteria given in the study by Chang et al[7]concluding that a low survival rate was associated with opacification of both lobes and drainage of only one.During the procedures in our study,minimal contrast medium was used and every bile duct opacified was drained.Also,we took a minimally invasive approach,trying not to be too aggressive using the guide-wires or catheters,since trauma is one of the main triggers for cholangitis.In our study,bilateral stenting gave better drainage results.The results are in line with those of Vienne et al[9]who suggested that >50% of the liver volume needed to be drained to accomplish sufficient drainage effectiveness.Late complications were more frequent in the bilateral stented group.Considering the nature of the late complications(stent clogging and stent migration),this can be explained by the number of stents implanted.These results did not in fluence the survival rate which was not significantly higher in the bilaterally stented group.We also compared unilateral left and right drainage and each with bilateral drainage.The results favored unilateral left drainage while unilateral right drainage had a worse drainage performance.From the anatomical point of view,the right liver lobe drains up to 70% of all bile.These results are contradictory.A possible explanation can be found in the anatomical variations,which were present in greater numbers in our group than in the average population due to a small number of patients included in the study or in the nature of the strictures,occluding the right biliary duct more aggressively and therefore making drainage more difficult.
Although this was not a randomized control study and the number of patients was rather small,it focused on the specific subgroup of patients with malignant biliary strictures.On the other hand,there are still no randomized control studies of patients with Bismuth-Corlette type II malignant strictures only.What can be concluded from this study is that a minimally invasive approach following the criterion that every opacified bile duct needs to be drained and trying to be less aggressive is associated with lower incidence of early complications,especially cholangitis.Since the clinical outcome measured by bilirubin level was lower in patients with bilateral drainage 7 days after the procedure,it can be assumed that drainage of 50% or more of the liver volume leads to sufficiently effective drainage.However,the one year survival rate was unfortunately low and it was not dependent on whether one or both hepatic ducts were drained.
Contributors:BM wrote the manuscript; BM and BM performed procedures and collected samples.PN contributed to manuscript writing and sample processing.SR,PR and SP edited the manuscript.RM and ZM revised the manuscript.IT provided analytical tools and analyzed results.
Funding:This study was supported by the Ministry of Education and Science of the Republic of Serbia (175054).
Ethical approval:The study was approved by the Ethics Committee of the Internal Review Board followed by definitive approval from the Ministry of Health (decision 01-235/2).
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Soehendra N,Reynders-Frederix V.Palliative bile duct drainage-a new endoscopic method of introducing a transpapillary drain.Endoscopy 1980;12:8-11.
2 Tytgat GN,Bartelsman JF,Den Hartog Jager FC,Huibregtse K,Mathus-Vliegen EM.Upper intestinal and biliary tract endoprosthesis.Dig Dis Sci 1986;31:57S-76S.
3 Lammer J,Neumayer K,Steiner H.Biliary endoprostheses in tumors at the hepatic duct bifurcation.Eur J Radiol 1986;6:275-279.
4 de Groen PC,Gores GJ,LaRusso NF,Gunderson LL,Nagorney DM.Biliary tract cancers.N Engl J Med 1999;341:1368-1378.
5 Bismuth H,Corlette MB.Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver.Surg Gynecol Obstet 1975;140:170-178.
6 Deviere J,Baize M,de Toeuf J,Cremer M.Long-term followup of patients with hilar malignant stricture treated by endoscopic internal biliary drainage.Gastrointest Endosc 1988;34:95-101.
7 Chang WH,Kortan P,Haber GB.Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage.Gastrointest Endosc 1998;47:354-362.
8 De Palma GD,Galloro G,Siciliano S,Iovino P,Catanzano C.Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction:results of a prospective,randomized,and controlled study.Gastrointest Endosc 2001;53:547-553.
9 Vienne A,Hobeika E,Gouya H,Lapidus N,Fritsch J,Choury AD,et al.Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures:the role of liver volume assessment.Gastrointest Endosc 2010;72:728-735.
10 Dowsett JF,Vaira D,Hatfield AR,Cairns SR,Polydorou A,Frost R,et al.Endoscopic biliary therapy using the combined percutaneous and endoscopic technique.Gastroenterology 1989;96:1180-1186.
11 Hintze RE,Abou-Rebyeh H,Adler A,Veltzke-Schlieker W,Felix R,Wiedenmann B.Magnetic resonance cholangiopancreatographyguided unilateral endoscopic stent placement for Klatskin tumors.Gastrointest Endosc 2001;53:40-46.
12 Bismuth H,Castaing D,Traynor O.Resection or palliation:priority of surgery in the treatment of hilar cancer.World J Surg 1988;12:39-47.
13 Black K,Hanna SS,Langer B,Jirsch DW,Rider WD.Management of carcinoma of the extrahepatic bile ducts.Can J Surg 1978;21:542-545.
14 Bismuth H,Nakache R,Diamond T.Management strategies in resection for hilar cholangiocarcinoma.Ann Surg 1992;215:31-38.
15 Blumgart LH,Hadjis NS,Benjamin IS,Beazley R.Surgical approaches to cholangiocarcinoma at con fluence of hepatic ducts.Lancet 1984;1:66-70.
16 Alexander F,Rossi RL,O'Bryan M,Khettry U,Braasch JW,Watkins E Jr.Biliary carcinoma.A review of 109 cases.Am J Surg 1984;147:503-509.
17 Guthrie CM,Banting SW,Garden OJ,Carter DC.Segment III cholangiojejunostomy for palliation of malignant hilar obstruction.Br J Surg 1994;81:1639-1641.
18 Larghi A,Tringali A,Lecca PG,Giordano M,Costamagna G.Management of hilar biliary strictures.Am J Gastroenterol 2008;103:458-473.
19 Polydorou AA,Chisholm EM,Romanos AA,Dowsett JF,Cotton PB,Hatfield AR,et al.A comparison of right versus left hepatic duct endoprosthesis insertion in malignant hilar biliary obstruction.Endoscopy 1989;21:266-271.
20 Vogl TJ,Schwarz WO,Heller M,Herzog C,Zangos S,Hintze RE,et al.Staging of Klatskin tumours (hilar cholangiocarcinomas):comparison of MR cholangiography,MR imaging,and endoscopic retrograde cholangiography.Eur Radiol 2006;16:2317-2325.
21 Zidi SH,Prat F,Le Guen O,Rondeau Y,Pelletier G.Performance characteristics of magnetic resonance cholangiography in the staging of malignant hilar strictures.Gut 2000;46:103-106.
22 Hänninen EL,Pech M,Jonas S,Ricke J,Thelen A,Langrehr J,et al.Magnetic resonance imaging including magnetic resonance cholangiopancreatography for tumor localization and therapy planning in malignant hilar obstructions.Acta Radiol 2005;46:462-470.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Double inferior vena cava does not complicate para-aortic nodal dissection for the treatment of pancreatic carcinoma
- Cerebral protective effect of nicorandil premedication on patients undergoing liver transplantation
- Steroid elimination within 24 hours after orthotopic liver transplantation:effectiveness and tolerability
- Association of polymorphisms in non-classic MHC genes with susceptibility to autoimmune hepatitis
- Correlation of the occurrence of YMDD mutations with HBV genotypes,HBV-DNA levels,and HBeAg status in Chinese patients with chronic hepatitis B during lamivudine treatment
- Efficacy and factors in fluencing treatment with peginterferon alpha-2a and ribavirin in elderly patients with chronic hepatitis C