胰腺结核九例的MDCT特征和误诊分析
2011-11-21梁宗辉窦娅芳唐颖汤伟军冯晓源
梁宗辉 窦娅芳 唐颖 汤伟军 冯晓源
·论著·
胰腺结核九例的MDCT特征和误诊分析
梁宗辉 窦娅芳 唐颖 汤伟军 冯晓源
目的分析胰腺结核(pancreatic tuberculoses,PT)的多层螺旋CT(MDCT)征象,以期提高对该病的认识和诊断正确率。方法收集2003年至2009年行MDCT检查并最终确诊为PT的9例患者,其中2例行MDCT血管成像。分析PT的MDCT特征性表现,并与手术及病理结果进行比较。结果MDCT诊断为胰腺癌1例、囊腺癌1例、囊腺瘤2例、假性囊肿1例、胰腺癌伴后腹膜淋巴结转移2例、淋巴瘤2例。通过病理证实,9例均为PT,误诊率达100%。PT常表现为胰头肿块,亦可累及体尾部或整个胰腺。MDCT呈现等或略低密度的囊实性肿块,偶见钙化,增强后轻度至中度环形强化。通常不伴有胰管扩张,但常伴有后腹膜或邻近淋巴结肿大,且肿大淋巴结亦呈环形强化。有时伴有腹部其他脏器结核。结论环形强化的肿块不伴有胰管扩张,同时伴有环形强化的肿大淋巴结为PT特征性的MDCT表现。
胰腺; 结核; 体层摄影术,螺旋计算机; 诊断
胰腺结核(pancreatic tuberculoses, PT)一直被认为是一种罕见病,尚没有确切的发病率统计,但却呈逐年增高的趋势,即使是在无免疫缺陷的人群之中[1]。PT常常被误诊为胰腺肿瘤,因此认识其影像学表现并给出正确诊断,有助于减少不必要的手术、放疗或化疗等创伤性治疗。本研究旨在探讨胰腺结核的多层螺旋CT(MDCT)特征,并分析误诊原因,以期提高对该病的认识和诊断水平。
材料和方法
收集我院2003年至2009年间经手术或活检病理证实的PT 9例。采用GE High Speed CT或西门子SOMATOM Sensation 64-C 螺旋CT扫描机行横断面扫描,层厚和层距均为5 mm;增强时使用碘海醇(Omnipaque)100 ml静脉注射。其中2例行MDCT血管成像,包括动脉成像(CTA)和静脉成像(CTV)。分析所有病例的CT表现,并与手术和病理结果进行对照研究,同时分析MDCT误诊原因。
结 果
9例患者中男性2例,女性7例,年龄21~73岁,平均54岁。主要症状是腹痛(4例)、消瘦(3例)和疲劳, 1例伴有轻度黄疸,1例呈现急性感染症状(高热、寒战),4例为体检发现。结核常见的症状如低热、盗汗等不明显。病程1个月~1年。MDCT均未诊断为PT,误诊率达100%。其中误诊为胰腺癌1例、囊腺癌1例、囊腺瘤2例、假性囊肿1例,该5例均经手术切除和病理证实;2例误诊为胰腺癌伴后腹膜淋巴结转移而行化疗和介入治疗,最后通过手术活检证实;2例误诊为淋巴瘤,经穿刺活检证实。
PT位于胰头颈部3例,位于肝门累及胰头2例。MDCT平扫表现为胰头或肝门区实质性或囊实性占位,等或略低密度,均匀或不均匀,形态不规则,大小3.5~8 cm,与正常胰腺分界清晰,不伴有远端胰管的扩张;增强后动脉期呈现边缘轻度不均匀或环形强化,静脉期环形强化更明显(图1),但其强化程度低于正常胰腺。PT位于胰腺体尾部3例,MDCT表现与位于头颈部者类似。PT累及全胰腺1例,表现为多发小囊样灶(图2a)。4例伴有肠系膜根部和(或)后腹膜淋巴结肿大,肿大的淋巴结融合成团块状,包绕肠系膜血管或者腹主动脉,增强后轻度环形强化,具有一定的特征性(图2b)。1例同时见肝脏内多发低强化结节灶(图2c)。2例可见病灶内小点片样钙化(图2d)。行血管成像的2例患者,不管是动脉还是静脉均见受压征象,而未被侵犯(图3)。
5例手术者术中见病灶与胰腺分界清晰,其内为干酪样坏死;2例手术活检者见淋巴结中央干酪样坏死,嗜酸染色证实为结核杆菌;2例穿刺活检者亦发现干酪样坏死和结核杆菌。

CT平扫(a)示胰头肿大,呈等、略低密度,增强后动脉期(b)轻度不均匀环形强化,静脉期(c)强化更明显
图1位于胰头颈部PT的MDCT征象
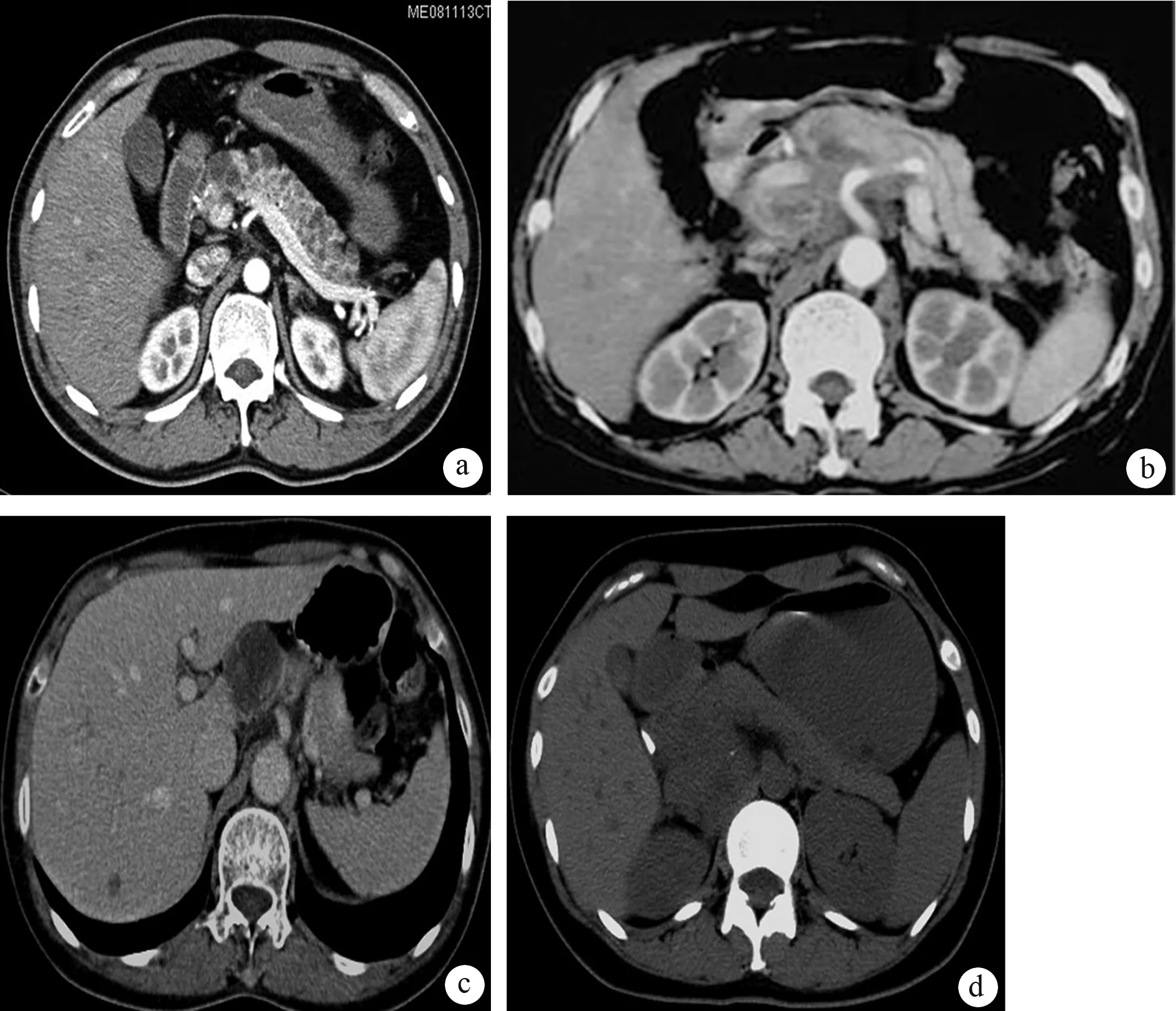
a:误诊为胰腺囊腺瘤,全胰腺内可见多发小囊状低密度灶;b:误诊为淋巴瘤,后腹膜肿大淋巴结呈环形强化;c:误诊为胰头囊腺瘤,肝脏内见低强化结节灶;d:误诊为胰腺瘤,病灶内可见钙化
图2PT患者的MDCT特征

CTA图像最大密度投影(MIP)重建显示病灶包绕血管(a),压迫门静脉(b);容积重建(VR)显示门静脉受压而非侵犯(c)
图3PT的MDCT血管成像征象
讨 论
PT是一种罕见的胰腺疾病,Franco-Paredes等[2]回顾1980年至2002年的文献,仅报道了50例PT,Nagar等[3]2009年回顾文献,报道不足100例,Xia等[4]2003年回顾中文文献,共报道了58例。PT病理与其他部位的结核一样,主要表现为结核性肉芽肿和干酪样坏死。通常伴有腹腔内其他部位的结核灶,如肝脏、脾脏、胆囊、肠系膜或者后腹膜淋巴结以及腹膜等部位。局灶性的结核球有时类似占位性病变,常常被误诊为胰腺癌而手术。
PT主要见于HIV感染或器官移植后使用免疫抑制剂者[5]。近年来,发生于免疫正常者的病例逐渐增多,本组均为免疫功能正常者。PT发病以年轻人多见,男、女的发病率相仿[6],本组以成年女性居多,与Xia等[4]的报道一致。PT的临床症状多种多样,缺乏特征性[1-2,5-8]。本组患者主要症状为腹痛和消瘦,4例体检发现,MDCT检查后均误诊。
PT的CT平扫示胰腺低密度或囊样肿块,主要位于胰头[7]。有时可以看到扩张的主胰管、脾静脉栓塞、胆总管梗阻所致的胆管扩张等征象,而胰腺弥漫肿胀类似急性胰腺炎的表现则非常少见。CT增强扫描,病灶呈不均匀强化或环形强化。钙化较少见,在疾病晚期可见钙化。有时PT表现为囊肿而被误诊。此外尚可发现肝脏、脾脏等病灶以及后腹膜淋巴结肿大[6]。肝脏结核通常表现为低密度病灶伴钙化,肿大的淋巴结呈现中央低密度伴有环形强化。
PT常常被误诊为胰腺癌,特别是在出现梗阻性黄疸、局灶性肿块且伴有胆总管扩张时[1,4,8-11]。PT以年轻人多见,且肿瘤标志物,如CA19-9、CEA等通常没有增高;而胰腺癌以老年人多见,且伴有肿瘤指标的升高。影像学检查中,MRI可以提供较多的信息,如病灶的延迟环形强化,不侵犯血管,且胰、胆管扩张程度与肿块不成比例等有助于PT的诊断。
PT常伴有广泛后腹膜、肝门淋巴结肿大时需要与淋巴瘤相鉴别。淋巴瘤好发于50岁左右的中年人,其病灶和肿大淋巴结均为实质性,密度均匀,边缘轻度强化,有时出现胰管狭窄或轻度扩张,肿大淋巴结具有融合的趋势且包绕血管[12-13];而PT多见于30岁左右的青年人,其病灶和肿大淋巴结都呈典型环形强化,不包绕血管。
EUS或CT引导下的穿刺活检或者是通过ERCP胆管冲刷可获得正确诊断[14],试验性的抗结核治疗也可以作为一种手段。
总之,胰腺结核具有局灶性肿块或囊肿伴有环形强化为特征的MDCT表现,胰胆管通常正常,周围肿大淋巴结也以环形强化为特征,MDCT血管成像有助于判断病灶或淋巴结与血管的关系。
[1] Pombo F,Díaz Candamio MJ,Rodriguez E,et al.Pancreatic tuberculosis:CT findings.Abdom Imaging,1998,23:394-397.
[2] Franco-Paredes C,Leonard M,Jurado R,et al.Tuberculosis of the pancreas: Report of two cases and review of the literature.Am J Med Sci,2002,323:54-58.
[3] Nagar AM,Raut AA,Morani AC,et al.Pancreatic tuberculosis: a clinical and imaging review of 32 cases.J Comput Assist Tomogr,2009,33:136-141.
[4] Xia F,Poon RT,Wang SG,et al.Tuberculosis of pancreas and peripancreatic lymph nodes in immunocompetent patients:experience from China.World J Gastroenterol,2003,9:1361-1364.
[5] Sanabe N,Ikematsu Y,Nishiwaki Y,et al.Pancreatic tuberculosis. J Hepatobiliary Pancreat Surg,2002,9:515-518.
[6] Foo FJ,Verbeke CS,Guthrie JA,et al.Pancreatic and peripancreatic tuberculosis mimicking malignancy.JOP,2007,8:201-205.
[7] David AW,Eapen A,Vyas FL,et al.The pancreas and tuberculosis: a diagnostic challenge.Indian J Gastroenterol,2008,27:29-30.
[8] Khalil B,Adeyeri A,Ramcharan A.Pancreatic tuberculosis mimicking malignancy.J Am Coll Surg,2009,208:476-477.
[9] Eyal AS,Karusseit VO.Tuberculosis of the pancreas mimicking carcinoma.Int J Infect Dis,2008,12:108-110.
[10] Weiss E,Klein W,Yeo C.Peripancreatic tuberculosis mimicking pancreatic neoplasia.J Gastrointest Surg,2005,9:254-262.
[11] Tan KK,Chen K,Liau KH,et al.Pancreatic tuberculosis mimicking pancreatic carcinoma: series of three cases. Eur J Gastroenterol Hepatol,2009,21:1317-1319.
[12] Lin H,Li SD,Hu XG,et al.Primary pancreatic lymphoma: report of six cases.World J Gastroenterol,2006,12:5064-5067.
[13] Mortenson MM,Katz MH,Tamm EP,et al.Current diagnosis and management of unusual pancreatic tumors.Am J Surg,2008,196: 100-113.
[14] Sachdev A,D′Cruz S,Chauhan S,et al.Pancreaticobiliary tuberculosis diagnosed by endoscopic brushings.JOP,2006,7:665-669.
2010-05-10)
(本文编辑:屠振兴)
Pancreatictuberculosis:MDCTfeaturesanddifferentialdiagnosis
LIANGZong-hui,DOUYa-fang,TANGYing,TANGWei-jun,FENGXiao-yuan.
DepartmentofRadiology,HuashanHospital,FudanUniversity,Shanghai200040,China
LIANGZong-hui,Email:liangzh@vip.163.com
ObjectiveTo study the multi-detector spiral CT (MDCT) features of pancreatic tuberculosis to improve the awareness and correct diagnosis.MethodsImaging features of MDCT were retrospectively reviewed on 9 cases with pancreatic tuberculosis that were diagnosed from 2003 to 2009, among them two patients underwent MDCT angiography, the features were compared with those of operative and pathological findings.ResultsOne case of pancreatic cancer, 2 cases of cystadenocarcinoma and 1 case of pseudocyst, 2 cases of pancreatic cancer with retroperitoneal lymph node metastasis, 2 cases of lymphoma were diagnosed by MDCT, and all the lesions were diagnosed as pancreatic tuberculosis pathologically, and the misdiagnosis rate was 100%. Pancreatic tuberculosis often presented as pancreatic head mass, sometimes pancreatic body and tail were involved. MDCT showed isopycnic or low density solid-cyst mass, occasionally calcification was present, with slightly or moderate ring-like enhancement after contrast injection. There was no enlargement of the pancreatic duct. The retroperitoneal and adjacent lymph nodes were always enlarged with ring-like enhancement. Sometimes there was evidence of tuberculosis of other abdominal organs.ConclusionsRing-like enhanced lesions with ring-like enhanced lymph nodes without enlargement of pancreatic duct are characteristic MDCT features of pancreatic tuberculosis.
Pancreas; Tuberculosis; Tomography,spiral computed; Diagnosis
10.3760/cma.j.issn.1674-1935.2011.02.011
200040 上海,复旦大学附属华山医院放射科(梁宗辉、窦娅芳、唐颖、汤伟军、冯晓源);上海市静安区中心医院放射科(梁宗辉)
梁宗辉,Email:liangzh@vip.163.com
