Monday blues of deceased-donor liver transplantation
2011-07-07SeeChingChanWingChiuDaiChungMauLoBannyLamYuenManKwanWaiYiHoandSheungTatFan
See Ching Chan, Wing Chiu Dai, Chung Mau Lo, Banny Lam, Yuen Man Kwan, Wai Yi Ho and Sheung Tat Fan
Hong Kong, China
Original Article / Transplantation
Monday blues of deceased-donor liver transplantation
See Ching Chan, Wing Chiu Dai, Chung Mau Lo, Banny Lam, Yuen Man Kwan, Wai Yi Ho and Sheung Tat Fan
Hong Kong, China
BACKGROUND:There is a constant and global shortage of deceased-donor organs for transplantation. Ways to identify areas for securing potential deceased-donor organs may improve the supply and hence benefit more patients in need of transplantation.
METHODS:We looked into the disparity of the number of deceased-donor liver transplantation (DDLT) performed at our hospital on different days of the weeks from January 2000 to the end of December 2009 (237 DDLTs). The number of DDLT performed on each day was compared with the other days of the week.
RESULTS:It was apparent that there were fewer DDLTs on Mondays, as shown by the numbers of DDLT performed on different days of the week in an ascending order: Monday 18 (7.6%), Sunday 30 (12.7%), Thursday 34 (14.3%), Friday 36 (15.2%), Wednesday 38 (16.0%), Tuesday 40 (16.9%), and Saturday 41 (17.3%). The difference reached statistical significance when Monday was compared with Tuesday (P=0.019), Wednesday (P=0.010), Friday (P=0.021), and Saturday (P=0.007). It was twice as unlikely a DDLT would be performed on Monday as compared with other days. Such a trend did not change even with an increase in the number of deceased-donor liver grafts in the last year. As consent to donation was obtained from the donor family the day before DDLT, fewer consents were thus obtained on Sundays.
CONCLUSION:These findings suggested that deceased-donor organ donation activities were less active on Sundays and could be improved. This further raises the concern of possible wastage of potential cases of organ donation.
(Hepatobiliary Pancreat Dis Int 2011; 10: 26-29)
deceased-donor; liver transplantation; graft shortage; organ donation
Introduction
Deceased-donor liver transplantation (DDLT), the ideal treatment for end-stage liver disease and small unresectable hepatocellular carcinoma, is unfortunately hampered by the shortage of deceaseddonor liver grafts. The current practice of DDLT has achieved a satisfactory 5-year survival rate of over 80%[1]and 70%[2]respectively for the aforementioned two categories of transplant recipients. The constant discussion about allocation of a limited number of liver grafts for transplantation to a much larger number of transplant candidates listed is a testimony to the refractory shortage of organs.[3,4]This shortage is the only reason why living-donor liver transplantation (LDLT) is taking up the upfront role in many regions of Asia where the shortage is devastating.[5,6]Unless DDLT is not feasible, LDLT should not be the prime treatment, given the inevitable and undeniable donor morbidity at as high as 67%[7]and donor mortality 0.5%.[8]
Organ donation, which we refer to as donation from a deceased-donor, does not just happen. It can only come into existence through deliberations of many parties, and can only be accomplished through motivation, education, training, and adequate funding. We in our city witnessed an encouraging increase in organ donation in the year 2009. Nonetheless, identifying potential areas for improvement should not stop. Aiming at increasing the number of organs available for DDLT, this studyinvestigated whether organ donation is less frequent on any particular day of the week in relation to statutory holidays.
Methods
We reviewed our centre's liver transplant data from January 2000 to December 2009. In July 2003, the only two liver transplant waiting lists in our city were unified; and since late 2003, our centre has been the only designated centre in the city for performing liver transplantation. The data, collected prospectively by liver transplant coordinators and entered into a single liver transplant database, were evaluated retrospectively. Only DDLTs were included. The day on which a DDLT operation started was coded as the day of the operation. Split-liver transplantation using grafts from the same liver was counted as two cases. The second operation of sequential liver transplantation was considered as LDLT and was excluded. All data were analyzed with SPSS version 16.0 for Windows (SPSS, Chicago, IL, USA). A P value of <0.05 was considered statistically significant.
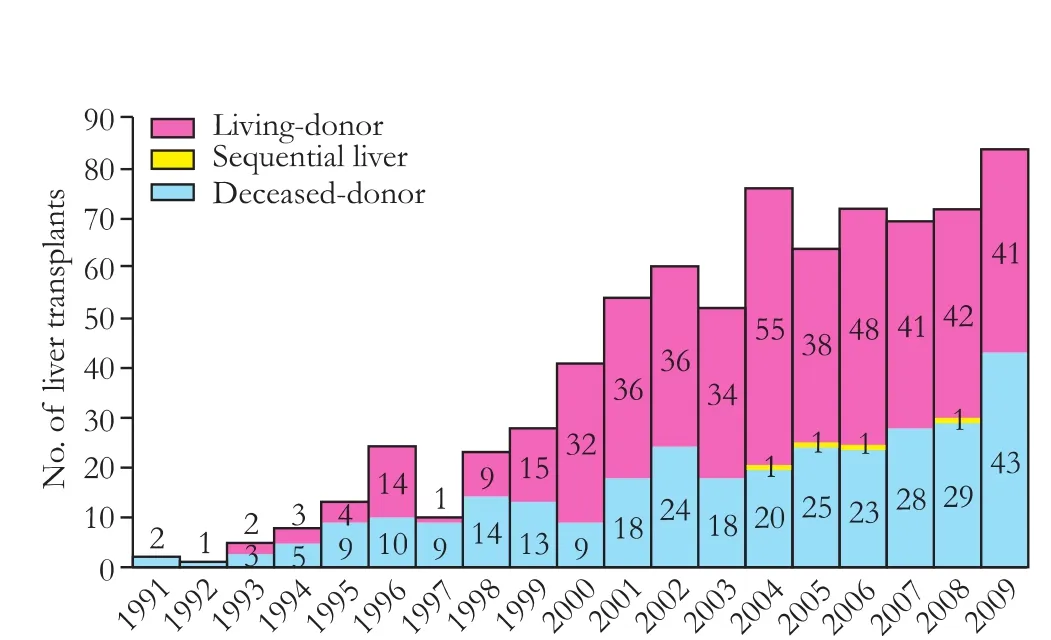
Fig. 1. Liver transplants at the authors' hospital from 1991 to 2009.
Results
The past liver transplant caseload (1991-2009) in our centre is depicted in Fig. 1. About two thirds of the cases were LDLTs and one third DDLTs. From January 2000 to December 2009, we performed 237 DDLTs with grafts from 227 donors. Ten livers were split and transplanted to 20 recipients. The causes of brain death of the donors are shown in Table. In 2009, 43 DDLTs were performed, outnumbering DDLTs performed in each of the previous years. When the number of DDLTs performed on each day of the week in the 10 years was plotted in Fig. 2, it became apparent that there were fewer cases on Monday. The numbers of DDLTs performed on different days of the week were (in an ascending order): Monday 18 (7.6%), Sunday 30 (12.7%), Thursday 34 (14.3%), Friday 36(15.2%), Wednesday 38 (16.0%), Tuesday 40 (16.9%), and Saturday 41 (17.3%). Monday had about half the number of DDLTs compared with any day of the rest of the week. The difference was statistically significant when Monday was compared with Tuesday (P=0.019), Wednesday (P=0.010), Friday (P=0.021), and Saturday (P=0.007) (Fig. 2). Such a trend did not change even with an increase in the number of deceased-donor liver grafts in the last year. When the numbers of cases on different days of the week were plotted year by year, it was also found that DDLT was performed on Monday only once a year in 4 years. In the year 2003, no DDLT was performed on Monday at all. It is worth noting that in 2008, however, 5 DDLTs were performed on Monday (Fig. 3).
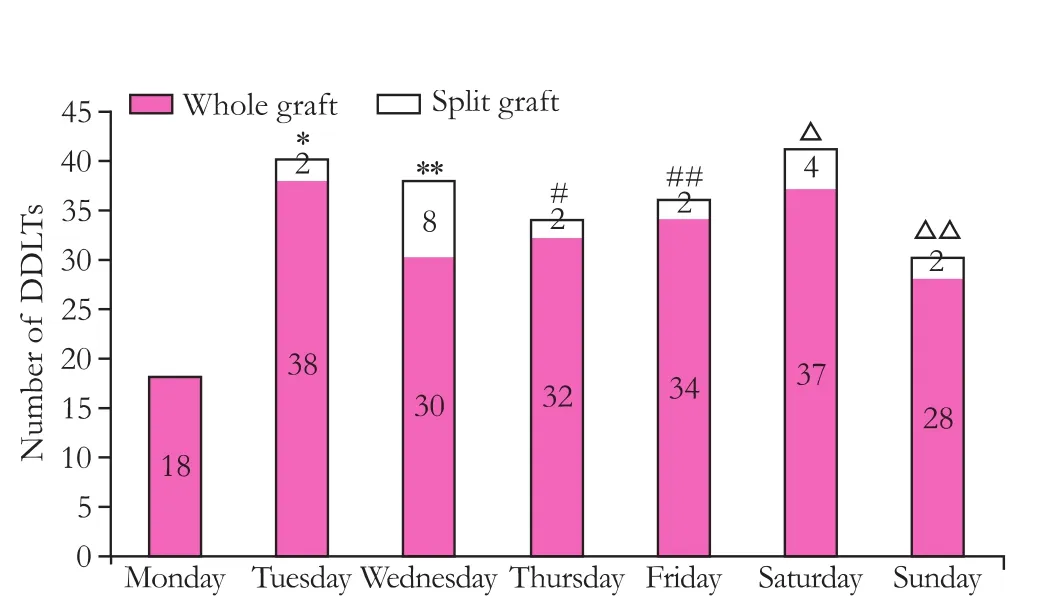
Fig. 2. Total number of DDLTs on each day of the week from 2000 to 2009 at the authors' hospital. *: P=0.019, Monday vs. Tuesday; **: P=0.010, Monday vs. Wednesday; #: P=0.050, Monday vs. Thursday; ##: P=0.021, Monday vs. Friday; △: P=0.007, Monday vs. Saturday; △△: P=0.066, Monday vs. Sunday.
Fig. 3. Yearly numbers of DDLTs on each day of the week from 2000 to 2009 at the authors' hospital.
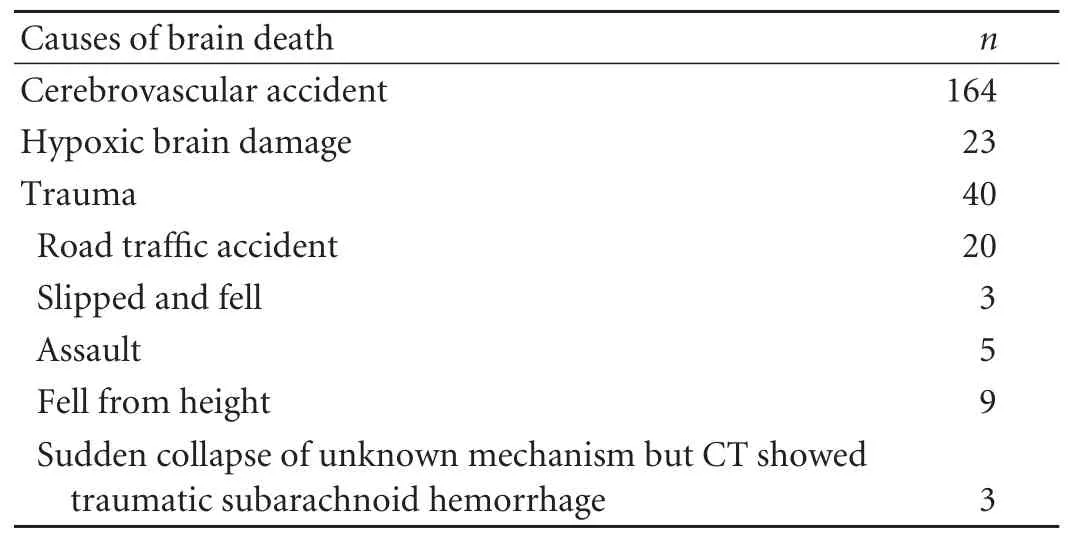
Table. Causes of brain death of the 227 deceased donors
Discussion
Fewer DDLTs were performed on Monday. As DDLT is usually performed on the day after consent to donation has been obtained, this finding suggests that deceased-donor organ donation activities were less active on Sunday. A rebound in the number of DDLTs on Tuesday as compared with Wednesday (P=0.908), Thursday (P=0.375) and Friday (P=0.536) was not observed. This further raises the concern over possible wastage of potential donations.
Data on the consent rate of potential donor families was not included in this analysis. This is an area one can look into as it may also reflect the difference in the success rates on different days of the week. Say, in the analysis of this series, there could have been the same number of potential donor families being approached on each day of the week, but the consent rate was, however, lower on Sunday. Unlike other years, in 2008, 5 DDLTs were performed on Monday. This coincided with the recruitment of two full-time organ transplant coordinators. It will take much longer to obtain a clearer pattern of this observation. Many other factors are relevant in the process of organ donation, including the suitability of a liver as a graft in terms of liver functionwhether there is fatty change, hepatitis, etc. There is, however, no reason that these should vary across the week.
As the majority of brain-dead deaths are a result of intracerebral accidents, there is a question of a higher mortality or non-salvage rate at the weekend as shown in a study.[9]If this was true, then the number of donations should be the highest on Saturday and Sunday and DDLT more frequent on the following days, i.e. Sunday and Monday. Published data on this are conflicting. While there were series and observation of "the weekend effect" of higher mortality, such "effect", if any, was immaterial in a well-staffed comprehensive stroke centre.[10]There also comes a question of an increase in the incidence of stroke during weekdays. In a large series from Japan, the incidence of admission for stroke did increase after weekend and stayed high over the weekdays.[11]This could explain our situation of fewer DDLTs on Monday but not other days. However, according to another study, the fatality rate of stroke was higher in patients admitted at the weekend.[12]While there was evidence of a lower survival rate of inpatient cardiac arrest during night time and the weekend,[13]the fatality rate of motor-vehicle accidents did not vary in a highly developed trauma and acute care centre.[14]This suggests that improved clinical services, incentives and resources could abolish the compromised outcome of such emergencies. The irregularity of organ donation throughout the week should also be eliminated by such means.
To truly assess the deceased-donor liver procurement rate, comparison between data on the liver and data on the kidney as well as other organs is needed; a more comprehensive database would help in future planning of organ donation promotions. Since failure in securing transplantable deceased-donor organs may occur early in the procurement process, for example, when identifying suitable donors or obtaining consent from the family, programmes like Donor Action[15]which can identify the inadequacies for improvement are much desirable.
Promotion of organ donation is a continuous process. As every organ for transplantation is life-saving, every organ counts. Our efforts to look into every potential source should be constant regardless of the day of the week. The very purpose of this study is to alert the organ transplant community of this area where there is potential for an increase in the number of liver grafts for transplantation.
Funding:None.
Ethical approval:Not needed.
Contributors:CSC designed the study, did the statistics, analyzed the data, and drafted the article. DWC analyzed the data. LB, KYM and HWY collected the data. LCM and FST were responsible for critical revision and approval of the article.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Roberts MS, Angus DC, Bryce CL, Valenta Z, Weissfeld L. Survival after liver transplantation in the United States: a disease-specific analysis of the UNOS database. Liver Transpl 2004;10:886-897.
2 Duffy JP, Vardanian A, Benjamin E, Watson M, Farmer DG, Ghobrial RM, et al. Liver transplantation criteria for hepatocellular carcinoma should be expanded: a 22-year experience with 467 patients at UCLA. Ann Surg 2007;246: 502-511.
3 Freeman RB, Jamieson N, Schaubel DE, Porte RJ, Villamil FG. Who should get a liver graft? J Hepatol 2009;50:664-673.
4 Schaubel DE, Guidinger MK, Biggins SW, Kalbfleisch JD, Pomfret EA, Sharma P, et al. Survival benefit-based deceaseddonor liver allocation. Am J Transplant 2009;9:970-981.
5 Morioka D, Egawa H, Kasahara M, Ito T, Haga H, Takada Y, et al. Outcomes of adult-to-adult living donor liver transplantation: a single institution's experience with 335 consecutive cases. Ann Surg 2007;245:315-325.
6 Chan SC, Fan ST, Lo CM, Liu CL, Wei WI, Chik BH, et al. A decade of right liver adult-to-adult living donor liver transplantation: the recipient mid-term outcomes. Ann Surg 2008;248:411-419.
7 Pomfret EA, Pomposelli JJ, Lewis WD, Gordon FD, Burns DL, Lally A, et al. Live donor adult liver transplantation using right lobe grafts: donor evaluation and surgical outcome. Arch Surg 2001;136:425-433.
8 Barr ML, Belghiti J, Villamil FG, Pomfret EA, Sutherland DS, Gruessner RW, et al. A report of the Vancouver Forum on the care of the live organ donor: lung, liver, pancreas, and intestine data and medical guidelines. Transplantation 2006; 81:1373-1385.
9 Saposnik G, Baibergenova A, Bayer N, Hachinski V. Weekends: a dangerous time for having a stroke? Stroke 2007; 38:1211-1215.
10 Albright KC, Raman R, Ernstrom K, Hallevi H, Martin-Schild S, Meyer BC, et al. Can comprehensive stroke centers erase the 'weekend effect'? Cerebrovasc Dis 2009;27:107-113.
11 Turin TC, Kita Y, Murakami Y, Rumana N, Sugihara H, Morita Y, et al. Increase of stroke incidence after weekend regardless of traditional risk factors: Takashima Stroke Registry, Japan; 1988-2003. Cerebrovasc Dis 2007;24:328-337.
12 Turin TC, Kita Y, Rumana N, Ichikawa M, Sugihara H, Morita Y, et al. Case fatality of stroke and day of the week: is the weekend effect an artifact? Takashima stroke registry, Japan (1988-2003). Cerebrovasc Dis 2008;26:606-611.
13 Peberdy MA, Ornato JP, Larkin GL, Braithwaite RS, Kashner TM, Carey SM, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA 2008;299:785-792.
14 Laupland KB, Ball CG, Kirkpatrick AW. Hospital mortality among major trauma victims admitted on weekends and evenings: a cohort study. J Trauma Manag Outcomes 2009;3: 8.
15 Roels L, Spaight C, Smits J, Cohen B. Critical Care staffs' attitudes, confidence levels and educational needs correlate with countries' donation rates: data from the Donor Action database. Transpl Int 2010;23:842-850.
October 13, 2010
Accepted after revision December 31, 2010
Author Affiliations: Department of Surgery, Queen Mary Hospital, The University of Hong Kong, Hong Kong, China (Chan SC, Dai WC, Lo CM, Lam B, Kwan YM, Ho WY and Fan ST)
Chung Mau Lo, Professor, Department of Surgery, Queen Mary Hospital, The University of Hong Kong, 102 Pok Fu Lam Road, Hong Kong, China (Tel: 852-22554748; Fax: 852-28162765; Email: chungmlo@hkucc.hku.hk)
© 2011, Hepatobiliary Pancreat Dis Int. All rights reserved.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Laparoscopic liver resection for benign and malignant liver tumors
- Assessment of tumor vascularization with functional computed tomography perfusion imaging in patients with cirrhotic liver disease
- Expression oflamino acid transport system 1 and analysis of iodine-123-methyltyrosine tumor uptake in a pancreatic xenotransplantation model using fused high-resolution-micro-SPECT-MRI
- Hepatobiliary & Pancreatic Diseases International (HBPD INT)
- Roles of sulfonylurea receptor 1 and multidrug resistance protein 1 in modulating insulin secretion in human insulinoma
- Atypical focal nodular hyperplasia of the liver
