Undifferentiated embryonal sarcoma of the liver presenting as a hemorrhagic cystic tumor in an adult
2011-07-03HoHyunKimJungChulKimEunKyuParkYoungHoeHurYangSeokKohCholKyoonChoHyungSeokKimandHyunJongKim
Ho Hyun Kim, Jung Chul Kim, Eun Kyu Park, Young Hoe Hur, Yang Seok Koh, Chol Kyoon Cho, Hyung Seok Kim and Hyun Jong Kim
Gwangju, Korea
Undifferentiated embryonal sarcoma of the liver presenting as a hemorrhagic cystic tumor in an adult
Ho Hyun Kim, Jung Chul Kim, Eun Kyu Park, Young Hoe Hur, Yang Seok Koh, Chol Kyoon Cho, Hyung Seok Kim and Hyun Jong Kim
Gwangju, Korea
BACKGROUND:Undifferentiated embryonal sarcoma (UES) of the liver is a rare, highly malignant neoplasm with a poor prognosis occurring almost exclusively in late childhood (6-10 years of age). Only a few cases have been reported in adults, accounting for less than 1% of all primary liver neoplasms.
METHODS:A 47-year-old woman presented with a palpable mass in the left upper abdomen. Magnetic resonance imaging revealed a 12×10 cm cystic mass with hemorrhage in the left lateral segment of the liver. The initial impression was a hemorrhagic cystic tumor of the liver. The patient underwent a left lateral sectionectomy of the liver. Histopathology and immunohistochemistry helped make a diagnosis of UES.
RESULTS:The patient recovered uneventfully and received systemic chemotherapy. Radiologic examination for follow-up revealed a metastatic lesion in the lumbar spine (L5). She was subjected to radiotherapy at the lumbar spine. She survived 48 months.
CONCLUSION:Although hepatic cyst as UES of the liver is difficult to diagnose because of its rarity in adults and lack of specific findings, it should be considered in a differential diagnosis.
(Hepatobiliary Pancreat Dis Int 2011; 10: 657-660)
embryonal sarcoma; liver neoplasms; cyst; adult
Introduction
Undifferentiated embryonal sarcoma (UES) of the liver was reported as a clinicopathological entity in 1978.[1]Before this, its nomenclature included mesenchymoma, primary sarcoma of the liver, fibromyxosarcoma and malignant mesenchymoma.[2]UES of the liver has a predilection for the pediatric population between 6 and 10 years of age. Its incidence in adults over the age of 40 years is exceptionally low.[3]To our knowledge, fewer than 50 cases of UES of the liver in adults have been reported within 40 years up to 2009.[4]
We treated a 47-year-old woman with UES of the liver who had been admitted to our hospital for a palpable mass in the left upper abdominal quadrant. The diagnosis of UES was confirmed by histopathological and immunohistochemical findings.
Case report
A 47-year-old woman came to our hospital for abdominal distension for 20 days. Her medical history was noncontributory. Clinical examination revealed a huge palpable mass in the left upper abdominal quadrant. Blood tests showed elevated levels of amylase and lipase (amylase 141 IU/L, normal 20-100 U/L; lipase 129 U/L, normal 7-60 U/L). Liver function was within normal. The level of carbohydrate antigen 125 (CA125) was elevated to 64.93 U/mL (normal 0-30 U/mL). The serum levels of carcinoembryonic antigen (CEA), carbohydrate antigen 19-9 (CA19-9) and alpha-fetoprotein (AFP) were within normal limits. Hepatitis viral markers HBsAg and anti-HCV were negative.
Abdominal computed tomography (CT) revealed a 12-cm well-demarcated, low attenuated mass with hyperdense septations in the left lobe of the liver (Fig. 1). There was no calcification in the mass. Magnetic resonance imaging (MRI) of the liver demonstrated a 12×10 cm exophytic multiseptated cystic mass in the left lateral segment of the liver (Fig. 2). The septa and wall of the mass were strongly enhanced after injection of intravenous contrast medium. No regional lymphadenopathy, ascites or metastasis was demonstrated on MRI. A hemorrhagic cystic tumor such as biliary cystadenoma was diagnosed initially. A left lateral sectionectomy of the liver was performed. Macroscopic examination revealed an exophyting multiseptate cystic mass (13×12×8 cm) in the left lateral lobe of the liver, accompanied by a hard capsule and internal hematoma (Fig. 3). Histopathologically, the tumor was composed of spindle cells with occasional bizarre giant nuclei and no differentiation (Fig. 4). The tumor cells were embedded in the myxoid stroma (Fig. 4A). An immunohistochemical examination revealed positive staining for vimentin (Fig. 4B), HAS (Fig. 4C), CK7, CD34, CK, actin, desmin, PAS (Fig. 4D) and D-PAS, but no staining for CK20, S-100, D2-40, HMB45, and c-kit. A final pathological diagnosis was made of undifferentiated embryonal sarcoma of the liver. The patient recovered uneventfully and was discharged on the 18th postoperative day.
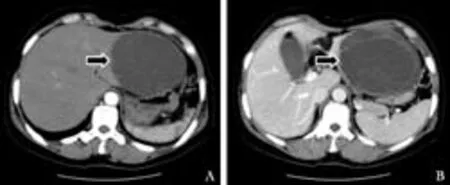
Fig. 1. Abdominal CT findings. CT showing a 12-cm welldemarcated, low attenuation mass with hyperdense septations in the left lobe of the liver. There was no calcification in the lesion.
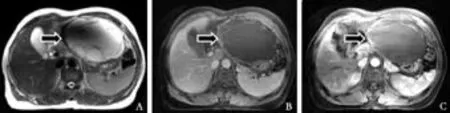
Fig. 2. Abdominal MRI findings. MRI showing a 12×10 cm exophytic cystic mass with multiseptation in the left lateral segment of the liver. The septa and wall of the mass were enhanced.
She had received chemotherapy with MAID (Mesna 2500 mg/m2, Doxorubicin 15 mg/m2; Ifosfamide 2500 mg/m2, dacarbazine 250 mg/m2) for 6 times at 3-week intervals. Two years later, positron emission tomography/ computed tomography (PET/CT) in follow-up revealed a metastatic lesion in the lumbar spine (L5). No tumor recurrence was seen in the abdominal cavity. The patient underwent radiotherapy at the lumbar spine. The patient is being subjected to routine imaging and laboratory examination twice a year.

Fig. 3. Gross findings of undifferentiated embryonal sarcoma of the liver. There was a 13×12×8 cm exophyting multiseptated cystic mass in the left lateral section of the liver, which had hard capsule and internal hematoma.
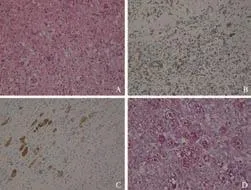
Fig. 4. Microscopic findings (HE, original magnification ×200). The tumor was composed of spindle cells with occasional bizarre giant nuclei and no differentiation. The tumor cells were embedded in myxoid stroma (A). Immunohistochemical studies revealed positive expression of vimentin (B), HAS (in hepatocytes, C) and PAS (D).
Discussion
UES of the liver was first described by Stocker and Ishak in 1978.[1]The tumor is predominantly seen in children aged between 6 and 10 years, and is an extremely rare neoplasm in adults. It is seen more frequently in the right lobe of the liver (59%) than in the left one (22%), but sometimes appears simultaneously in both lobes (20%).[5]
The cause of UES of the liver is unclear, and the histogenesis of this tumor remains undetermined. It is recognized a malignant counterpart of mesenchymal hamartoma.[6]The tumor may be derived from a multipotent precursor cell that is able to differentiate along stromal and epithelial lines.[7]Several cytogenetic abnormalities, including TP53 mutation, chromosomes 19q and 7q, have been investigated to understand the histogenesis of this tumor.[8]
Adult patients with UES of the liver often show nonspecific symptoms including epigastric mass, dull upper abdominal pain, and hepatomegaly.[9]
In contrast to primary liver carcinoma, UES of the liver is not associated with hepatitis or liver cirrhosis, and no disturbance of liver function. Laboratory studies are non-specific, and tumor markers including AFP, CEA, and CA19-9 are often not informative.[2,10]
CT findings show a well-circumscribed huge cystic or solid mass with a few internal septations and a dense peripheral rim corresponding to the fibrous pseudocapsule, which is hypodense in the pre-contrast phase and strongly enhanced in the contrast phase.[6,11]MRI usually demonstrate that large portions of the mass are hypointense on the T1-weighted images and have a high signal intensity on T2-weighted images. The areas of a high signal intensity on T1-weighted images and a low signal intensity on T2-weighted images may be seen in some cases due to intratumoral hemorrhage.[3,6,8]Before surgery it is difficult to diagnose the mass pathologically because there are no specific symptoms, tumor markers, or radiologic results.
Occasionally, it is difficult to differentiate UES from other cystic tumors such as biliary cystadenoma because of similar CT/MRI findings. In biliary cystadenoma, CT demonstrates a hypodense, well-defined mass with septations. The cyst often appears hypointense on the T1-weighted images and hyperintense on the T2-weighted images, similar to other fluid-filled cystic lesions. Furthermore, a variety of T1- and T2-signal characteristics are dependent on the fluid content of the cyst. In our patient, CT revealed a well-demarcated, low attenuated mass with hyperdense septations in the left lobe of the liver. MRI demonstrated a multiseptate cystic mass in the left lateral segment of the liver. UES is an extremely rare neoplasm in adults. Therefore, the initial radiological diagnosis was made of a hemorrhagic cystic tumor such as biliary cystadenoma. However, UES of the liver was diagnosed after surgery.
Until the late 1980s, the survival rate of patients with UES of the liver was poor. Most of the patients died of tumor recurrence or metastasis within two years after operation.[1]The major impediments in achieving long-term, disease-free intervals are local recurrence in the upper abdomen and distant metastases.[12]Metastasis to the lung, pleura and peritoneum are common. However, the survival rate of the patients was improved considerably in the early 1990s. It is likely that refinement of surgical techniques has contributed to this improvement. Reports have described that combination of surgical resection and adjuvant chemotherapy (with cisplatin, adriamycin, cyclophosphamide) and/or radiotherapy may offer a reasonable prognosis.[13,14]Lenze et al[15]reported that the survival of patients who underwent a tumor resection followed by adjuvant chemotherapy (n=17) was significantly better than that of the patients who underwent operation alone (n=14). Our patient received chemotherapy 6 times and radiotherapy. She has survived during a follow-up of 48 months. Thus, preand/or post-operative systemic chemotherapy and/or radiotherapy may benefit patients with UES.[10]Patient age, sex, and tumor size are influential to the survival of UES patients.[16]
In conclusion, hepatic cyst such as UES of the liver is difficult to diagnose for its rare occurrence in adults and lack of specific findings. A differential diagnosis should be made because early diagnosis and a curative resection of the tumor are essential for a favorable outcome.
Funding:None.
Ethical approval:Not needed.
Contributors:KHH wrote the paper. KHS evaluated immunohistochemical staining. KJC designed the research and supervised the paper. All authors contributed to the intellectual context and approved the final version. KJC is the guarantor.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Stocker JT, Ishak KG. Undifferentiated (embryonal) sarcoma of the liver: report of 31 cases. Cancer 1978;42:336-348.
2 McFadden DW, Kelley DJ, Sigmund DA, Barrett WL, Dickson B, Aron BS. Embryonal sarcoma of the liver in an adult treated with preoperative chemotherapy, radiation therapy, and hepatic lobectomy. Cancer 1992;69:39-44.
3 Psatha EA, Semelka RC, Fordham L, Firat Z, Woosley JT. Undifferentiated (embryonal) sarcoma of the liver (USL): MRI findings including dynamic gadolinium enhancement.Magn Reson Imaging 2004;22:897-900.
4 Kaur J, Dey P, Das A. Fine needle aspiration cytology of undifferentiated (embryonal) sarcoma of liver in an adult male. Diagn Cytopathol 2010;38:547-548.
5 Pachera S, Nishio H, Takahashi Y, Yokoyama Y, Oda K, Ebata T, et al. Undifferentiated embryonal sarcoma of the liver: case report and literature survey. J Hepatobiliary Pancreat Surg 2008;15:536-544.
6 Joshi SW, Merchant NH, Jambhekar NA. Primary multilocular cystic undifferentiated (embryonal) sarcoma of the liver in childhood resembling hydatid cyst of the liver. Br J Radiol 1997;70:314-316.
7 Walker NI, Horn MJ, Strong RW, Lynch SV, Cohen J, Ong TH, et al. Undifferentiated (embryonal) sarcoma of the liver. Pathologic findings and long-term survival after complete surgical resection. Cancer 1992;69:52-59.
8 Wei ZG, Tang LF, Chen ZM, Tang HF, Li MJ. Childhood undifferentiated embryonal liver sarcoma: clinical features and immunohistochemistry analysis. J Pediatr Surg 2008;43: 1912-1919.
9 Xu HF, Mao YL, Du SD, Chi TY, Lu X, Yang ZY, et al. Adult primary undifferentiated embryonal sarcoma of the liver: a case report. Chin Med J (Engl) 2010;123:250-252.
10 Dai CL, Xu F, Shu H, Xu YQ, Huang Y. Undifferentiated (embryonal) sarcoma of liver in adult: a case report. World J Gastroenterol 2005;11:926-929.
11 Moon WK, Kim WS, Kim IO, Yeon KM, Yu IK, Choi BI, et al. Undifferentiated embryonal sarcoma of the liver: US and CT findings. Pediatr Radiol 1994;24:500-503.
12 Steiner M, Bostrum B, Leonard AS, Dehner LP. Undifferentiated (embryonal) sarcoma of the liver. A clinicopathologic study of a survivor treated with combined technique therapy. Cancer 1989;64:1318-1322.
13 Kim DY, Kim KH, Jung SE, Lee SC, Park KW, Kim WK. Undifferentiated (embryonal) sarcoma of the liver: combination treatment by surgery and chemotherapy. J Pediatr Surg 2002;37:1419-1423.
14 Bisogno G, Pilz T, Perilongo G, Ferrari A, Harms D, Ninfo V, et al. Undifferentiated sarcoma of the liver in childhood: a curable disease. Cancer 2002;94:252-257.
15 Lenze F, Birkfellner T, Lenz P, Hussein K, Langer F, Kreipe H, et al. Undifferentiated embryonal sarcoma of the liver in adults. Cancer 2008;112:2274-2282.
16 Poggio JL, Nagorney DM, Nascimento AG, Rowland C, Kay P, Young RM, et al. Surgical treatment of adult primary hepatic sarcoma. Br J Surg 2000;87:1500-1505.
Received September 16, 2010
Accepted after revision January 17, 2011
Author Affiliations: Department of Surgery (Kim HH, Kim JC, Park EK, Hur YH, Koh YS, Cho CK and Kim HJ) and Department of Pathology (Kim HS), Chonnam National University Medical School, Gwangju, Korea
Jung Chul Kim, MD, PhD, Department of Surgery, Division of Hepatico-Biliary-Pancreatic Surgery, Chonnam National University Medical School, 671 Jebongno, Donggu, Gwangju, 501-757, Korea (Tel: +82-62-220-6451; Fax: +82-62-227-1635; Email: 3rdvivace@hanmail.net) © 2011, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(11)60112-4
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Risk factors of intrahepatic cholangiocarcinoma in patients with hepatolithiasis: a case-control study
- Fulminant liver failure models with subsequent encephalopathy in the mouse
- Relationship between pancreaticobiliary maljunction and gallbladder carcinoma: a meta-analysis
- Harmine induces apoptosis in HepG2 cells via mitochondrial signaling pathway
- Hepatobiliary & Pancreatic Diseases International (HBPD INT)
- Clinicopathological analysis of 14 patients with combined hepatocellular carcinoma and cholangiocarcinoma
