慢性胰腺炎胰腺钙化与烟酒关系初探
2010-11-23王伟廖专董元航李兆申张文俊王丽华邹多武金震东
王伟 廖专 董元航 李兆申 张文俊 王丽华 邹多武 金震东
·论著·
慢性胰腺炎胰腺钙化与烟酒关系初探
王伟 廖专 董元航 李兆申 张文俊 王丽华 邹多武 金震东
目的探讨国内慢性胰腺炎(CP)患者烟酒摄入量与发生胰腺钙化间的关系。方法按入院时有无胰腺钙化分为两组进行比较分析,再将无胰腺钙化者出院后有无新发胰腺钙化分为新发组和持续无钙化组。Logistic回归或Cox比例风险模型进行逐步回归分析胰腺钙化的风险因素。结果1997年1月到2007年7月共收治并成功随访449例CP患者,248例有胰腺钙化;201例无胰腺钙化,其中13例出院后新发生胰腺钙化。入院时胰腺钙化者的发病年龄小、病史长、糖尿病和腹泻发生率高。首发年龄≤40岁、酒精摄入量>20 g/d、糖尿病和腹泻为胰腺钙化风险因素;过量饮酒为无胰腺钙化CP患者新发生钙化的唯一风险因素(OR3.2)。结论饮酒增加CP患者胰腺钙化风险,建议戒酒;吸烟的作用需进一步研究。
胰腺炎,慢性; 钙质沉着症; 吸烟; 饮酒
慢性胰腺炎(chronic pancreatitis, CP)胰腺钙化机制尚不清楚。有研究认为,钙化始于胰管内蛋白栓子形成,继之钙离子沉积而成[1]。酒精为CP重要病因,吸烟为CP重要风险因素[2-3]。国外资料显示,烟酒与CP患者钙化有关[3-6]。CP患者在疾病初期戒烟亦可大大减少胰腺钙化风险[7]。但我国该方面资料少见,故回顾性分析近10年我院收治的CP患者资料,探讨国内CP患者烟酒摄入量与胰腺钙化间的关系,为临床研究提供参考。
资料和方法
一、临床资料
收集1997年1月到2007年7月间在我院住院治疗的所有CP患者。CP的诊断基于亚太诊断标准[5]。即典型的病史至少伴有如下表现之一:(1)病理见CP组织学特征; (2)影像学检查见胰腺钙化,包括胰管结石和胰腺实质钙化;(3)内镜下逆行胰胆管造影(ERCP)示胰管狭窄、扩张、不规则、粗细不均、串珠状改变等。
记录患者性别、病史、烟酒史和摄入量以及糖尿病、腹泻、体重下降等资料。日摄入酒精量>80 g(男)或>60 g(女),持续时间超过2年患者为酒精性CP[8];除外重度饮酒(>80 g/d)、遗传性、药物性、外伤性和甲状旁腺功能亢进等因素导致的CP为特发性CP(idiopathic chronic pancreatitis, ICP),发病<35岁为早发型ICP,>35岁为迟发型ICP[5]。吸烟者分为<100年支和>100年支两组。末次随访时间为2007年12月,随访时间平均(75±61)个月。
二、统计学方法

结 果
一、一般情况
共收治并成功随访449例CP患者,其中,酒精性79例(17.6%),ICP 345例(76.8%),其他因素所致者25例(5.6%)。有吸烟史233例,饮酒史230例,其中205例既吸烟又饮酒,吸烟与饮酒呈正相关(r=0.76,P=0.0000)。入院时胰腺钙化248例;无胰腺钙化201例,其中13例出院后随访发现胰腺钙化,188例持续无钙化。
二、风险因素分析
入院时胰腺钙化者的发病年龄小、病史长、糖尿病和腹泻发生率高(表1)。
首发年龄≤40岁、酒精摄入量>20 g/d、糖尿病和腹泻为胰腺钙化风险因素(表2)。
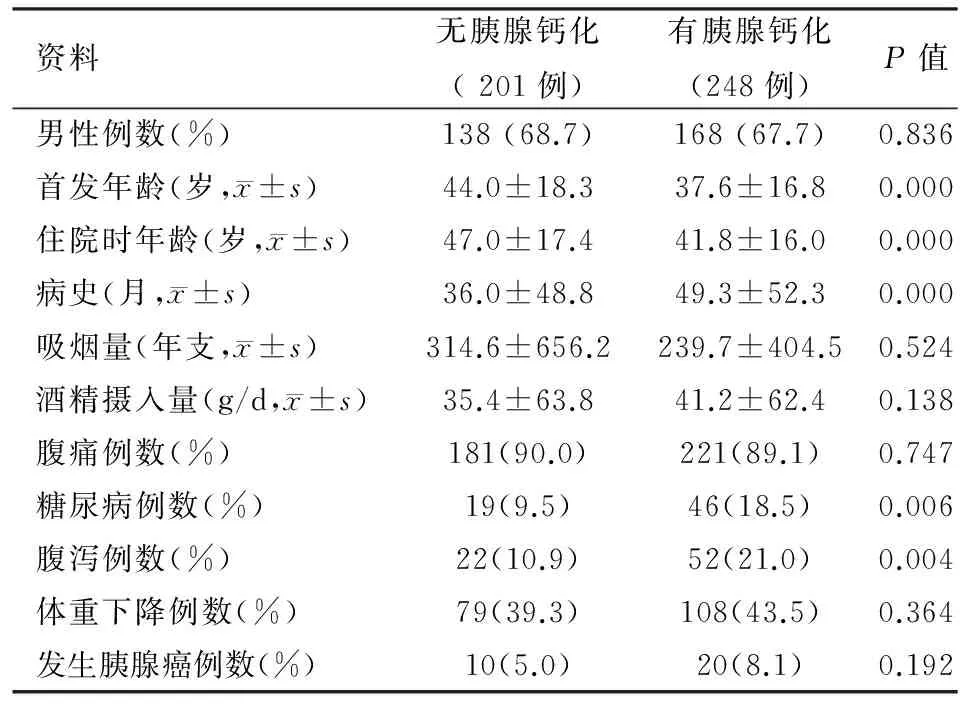
表1 449例慢性胰腺炎患者首次入院时的资料
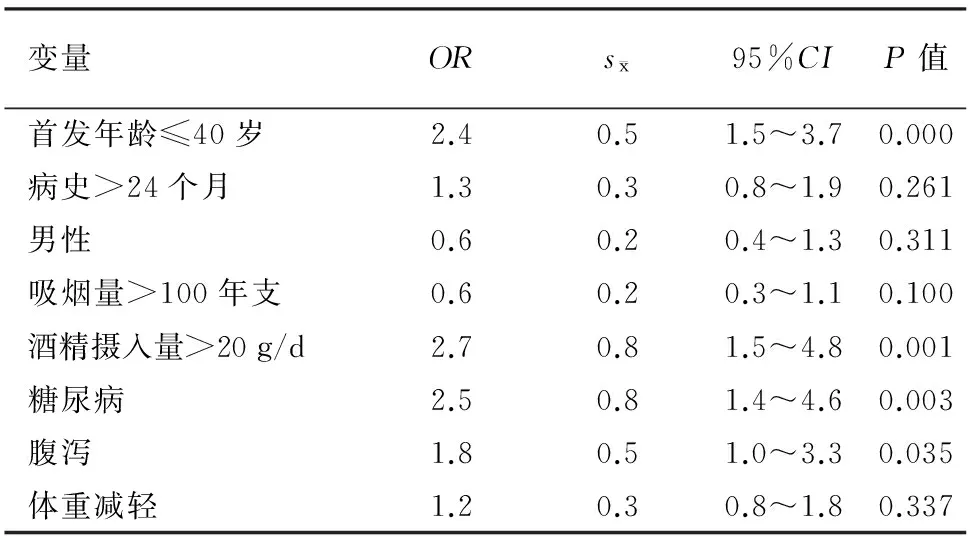
表2 CP胰腺钙化相关风险因素分析
三、新发胰腺钙化的风险因素
单因素和多因素Cox比例风险模型逐步回归分析显示,过量饮酒为无胰腺钙化CP患者新发生钙化的唯一风险因素(表3)。

表3 新发胰腺钙化单、多因素Cox比例风险模型分析
讨 论
本组显示,胰腺钙化患者入院时病史长,糖尿病、腹泻发生率高,其中糖尿病和腹泻为胰腺钙化风险因素之一,与CP基本特征[6,9]吻合。另外,本组胰腺钙化患者首发年龄较小,考虑与本组含青少年患者例数较多有关,亦提示应加强对青少年CP患者胰腺钙化机制及风险因素方面的研究。
胰腺钙化患者中过量饮酒者比率高,过量饮酒为胰腺钙化风险因素,且为出院后新发胰腺钙化的风险因素,均提示酒精的促胰腺钙化作用,与国外资料[7,9]类似。
吸烟与胰腺钙化的研究较复杂,原因是吸烟与饮酒往往相关,吸烟加速酒精导致的胰腺损伤[10],而饮酒为胰腺钙化的风险因素。本组出院后新发胰腺钙化患者单因素分析时发现过量吸烟(>100年支)发生胰腺钙化风险比为3.2,P=0.052,但多因素回归分析时吸烟因素被剔除,考虑该因素与饮酒呈正相关(相关系数0.76 ,P=0.0000 )或未知促钙化因素未纳入风险因素分析而影响统计结果有关。
Imoto等[1]研究了24和42例早发型和晚发型ICP(随访时间分别为27年和13年),晚发型ICP患者中吸烟者(>100年支)发生胰腺钙化率高于非吸烟者(83%对13%,P<0.0001),吸烟增加晚发型ICP胰腺钙化风险(相对危险度4.8)。Maisonneuve等[5]报道来自瑞士和意大利各83例ICP,前组显示吸烟同胰腺钙化无相关性(HR=0.64),后组则提示吸烟增加晚发型ICP胰腺钙化风险(HR=2.09)。Maisonneuve等[3]同时研究了1552例CP(酒精性CP 934例),随访(8.4±7.6)年,结果显示吸烟与CP确诊时的胰腺钙化显著相关(OR=2.0),CP确诊后胰腺钙化的发生同吸烟显著相关(HR=4.9)。Cavallini等[11]研究570例CP(酒精性459例),随访(10.4±6.4)年,发现吸烟同胰腺钙化相关(HR=1.2),即增加胰腺钙化风险20%。这些结论的不一致需要进一步的探索。
需要强调的是,吸烟诱使CP发生胰腺癌已有公认[6,12],其致癌机制为尼古丁的直接作用及激活致癌物或减弱抗蛋白酶活性等[9],因此CP患者戒烟的首要意义为减少癌症的发生、延长生存期[13]。
总之,胰腺钙化患者多表现为低龄、病史较长及糖尿病、腹泻,饮酒对CP胰腺钙化有显著促进作用,因此强烈建议CP患者戒酒。吸烟等其他风险因素在胰腺钙化中的作用尚待进一步研究。
[1] Imoto M,DiMagno EP.Cigarette smoking increases the risk of pancreatic calcification in late-onset but not early-onset idiopathic chronic pancreatitis.Pancreas,2000,21:115-119.
[2] Talamini G,Bassi C,Falconi M,et al.Alcohol and smoking as risk factors in chronic pancreatitis and pancreatic cancer. Dig Dis Sci,1999,44:1303-1311.
[3] Maisonneuve P,Lowenfels AB,Mullhaupt B,et al.Cigarette smoking accelerates progression of alcoholic chronic pancreatitis.Gut,2005,54:510-514.
[4] Frulloni L,Scattolini C,Graziani R,et al.Clinical and radiological outcome of patients suffering from chronic pancreatitis associated with gene mutations.Pancreas,2008,37:371-376.
[5] Maisonneuve P,Frulloni L,Müllhaupt B,et al.Impact of smoking on patients with idiopathic chronic pancreatitis.Pancreas,2006,33:163-168.
[6] Spanier BW,Dijkgraaf MG,Bruno MJ.Epidemiology,aetiology and outcome of acute and chronic pancreatitis:an update.Best Pract Res Clin Gastroenterol,2008,22:45-63.
[7] Talamini G,Bassi C,Falconi M,et al.Smoking cessation at the clinical onset of chronic pancreatitis and risk of pancreatic calcifications.Pancreas,2007,35: 320-326.
[8] Mullhaupt B,Truninger K,Ammann R.Impact of etiology on the painful early stage of chronic pancreatitis:a long-term prospective study. Z Gastroenterol,2005,43:1293-1301.
[9] Wittel UA, Hopt UT, Batra SK. Cigarette smoke-induced pancreatic damage:experimental data.Langenbecks Arch Surg,2008,393:581-588.
[10] Yadav D,Papachristou GI,Whitcomb DC.Alcohol-associated pancreatitis.Gastroenterol Clin North Am,2007,36:219-238.
[11] Cavallini G,Talamini G,Vaona B,et al.Effect of alcohol and smoking on pancreatic lithogenesis in the course of chronic pancreatitis. Pancreas,1994,9:42-46.
[12] Massarrat S.Smoking and gut.Arch Iran Med,2008,11:293-305.
[13] Pedrazzoli S,Pasquali C,Guzzinati S,et al.Survival rates and cause of death in 174 patients with chronic pancreatitis.J Gastrointest Surg,2008,12:1930-1937.
2009-07-08)
(本文编辑:屠振兴)
Impactofalcoholandsmokingonpancreaticcalcificationinchronicpancreatitis
WANGWei,LIAOZhuan,DONGYuan-hang,LIZhao-shen,ZHANGWen-jun,WANGLi-hua,ZOUDuo-wu,JINZhen-dong.
DepartmentofGastroenterology,ChanghaiHospital,SecondMilitaryMedicalUniversity,Shanghai200433,China
ObjectiveTo investigate the relationship between alcohol and smoking and the development of pancreatic calcification in chronic pancreatitis (CP) in China.MethodsThe patients were divided into two groups according to the presence of pancreatic calcification at admission and the data were analyzed; furthermore, the discharged patients without pancreatic calcification were divided into two groups as newly diagnosed pancreatic calcification group and persistent non-pancreatic calcification group. Logistic regression and Cox proportional-hazards model was used for multivariate analysis of the risk factors for pancreatic calcification.ResultsFrom January1997 to July 2007, 449 patients with CP were enrolled and followed up successfully. 248 patients presented with pancreatic calcification at admission; among the 201 patients presented without pancreatic calcification, 13 patients developed pancreatic calcification after discharge. Patients with pancreatic calcification had a young age at onset, long CP history, higher incidence of diabetes mellitus and diarrhea. Age at onset ≤ 40, alcohol intake over 20 g/day, and diabetes mellitus and diarrhea were risk factors for pancreatic calcification. The only risk factor of development of pancreatic calcification after discharge was excessive alcohol intake (OR: 3.2).ConclusionsAlcohol intake increased the risk of pancreatic calcifications, suggesting the patients abstain from alcohol intake. Further studies are necessary to clarify the role of smoking.
Pancreatitis, chronic; Calcinosis; Smoking; Alcohol drinking
Correspondingauther:LIZhao-shen,Email:zhaoshenlichhai@163.com
10.3760/cma.j.issn.1674-1935.2010.05.002
200433 上海,第二军医大学长海医院消化内科(慢性胰腺炎研究组)
李兆申,Email:zhaoshenlichhai@163.com
