Factors Influencing Pleural Effusion after Fontan Operation:an Analysis with 95 Patients
2010-11-22SongFuZhicunFengandSchranzDietmar
Song Fu ,Zhi-cun Feng *,and Schranz Dietmar
1Department of Children’s Heart Centre,BAYI Children’s Hospital,the Military General Hospital of Beijing PLA,Beijing 100700,China
2Department of Children’s Heart Centre,Justus-Liebig-University Giessen,Giessen 35385,Germany
THE Fontan procedure has been successfully used to treat univentricular heart.The procedure has undergone several modifications in an attempt to reduce the morbidity and mortality associated with this treatment.Although improvement has been achieved in the past few years,morbidity following Fontan procedure remains a challenge.Pleural effusion after the Fontan operation contributes significantly to morbidity and prolonged hospitalization.This study investigated the association between some selected preoperative,operative,and postoperative factors and persistent pleural effusion after extracardiac connection (EC) procedure.
PATIENTS AND METHODS
Patients
From June 1996 to July 2007,95 consecutive patients diagnosed with univentricular heart underwent EC using Gore-Tax conduits at the Department of Children’s Heart Centre,Justus-Liebig-University Giessen,Germany.Among them,60 (63.2%) patients were male and 35 (36.8%)were female.The median age of these patients was 57.12 momths (range,21.96-212.4 months),and the median weight was 13.8 kg (range,6.9-53.5 kg).
In this series,59 (62%) patients were diagnosed with single left ventricle,and 36 (38%) with single right ventricle.In addition,29 (31%) patients had transposition of the great arteries (TGA).The cardiac structure of all the patients fell into 8 different morphological types (Table 1).

Table 1.Anatomical diagnosis based on the morphological types of the cardiac structure of patients
Operative technique
Most patients had previous operation (Table 2).The mean number of times of previous operations was 2.1.
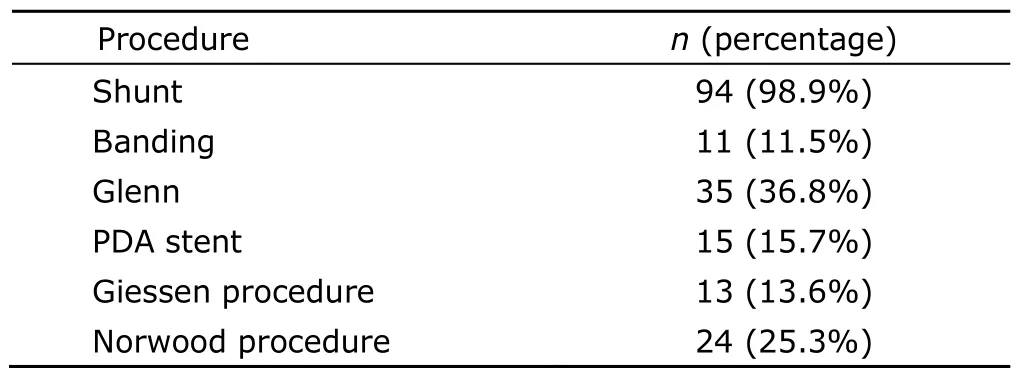
Table 2.Previous procedure before the Fontan operation
Standard cardiopulmonary bypass techniques were used after median sternotomy.After bicaval cannulation,the operation was performed under mild hypothermia(33-34°C).The priming solution of the extracorporeal circulation (ECC) consisted of 450 mL Ringer solution [in children with body weight less than 8 kg,200 mL Ringer solution was replaced by one unit (220 mL) of fresh frozen plasma],150 mL 20% human albumin,and 35 mL 8.4%NaHCO3.If the hemoglobin concentration of the patient was under 10 g/dL,one unit of erythrocyte concentrate(220 mL) was added to the solution.All the extracardiac conduits were connected with the heart beating and without cross-clamping the aorta.Atrial septectomy,when required,was performed during a short period of ventricular fibrillation.
For the EC procedure,polytetrafluoroethylene conduits were applied based on the weight and size of the patients.The conduit size was 20-22 mm in 82 patients,and 14-18 mm in 13 patients.The superior anastomosis between the conduit and the pulmonary artery was performed first.After allowing for the correct conduit length,the junction of inferior vena cava (IVC) and right atrium was incised to establish the IVC-conduit anastomosis,with the coronary sinus avoided.
Fenestration was performed by using a 4 or 5 mm coronary punch to the baffle,which was then connected to the right atrium side-by-side.It was done as a routine procedure if elevated pulmonary artery pressure,abnormal pulmonary artery anatomy,or severe atrioventricular valve regurgitation were present.Only when no signs of any factors that might compromise postoperative pulmonary circulation were present before the operation did we skip the routine fenestration.
Postoperative anticoagulation treatment
The initial step in our postoperative anticoagulation treatment was systemic heparinization,prolonging the plasma thrombin time (PTT) to 60 seconds for the first five postoperative days.This is followed by antiplatelet therapy(aspirin 1 mg/kg body weight) if no risk of thrombosis or any factors reducing velocity of blood flow in pulmonary circulation were present.When those problems appeared,the patients received Phenprocumone therapy with an international normalized ration (INR) of 2-2.5.A selfchecking system (Coagu-Check,Roche Ltd,Basel,Switzerland) was applied,and parents and patients were educated about its use.In the rare cases of enteropathy,low-molecular-weight heparin was administered subcutaneously.
Factors recorded before,during,and after the operation
Factors recorded before the operation included mean pulmonary artery pressure,ventricular end-diastolic pressure,preoperative oxygen saturation,and anatomical structure of the single ventricle.Operative factors included the use of fenestration,the size of the conduit used for construction of the extracardiac baffle,and the duration of cardiopulmonary bypass.After performing Fontan operation,we recorded three factors in the patients,namely postoperative pulmonary artery pressure (PAP),administration of angiotensin-converting enzyme inhibitors (ACEI),and occurrence of postoperative infection.
Evaluation of operative outcome
As a significant aspect of operative outcome,persistent pleural effusion in the present study was defined as pleural effusion lasting for more than 15 days after the operation or with an average drainage volume of more than 25 mL·kg-1·d-1.
Statistical analysis
The SPSS 10.0.0 version for Windows (SPSS Inc,Chicago,IL,USA) was used for data analysis.The data were presented as mean ± SD or range.All numerical data were initially analyzed for normality using the Kolmogorov-Smirnov test.Associations between persistent pleural effusion and demographic data as well as some preoperative,operative,and postoperative factors were analyzed by multivariate analysis and uniivariate analysis.Statistical significance was defined asPvalues less than 0.05.
RESULTS
Preoperative,operative,and postoperative factors
Some preoperative,operative,and postoperative factors recorded for the analysis of the association with operative outcome are summarized in Table 3.
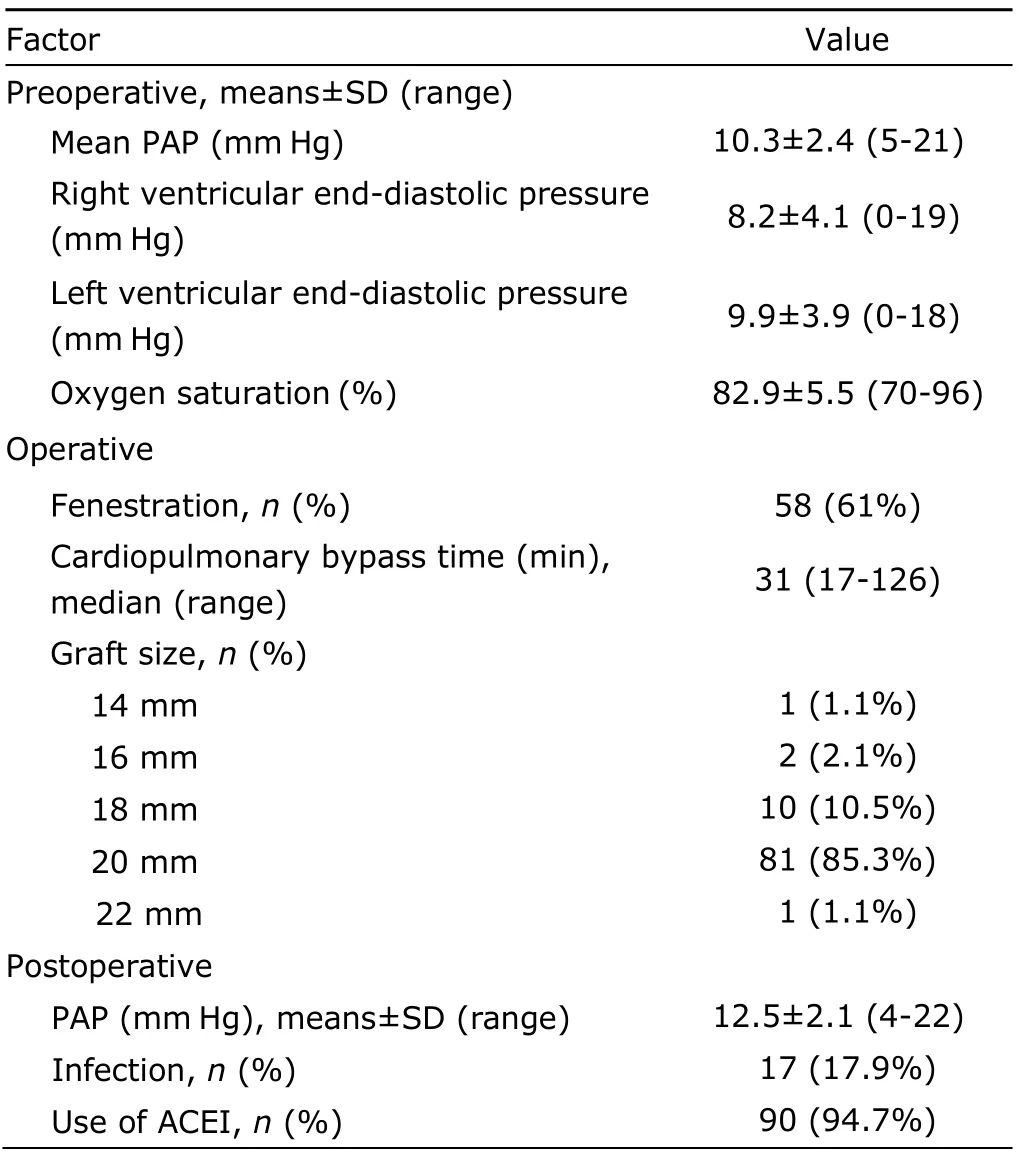
Table 3.Factors measured before,during,and after the Fontan procedure§
Operative outcome evaluated by pleural effusion
For all the 95 patients operated with Fontan procedure,the overall mortality was 3.2% (3 cases of death).Every patient developed postoperative pleural effusion.The median duration of chest tube output after the operation was 9 days (range,3-69 days),and the median volume was 12 mL·kg-1·d-1(range,2.0-37.5 mL·kg-1·d-1).Thirty-seven(38.9%) patients had pleural drainage lasting more than 15 days,and the volume in 35 (36.8%) patients exceeded 25 mL·kg-1·d-1.Nineteen (20%) patients required placement of additional chest tubes for re-accumulation of pleural effusion after removal of previous chest tubes.Fifteen (17.8%) patients required re-hospitalization because of pleural effusion after discharge.The median length of hospital stay after the operation was 14 days(range,4-78 days).
Factors associated with persistent pleural effusion
Demographic data and some preoperative,operative,and postoperative factors were evaluated for the association with persistent pleural effusion after the extracardiac Fontan procedure.Results showed that weight was not significantly related to the persistent pleural effusion.However,some risk factors were found to be significantly associated with prolonged duration (>15 days) or large volume (>25 mL·kg-1·d-1) of pleural drainage.The multivariate analysis showed that low preoperative oxygen saturation,non-fenestration,and postoperative infections were significantly associated with prolonged duration of chest tube output (P<0.05).Small conduit size,long cardiopulmonary bypass time,non-fenestration,and low preoperative oxygen saturation were significantly associated with excessive volume of chest tube output(P<0.05).In addition,the univariate analysis showed that dominant right ventricular lesions and the use of ACEI after the operation were significantly associated with prolonged duration;younger age and high preoperative PAP were significantly associated with excessive volume of pleural drainage (P<0.05) (Table 4).The analysis results of other factors did not reach the significance level.
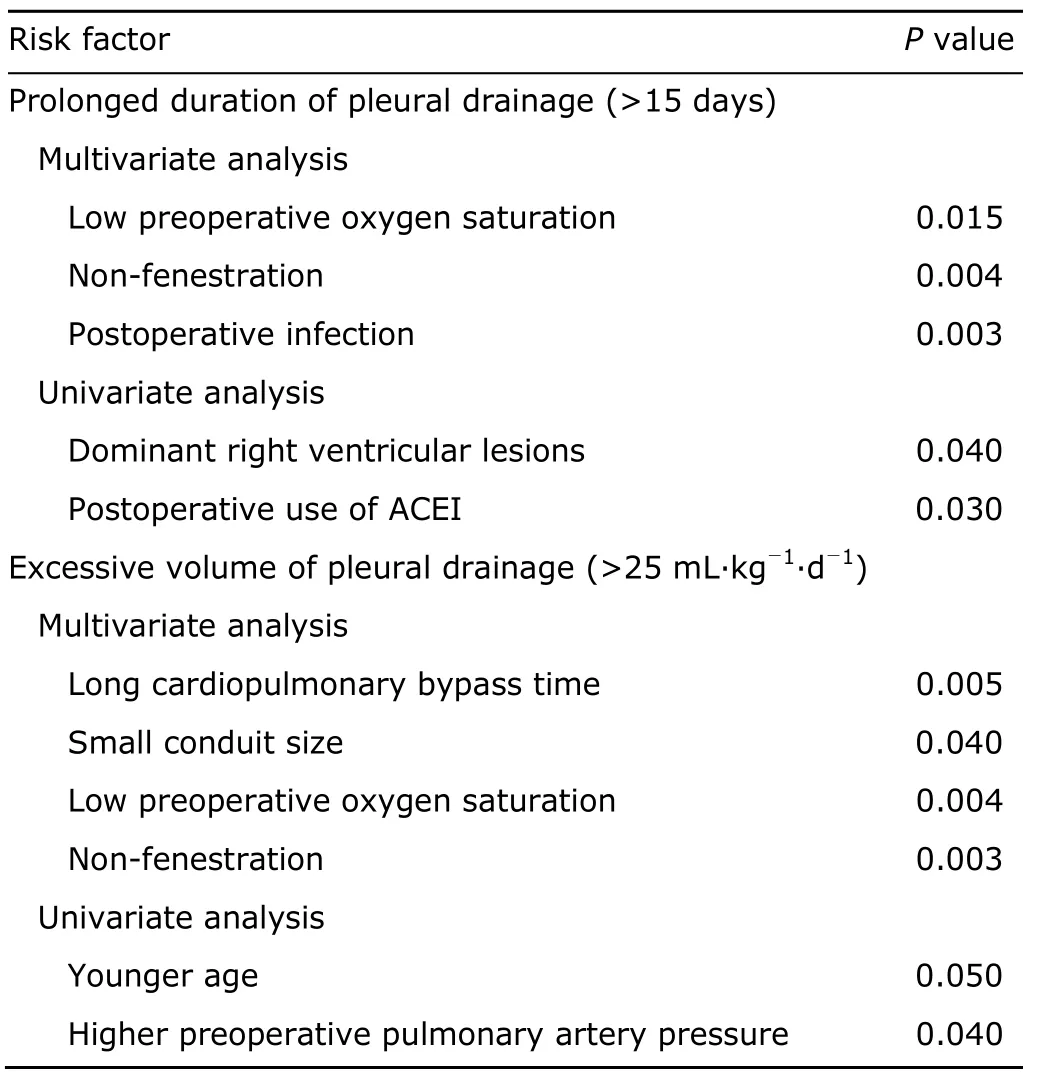
Table 4.Risk factors significantly associated with persistent pleural effusion after the extracardiac Fontan procedure
DISCUSSION
Three main mechanisms that may contribute to the development of persistent pleural effusion after the Fontan procedure were inflammatory,hydrostatic,and hormonal.The inflammatory response results mainly from exposure to cardiopulmonary bypass,1causing increased capillary leakage and subsequent fluid retention.Increased hydrostatic pressure in the Fontan circulation is caused by increased pulmonary vascular resistance,which is exacerbated by the absence of atrioventricular synchrony.The hormonal mechanism involves activation of the reninangiotensin system,2and more recent evidence suggests involvement of atrial natriuretic peptide and vasopressin.3
Fenestration of the atrial baffle was recommended on the basis that it allows a protective right-to-left shunt at the atrial level to overcome the low cardiac output in early postoperative period.4-7Lemler et al8demonstrated that fenestration significantly reduced both duration and volume of chest tube drainage,which is consistent with the findings of the present study.Benefits of baffle fenestration include improved ventricular preload,increased cardiac output,improved oxygen delivery,reduced systemic venous pressure,and decreased severity of pleural effusion.Fenestration has been reported to significantly reduce the duration of pleural effusion in several previous reports.9-12We routinely perform fenestration of the extracardiac baffle on patients with high risk in hemodynamics.In general,fenestration is recommended for patients with any of the following indicators:elevated pulmonary artery pressure,abnormal pulmonary artery,abnormal right ventricular anatomy,or significant atrioventricular valve regurgitation.Risk factors influencing pleural effusion include pulmonary artery pressure of or above 18 mm Hg,end-diastolic pressure of or above 12 mm Hg,valve regurgitation,pulmonary artery distortion,pulmonary vascular resistance of or above 2 Wood units,ventricular outflow obstruction,and complex anatomy.
The present study found low preoperative oxygen saturation is an independent risk factor for both prolonged duration and increased volume of pleural drainage after surgical intervention.Yet the underlying mechanism remains unclear.Preoperative oxygen saturation is a marker of total pulmonary blood flow,which is dependent on pulmonary vascular resistance.On the basis of the physiology of pulmonary blood flow,patients with higher pulmonary vascular resistance are likely to have lower preoperative saturation,and this might explain the occurrence of persistent pleural effusion.
Cardiopulmonary bypass time influences postoperative pleural drainage through development of inflammatory sequelae.The use of modified ultrafiltration has been reported to significantly reduce the incidence of postoperative pleural and pericardial effusion,demand for blood products,and hospital stay after the Fontan procedure.13The size of conduit used for construction of the extracardiac baffle was also found associated with excessive volume of pleural drainage after the operation.Although conduit size was partly determined by age and weight at the time of the operation,multivariate analysis showed that the effect of conduit size was independent of those two factors.In patients with conduit size smaller than 18 mm,83% developed persistent pleural effusion,compared with 13% in patients with larger conduits.We found small conduit size was positively correlated with high postoperative PAP,though statistically insignificant.
The use of ACEI after the operation was found positively associated with prolonged duration of pleural effusion by univariate analysis in the present study.There are conflicting reports about the influence of ACEI on the duration of pleural effusion after the Fontan procedure.14,15ACEI influence pleural drainage after surgical intervention through their action on the renin-angiotensin axis,which has been shown to contribute to the occurrence of prolonged pleural effusion after the Fontan procedure.16
Most previous studies have demonstrated that age is a risk factor for Fontan failure,but not a risk factor for persistent pleural effusion.17-19Because our study only involved extracardiac Fontan procedure,our patient population might differ slightly from those of other studies,which could be the reason for our contradictory results.High preoperative pulmonary artery pressure has also been reported as a risk factor for Fontan failure after the operation,20,21but not for persistent pleural effusion.18,21However,it was found to be significantly associated with increased volume of pleural drainage after the operation in our study.
In conclusion,for reduing postoperative duration and volume of pleural drainage following Fontan procedure,it seems to be important to improve the preoperative oxygen saturation,use large size of conduit,shorten cardiopulmonary bypass time,and make fenestration during the operation,as well as avoid postoperative infections.
1.Tam VK,Miller BE,Murphy K.Modified Fontan without use of cardiopulmonary bypass.Ann Thorac Surg 1999;68:1698-703.
2.Mainwaring RD,Lamberti JJ,Carter TL Jr,et al.Renin,angiotensin II,and the development of effusions following bidirectional Glenn and Fontan procedures.J Card Surg 1995;10:111-8.
3.Stewart JM,Gewitz MH,Clark BJ,et al.The role of vasopressin and atrial natriuretic factor in postoperative fluid retention after the Fontan procedure.J Thorac Cardiovasc Surg 1991;102:821-9.
4.Fu S,Valeske K,Akinturk H,et al.Fontan extracardiac tunnel connection:fenestration or not? Chin Med J (Engl)2009;122:2335-8.
5.Bridges ND,Lock JE,Castaneda AR.Baffle fenestration with subsequent transcatheter closure.Modification of the Fontan operation for patients at increased risk.Circulation 1990;82:1681-9.
6.Bridges ND,Mayer JE Jr,Lock JE,et al.Effect of baffle fenestration on outcome of the modified Fontan operation.Circulation 1992;86:1762-9.
7.Jacobs ML,Norwood WI Jr.Fontan operation:influence of modifications on morbidity and mortality.Ann Thorac Surg1994;58:945-52.
8.Lemler MS,Scott WA,Leonard SR,et al.Fenestration improves clinical outcome of the fontan procedure:a prospective,randomized study.Circulation 2002;105:207-12.
9.Geggel RL.Update on the modified Fontan procedure.Curr Opin Cardiol 1997;12:51-62.
10.Stamm C,Friehs I,Duebener LF,et al.Improving results of the modified Fontan in patients with heterotaxy syndrome.Ann Thorac Surg 2002;74:1967-77.
11.Bridges ND.Fenestration of the Fontan baffle:benefits and complications.Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 1998;1:9-14.
12.Koutlas TC,Gaynor JW,Nicolson SC,et al.Modified ultrafiltration reduces postoperative morbidity after cavopulmonary connection.Ann Thorac Surg 1997;64:37-42.
13.Thompson LD,McElhinney DB,Culbertson CB,et al.Perioperative administration of angiotensin converting enzyme inhibitors decreases the severity and duration of pleural effusions following bidirectional cavopulmonary anastomosis.Cardiol Young 2001;11:195-200.
14.Heragu N,Mahony L.Is captopril useful in decreasing pleural drainage in children after modified Fontan operation? Am J Cardiol 1999;84:1109-12.
15.Mainwaring RD,Lamberti JJ,Moore JW,et al.Comparison of the hormonal response after bidirectional Glenn and Fontan procedures.Ann Thorac Surg 1994;57:59-64.
16.Lamberti JJ,Mainwaring RD,Spicer RL,et al.Factors influencing perioperative morbidity during palliation of the univentricular heart.Ann Thorac Surg 1995;60 (6 Suppl):S550-3.
17.Fedderly RT,Whitstone BN,Frisbee SJ,et al.Factors related to pleural effusions after the Fontan procedure in the era of fenestration.Circulation 2001;104 (12 Suppl 1):I148-51.
18.Kaulitz R,Ziemer G,Luhmer I,et al.Total cavopulmonary anastomosis in patients less than three years of age.Ann Thorac Surg 1995;60(6 Suppl):S563-7.
19.Mayer JE,Bridges ND,Lock JE,et al.Factors associated with marked reduction in mortality for Fontan operations in patients with single ventricle.J Thorac Cardiovasc Surg 1992;103:444-52.
20.Knott-Craig CJ,Danielson GK,Schaff HV,et al.The modified Fontan operation.An analysis of risk factors for early postoperative death or takedown in 702 consecutive patients from one institution.J Thorac Cardiovasc Surg 1995;109:1237-43.
21.Hsu DT,Quaegebeur JM,Ing FF,et al.Outcome after the single-stage,nonfenestrated Fontan procedure.Circulation 1997;96 (9 Suppl):II-335-40.
杂志排行
Chinese Medical Sciences Journal的其它文章
- Sex Hormones and Androgen Receptor:Risk Factors of Coronary Heart Disease in Elderly Men△
- Comparison between Ophthalmologists and Community Health Workers in Screening of Shallow Anterior Chamber with Oblique Flashlight Test△
- Relationship between Carotid Atherosclerosis and Cerebral Infarction
- Expression of FLICE-inhibitory Protein in Synovial Tissue and Its Association with Synovial Inflammation in Juvenile Idiopathic Arthritis△
- A Case of Large“Silent”Extra-adrenal Retroperitoneal Paraganglioma Resected Laparoscopically
- Revascularization for Iliac-femoral Artery Pseudoaneurysm with Greater Saphenous Vein
