踝关节MR断层解剖、解剖变异和病理
——第二部分:解剖变异和病理
2010-09-05殷玉明
殷玉明
踝关节MR断层解剖、解剖变异和病理
——第二部分:解剖变异和病理
殷玉明
踝关节疼痛是一个非常常见的临床症状,病因很多,本文将引起踝关节疼痛病因的MR影像特征分为三部分进行描述:①侧副韧带损伤:侧副韧带损伤分为拉伤、部分撕裂和完全断裂。急性侧副韧带损伤MRI主要表现为韧带信号增高,韧带不规则断裂,界限不清,周围软组织水肿及邻近的骨水肿;慢性期的主要表现为韧带不规则增粗或变细。②肌腱病变:肌腱的病变大体上可分为肌腱病、部分肌腱撕裂、肌腱的完全断裂、肌腱纵向撕裂、肌腱腱鞘滑膜炎和肌腱脱位。单纯创伤性肌腱断裂很少见,多数肌腱断裂发生在肌腱病的基础之上。肌腱病变的MRI表现包括肌腱内信号增高,肌腱变粗或变细,边缘变得不锐利,肌腱周软组织水肿及肌腱鞘内积液。③骨、软骨及其他软组织病变:主要包括踝关节骨隐性压缩骨折、跖骨联合、副舟骨综合征、踝关节后撞击综合征、骨三角综合征、距骨骨软骨病变、和距骨缺血性坏死等。MRI能够准确的对上述疾病作出诊断及鉴别诊断。
踝关节;疼痛;韧带损伤;肌腱损伤;软组织损伤;磁共振成像
Ankle pain is a very common clinical presentation with a wide differential diagnosis. Ankle sprain is the most common cause of ankle pain. Other causes include tendon pathologies, bone and cartilage lesions and other soft tissue abnormalities such as sinus tarsi syndrome.
Ligaments pathologies:
Ankle ligamentous abnormalities are usually caused by traumatic injury. Magnetic resonance imaging (MRI) has been shown to be highly sensitive and accurate in identifying ligament injuries in the ankle. MRI can not only identify the number and extent of ligamentous tears, but also reveal other associated conditions including subtle fractures, osteochondral lesions, syndesmotic injuries, sinus tarsi syndrome, and associated muscle and tendon injuries. Ankleligamentous injuries are commonly classified into lateral ankle injuries, medial ankle injuries, and high ankle (syndesmotic) injuries. This division is based on anatomic regions and is arbitrary because many ankle injuries involve multiple groups of ligaments.
MR imaging appearances of the acute ligament injury can be graded according to the severity of the injury. Grade I injuries represent stretching of the ligament without fiber disruption. On MR imaging, the ligament may looks normal or slightly thickening with adjacent surrounding soft tissue edema. Grade II injuries represent partial tear of the ligament. MR images demonstrate thickening and edema of the ligament with partial f ber disruption and adjacent soft tissue edema. Grade III injuries represent complete tear of the ligament. MR images demonstrate complete discontinuity of the ligament with extensive surrounding soft tissue edema and joint fluid leak out side of the joint capsule. Other associated injuries including joint effusion, periarticular soft tissue edema, ruptured joint capsule, retinacular tears, tendon injuries and osteochondral injuries. Chronic ligament injuries on MRI may show thickening or thinning, discontinuity or nonvisualization of the ligament without signif cant surrounding soft tissue edema.
Lateral ligament injury
The lateral collateral ligaments complex includes anterior talofibular ligament (ATF), the calcanofibular ligament (CF), and the posterior talofibular ligament (PTF). The anterior talofibular ligament is the most commonly injured ligament. Followed by the CF ligament. The PTF tendon is the strongest ligament and its injury often occur in conjunction with injuries to other groups of ligaments, including the syndesmotic ligaments, the deltoid ligament, and fracture dislocation.
MRI evaluation
Axial and coronal MR images are usually adequate for assessing the lateral collateral ligaments. The sagittal images are usually better for assessing associated bony or other soft tissue injuries.


The normal ATF is a thin band of low signal extending from the talus to the fibula (Fig 1A). This ligament can be best seen on the axial images at the level below the talar dome. This ligament can be distinguished from the more superiorly located anterior inferior tibiofibular ligament (AITF) by two major criteria, the shape of the talus and the shape of the distal f bula on axial images. The talus appears oblong at the ATF ligament origin (Fig 1A) while the talus is square at the talar dome where the anterior inferior tibiof bular ligament is visualized (Fig 1B). The ATF inserts at thelevel of the fibular malleolar fossa where the fibula demonstrates a normal medial notch (Fig 1A), whereas the f bula is round at the insertion of the AITF (Fig 1B). MRI appearance of ATF ligament sprain caused by minor injury is thickening and increased signal within the ligament, indistinct margin, and adjacent soft tissue edema. Partial tear may be present (Fig 2). Complete rupture showed discontinuity of the ligament fibers, joint f uid may leak out of the capsule (Fig 3). Chronic ATF tear showed thickening and irregularity of the ligament without signif cant edema (Fig 4).


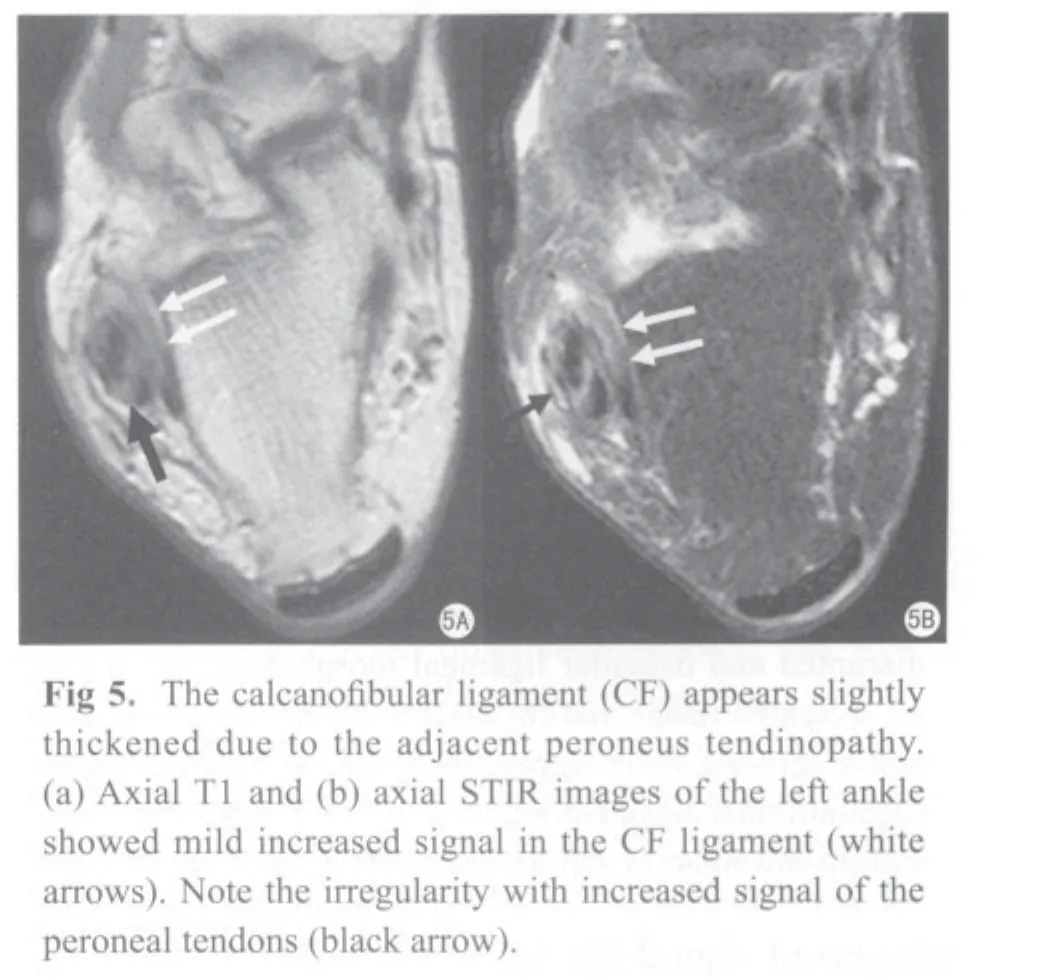
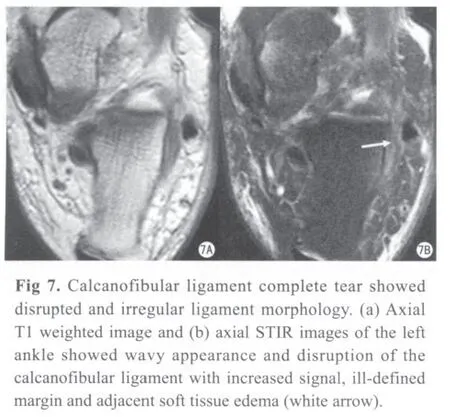
The normal calcanofibular ligament (CF) is frequently seen on axial images deep to the peroneal tendons along the lateral wall of the calcaneus and this ligament can be followed from the origin to the insertion on sequential coronal and axial images. Isolated CF is rare. This ligament is almost always associated with ATF injuries. Because the mid to distal segment of the CF ligament lies immediately underneath the peroneal tendon sheath, the more commonly occurred peroneal tendon pathology may extend to the CF ligament, which may demonstrateincreased signal on T2 weighted images, but is functionally intact (Fig 5). MR appearances of CF tear include localized edema between the lateral aspect of the calcaneus and peroneal tendons (Fig 6), disrupted and irregular ligament morphology (Fig 7), peroneal retinaculum thickening, and tenosynovitis.
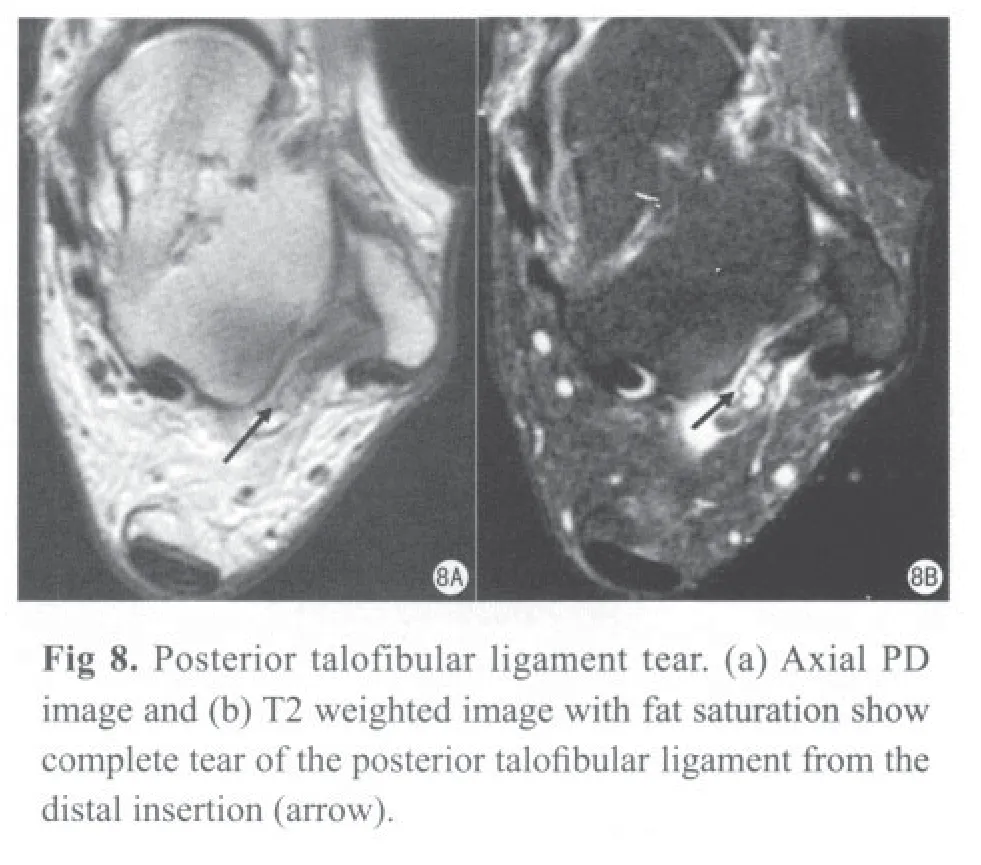
The PTF is usually the last ligament to be injured in the lateral collateral ligament complex injury. This ligament is fan shaped with a broad insertion into the fibular malleolar fossa. Normally, this ligament demonstrates inhomogeneous striated appearance because of interdigitating fat between ligament f bers. This striation should not be confused with a tear. MR appearances of the PTF tear include localized edema, disrupted and irregular ligament morphology (Fig 8), and loss of normal striated appearance.
Syndesmotic injuries
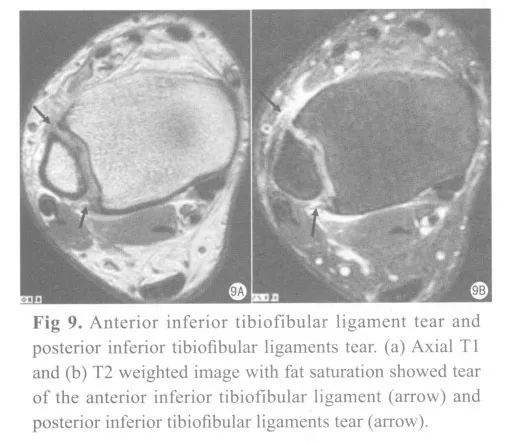
The ankle syndesmotic ligament complex consists of the anterior inferior tibiofibular ligament (AITF), the posterior inferior tibiofibular ligament (PITF), and the interosseous membrane. The AITF is the most important stabilizer and is the most frequently torn with syndesmotic injuries.
Syndesmotic ligamentous injury, also called high ankle sprain, indicates more severe ankle injury and often require longer recovery time. It may occur as an isolated injury or in association with lateral and medial collateral ligament injuries. The injury is common in young athletic individuals, especially those involved in high contact sports.
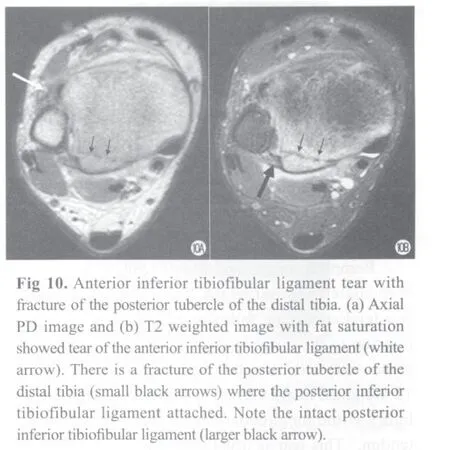
On MR imaging, the normal AITF and PITF are dark on all the sequences, but may have normal fenestrations and accessory fascicles. These two ligaments have oblique course arising from anterior and posterior tibial tubercles and extending inferolaterally to the anterior and posterior f bular tubercles respectively at the level of talar doom. MR findings of acute syndesmotic injuries include abnormal increased signal with thickening, discontinuity, contour alterations (wavy or curved ligaments), or nonvisualization of the ligament (Fig 9). An associated fracture of the tibia and/or fibula may also occur (Fig 10). When there is widening of the ankle mortise, additional axial images may be needed to cover more proximal located interosseous membrane.
The medial collateral ligament injury
The medial collateral ligament (MCL) or the deltoid ligament of the ankle consists of three superficial bands (tibionavicular, tibiocalcaneal, and superf cial posterior tibiotalar ligaments), and two deep bands (the anterior tibiotalar and the posterior tibiotalar ligaments). Isolated injuries to the deltoid are rare. Traumatic deltoid ligament injuries are more commonly associated with malleolar fractures, lateral ankle sprains, and syndesmotic diastasis.
On MR imaging, the normal superficial bands demonstrate well-defined, dark linear structure on all the MR sequences. The deep bands demonstrate inhomogeneous striated appearance owing the presents of fibrofatty tissue within the ligament fibers. Thedeltoid ligament injuries are best seen on coronal and axial images. The most common MRI findings of deltoid ligament injuries are morphologic changes and increased signal intensity. Absence of the ligament is rarely seen. An acutely torn ligament shows fascicular disruption, heterogeneity, and increased signal, best seen on the coronal images. The deep tibiotalar component, in particular, will often show loss of the orderly striation of the ligament and an increased interstitial signal with adjacent bone arrow edema at the attachment sites (Fig 11).
Tendon disorders:
Common ankle tendon disorders including tendinopathy, tenosynovitis and tendon tear. Ankle tendon injuries most commonly occur as a result of chronic microtearing due to overuse from athletic activity or primary degeneration. Traumatic tendon tear is uncommon, discrete tears of the ankle tendons commonly occur on a background of tendinopathy. Other tendon injuries include peritendinitis and dislocation.
Magnetic resonance imaging

Normal tendons demonstrate low signal intensity on both T1- and T2-weighted sequences. However, magic angle phenomenon is commonly seen in ankle tendons due to their changing course across the ankle. In generally, the tendon signal is only evaluated on T2-weighted sequences to minimize this effect. A trace of physiologic fluid may normally be present within ankle tendon sheaths. Tendinopathy generally has the same appearance on MRI in all tendons, manifested as increased tendon diameter and/or increased signal intensity on T2-weighted sequences. Occasionally, tendinopathy manifests as thinning and atrophy of the tendon. Longitudinal split tears are diagnosed when discrete linear high-signal areas seen parallel to the tendon fibers. Transverse tendon ruptures may be partial or complete and acute or chronic. In acute partial or complete ruptures, focally increased signalintensity, fluid like signal is present at the site of the tear. In chronic tears, scarring and f brosis may f ll the gap between the torn tendon f bers.
Tenosynovitis demonstrates increased f uid within the synovial tendon sheath with or without synovial thickening. The Achilles tendon is the only ankle tendon that does not have a tenosynovial covering and therefore the terms peritendinitis.
Peroneal brevis tendon
Peroneus longus and brevis tendons are located immediate posterior to the lateral malleolus. These two tendons can be followed from the myotendinous junction to the distal insertion. On MR imaging, both tendons are seen as solid black signal on both T1 and T2 weighted images. The most common lateral tendon injury is the longitudinal tear of the peroneus brevis tendon. This tear is usually at the level of the distal f bula where the tendon is forcibly compressed against the posterior f bular cortex during an inversion injury. This longitudinal intrasubstance tear of the peroneus brevis tendon has a distinct appearance on axial MR images. The tendon assumes a C-shaped conf guration that partially envelops the peroneus longus tendon (Fig 12).
Peroneus longus tendon
Peroneus longus injury often occurs distally adjacent to the peroneal tubercle in the midlateral calcaneus body or distally under the cuboid where the tendon changes direction from vertical to horizontal course. MRI appearance usually shows thickening of the tendon with increased signal (Fig13).
Peroneal tenosynovitis demonstrates thickening of the synovium surrounding the tendon with fluid collection within the tendon sheath (Fig 14).
Peroneus tendon dislocation
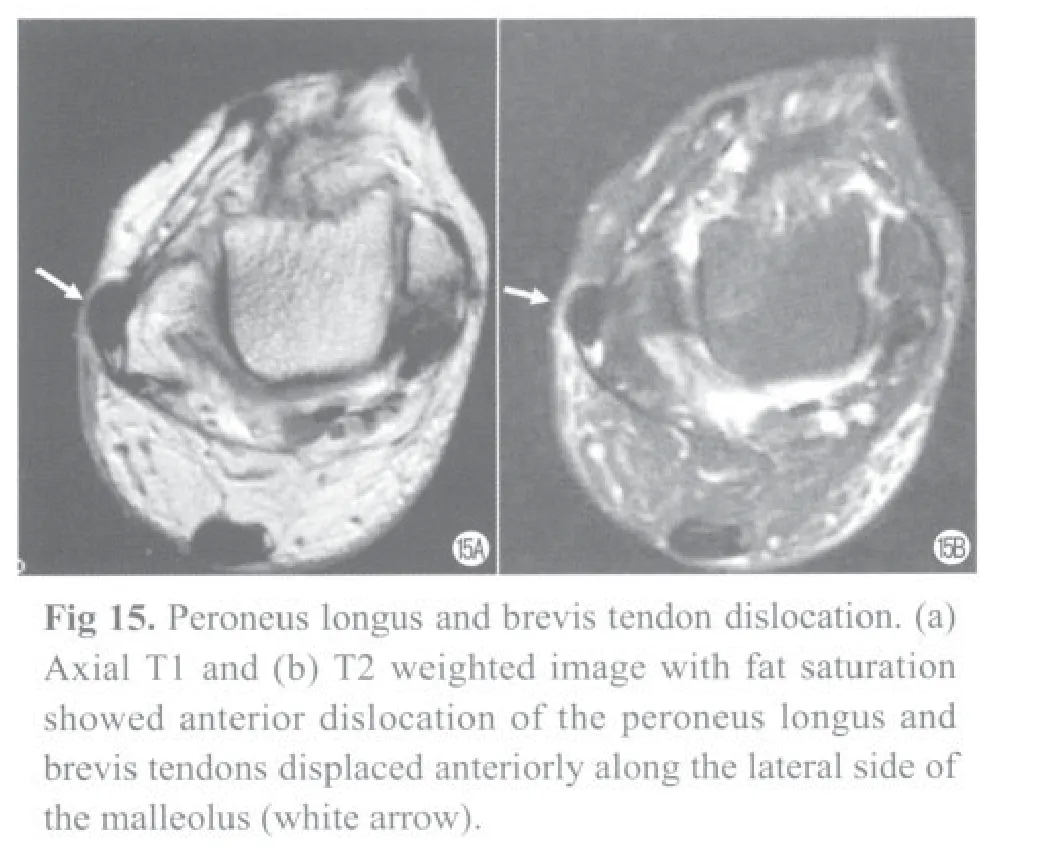
The major stabilizer of the peroneal tendon is superior peroneal retinaculum. Clinically, retinacular injury may manifest as retromalleolar pain with active ankle eversion. Because retinacular injury often occurs concurrently with lateral ligament sprain, this injury may be missed or misdiagnosed.
MR imaging features of retinacular injury include edema or discontinuity of the retinaculum and lateral and anterior subluxation of the peroneal tendons (Fig 15).




Posterior tibialis tendon (PT)
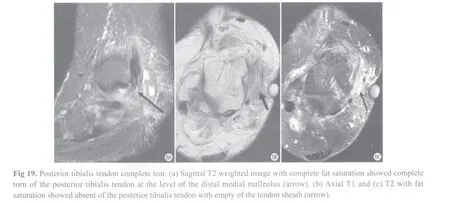
The posterior tibialis tendon lies along the posterior aspect of the medial malleolus. It is the most medial structure within the tarsal tunnel. The normal posterior tibialis tendon is seen about twice the diameter of the adjacent f exor digitorum longus tendon (Fig 16). The distal aspect of the posterior tibialis tendon passed the distal end of the medial malleolus may show higher signal intensity on both T1- and T2-weighted sequences owing to a combination of volume averaging from the multiple slips and oblique orientation of fibers and the magic angle phenomenon. Tendinopathy usually shows enlargement of the tendon (Fig 17), sometimes associated with longitudinal split (Fig 18). The tendon may become equal or smaller diameter compared with the adjacent f exor tendons, a condition called atrophic tendinopathy. Partial or complete tear of the tendon will show discontinuity of the f ber with retraction (Fig 19). In tenosynovitis, MRI will show excesses fluid in the tendon sheath (Fig 20).


Flexor hallucis longus tendon
Tenosynovitis of this tendon is relatively common because this tendon run through a fibro-osseous tunnel between the medial and lateral tubercles of the posterior talar process underneath the f exor retinaculum (Fig 21). It passes underneath the sustentaculum tali to the plantar aspect of the foot. The proximal course is better evaluated with axial images, the distal course should evaluated on coronal images and following to the distal insertion.Tenosynovitis manifests by a relatively large volume of fluid within the tendon sheath disproportionate to the quantity of f uid in the tibiotalar joint (Fig 22). However, small amount of the f uid can be normally present in the f exor hallucis longus tendon sheath, especially when you see large amount of the f uid in the tibiotalar joint due to communication (Fig 23).

Achilles tendon injuries
Achilles tendon injuries can be classified as midsubstance tendinopathy, insertional tendinopathy, longitudinal tear, partial tear and complete tear. Associated abnormalities include retrocalcaneal bursitis, Haglund’s deformity, and peritendinitis.
MR appearances
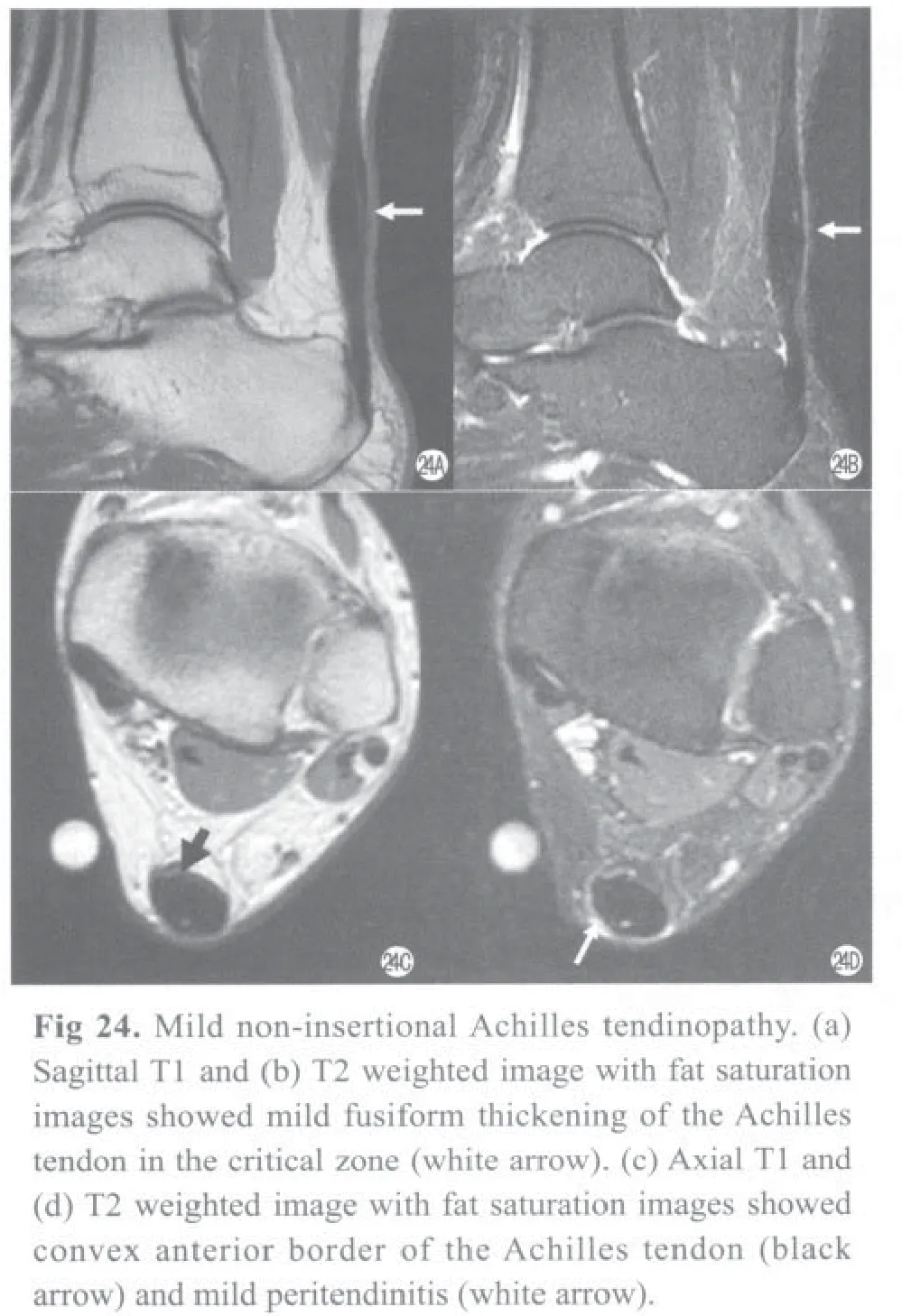
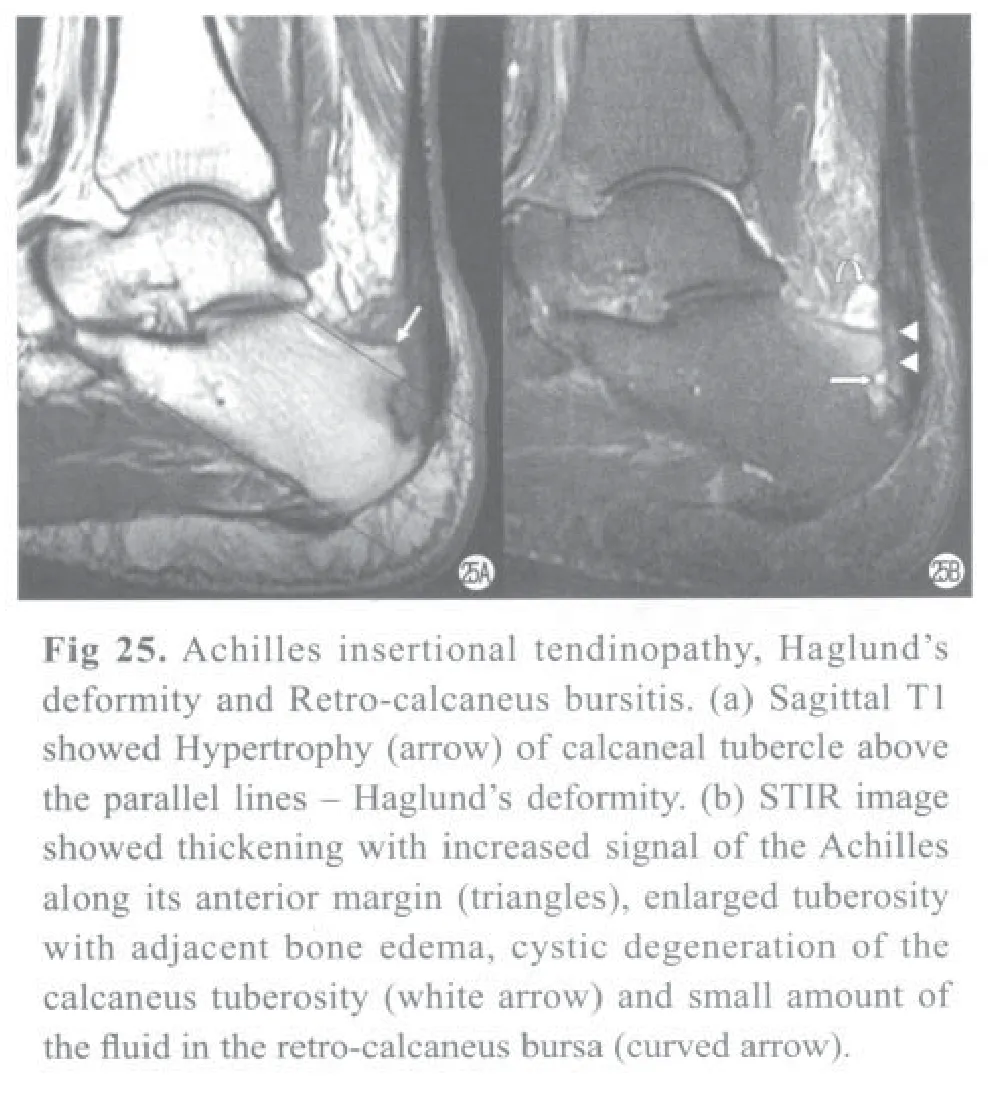
MR findings in midsubstance tendinopathy include focal fusiform thickening of the Achilles tendon, loss of the biconcave contour, and increased signal intensity in the hypovascular watershed zone 4 to 6 cm from the calcaneus insertion (Fig 24). Insertional tendinopathy demonstrates high signal at the calcaneal enthesis and is often associatedwith retrocalcaneal bursitis, Haglund's deformity, and bone marrow edema in the calcaneal tuberosity (Fig 25). In acute tears, it is important to measure the distance between the torn tendon edges because the degree of separation has implications for treatment. Paratendinitis and retrocalcaneal or retro-Achilles bursitis may be present either in isolation or associated with tendinopathy and demonstrate areas of increased signal intensity in their respective anatomic locations.

Anterior tibialis tendon
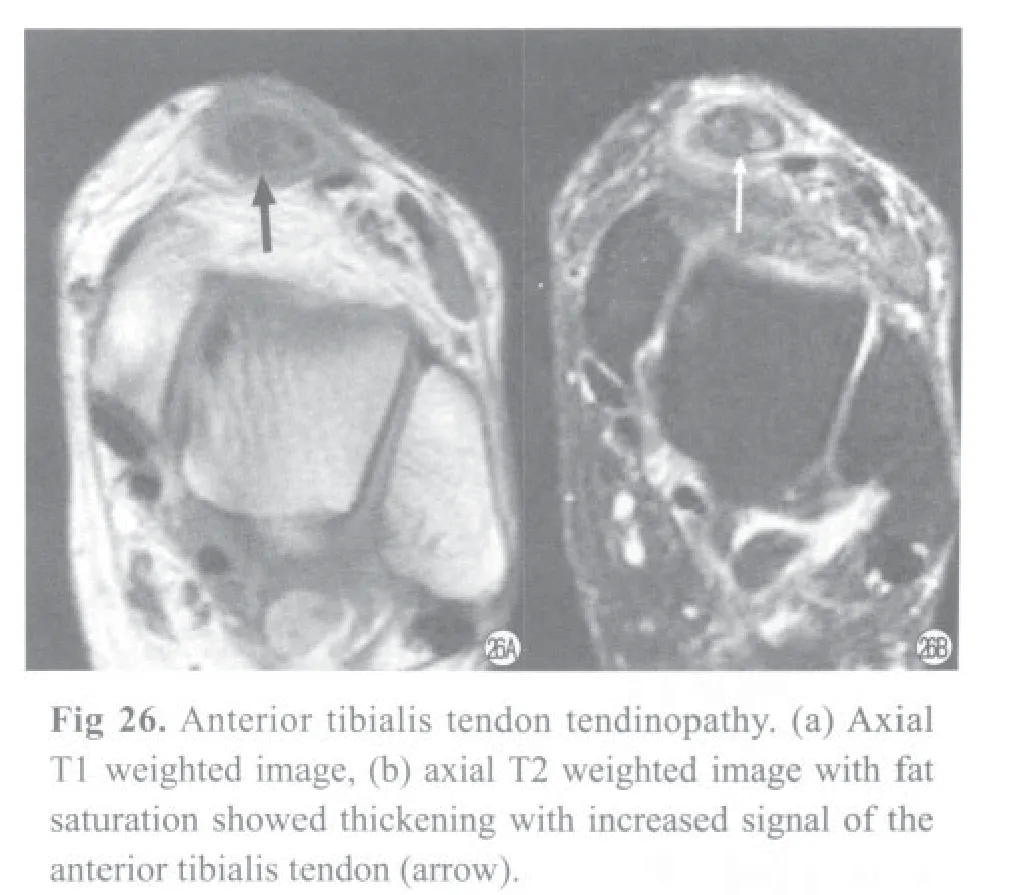
Tendinopathy and other pathologic processes affecting the anterior ankle tendons are less common than disorders of the other ankle tendons. Rupture typically occurs in elderly individuals after minor or no trauma. Anterior tibialis tendinopathy may result in extreme focal tendon enlargement (Fig 26) or tear with retraction mimicking a mass lesion above the anterior ankle joint and on imaging as tendon discontinuity (Fig 27).
(To be continued)
The ankle joint: MR sectional anatomy, anatomic variation and pathology. Part II: variation and pathology
Yuming Yin
Radiology Associates, LLP, Corpus Christi, TX, USA
*
Yin YM, E-mail: yyin@xraydocs.com
10 Aug 2010; Accepted 15 Sep 2010
Ankle pain is a very common clinical presentation. There are many disorders that can cause ankle pain. This article reviewed the MRI features of common etiologies that cause ankle pain in the following three categories: (1) Ligamentous injuries, that are commonly classif ed into lateral ankle injuries, medial ankle injuries, and high ankle (syndesmotic) injuries. Of the acute ligament injury, the ligament shows increased signal with adjacent surrounding soft tissue edema on MR imaging, and partial tear of the ligament is observed. Chronic ligament injuries mainly represent thickening or thinning, discontinuity or nonvisualization of the ligament. (2) Tendon disorders, that include tendinopathy, tendon tears, tenosynovitis, peritendinitis and dislocation. Traumatic tendon tear is uncommon, discrete tears of the ankle tendons commonly occur on a background of tendinopathy. MRI can accurately show the characteristics of the disorders above. (3) Bone, cartilage and other soft tissue disorders, including subtle fracture of the anterior process of the calcaneus, tarsal coalition, accessory navicular syndrome, Os Trigonum syndrome, osteochondral lesion of the talus, and avascular necrosis of the talus. MRI can make diagnosis or differential diagnosis from the disorders.
Ankle joint; Pain; Ligamentous injuries; Tendon disorders; Soft tissue injuries; Magnetic resonance imaging
book=337,ebook=41
Radiology Associates, LLP, Corpus Christi, TX, USA
Yuming Yin, E-mail: yyin@xraydocs.com
2010-08-10接受日期:2010-09-15
R684;R445.2
A
10.3969/j.issn.1674-8034.2010.05.005
殷玉明. 踝关节MR断层解剖、解剖变异和病理——第二部分:解剖变异和病理. 磁共振成像, 2010, 1(5): 337-345.
Acknowledgement
The author would like to thank professor Shinong Pan (潘诗农) for his excellent translation of the abstract from English to Chinese.
