Differential Diagnosis of Warthin's Tumor Complicated with Lung Adenocarcinoma by 18F- FDG PET/CT Imaging and Radioisotope Scanning with Tc-99m Pertechnetate: A Case Report and Literature Review
2010-07-18TingzhengFangJiaruiZhuLingChuanWenruiZhaoYingkuiLiangShengWang
Ting-zheng Fang, Jia-rui Zhu, Ling Chuan, Wen-rui Zhao, Ying-kui Liang, Sheng Wang
Department of Nuclear Medicine, Navy General Hospital of PLA, Beijing 100048, China
Differential Diagnosis of Warthin's Tumor Complicated with Lung Adenocarcinoma by 18F- FDG PET/CT Imaging and Radioisotope Scanning with Tc-99m Pertechnetate: A Case Report and Literature Review
Ting-zheng Fang, Jia-rui Zhu*, Ling Chuan, Wen-rui Zhao, Ying-kui Liang, Sheng Wang
Department of Nuclear Medicine, Navy General Hospital of PLA, Beijing 100048, China
A seventy eight years old male patient underwent a whole body 18F- FDG PET/CT imaging to diagnose the lesion which was showed in the right lung by a chest X ray test and CT scan before. Besides the intense 18F- FDG uptake of the lesion in the right lung, a lesion in the left parotid gland also showed intense 18F- FDG uptake. To evaluate the pathology of the lesion in the left parotid gland, a parotid gland scintigraphy imaging with Tc-99m pertechnetate was done and revealed a Warthin’s tumor. Later a fine needle aspiration(FNA) confirmed that it was a Warthin’s tumor.
Warthin’s tumor; Lung adenocarcinoma; 18F- FDG; PET/CT; Tc-99m pertechnetate; SPECT
INTRODUCTION
The Warthin’s tumor what is called adenolymphoma is a benign parotid gland tumor characterized histologically by tall columnar and oncocytic epithelium within a lymphoid tissue stroma[1,2]. WHO and Armed Forces Institute of Pathology designed this entity adenolymphoma, while the use of Warthin’s tumor pays homage to Warthin who reported the first two cases in America[1]. It is generally accepted that the tumor arises from heterotopic salivary tissue trapped within a lymph node during embryogenesis and has a remarkable relativity with smoking[1,3,4]. Most of the Warthin’s tumor occurred in parotid glands except for a few cases reported in the lip and the palate[1,3]. Its peak incidence is frequently reported in the 60s and 70s[1,3,5]. Although the male patients are still notably more than female patients, the male-to-female ratios have decreased steadily since the 1940s and are quite common as less than 2∶1, simultaneously with theincrease in the tobacco consumption among women[1,3,4]. As the second most common benign parotid tumor (benign mixed tumors are the most common tumor), Warthin’s tumor accounts for 6%-10%, and even 24.4% of parotid gland epithelial tumors, and 2% of all head and neck tumors[1,3,5,6]. A good many of reports have identified a bilateral incidence of 3%-10%, a multiple incidence of 4%-12% and a nearly equal incidence of each parotid gland[1,3,6,7].
CASE REPORT
The patient was a seventy eight years old man. In June 2008, a chest X ray test of the routine health examination showed that there was a lesion in the patient’s right lung. The physical examination results were negative. A chest computed tomography(CT) scan was carried out soon and showed that the lesion was in the inferior lobe of right lung and highly suspicious to be malignant. For diagnosis and staging, the patient underwent an 18F- Fluorodeoxyglucose (FDG) positive emission tomography (PET/CT) imaging from the pelvis to the maxilla days later. The patient was asked to fast for at least 4 h beforeundergoing the examination. He had glucose level below 150 mg/dL and received an IV injection of 370 MBq(10 mCi) of FDG. Data acquisitions were performed 60 minutes after injection using an integrated in-line PET/CT system (Discovery LS, GE Healthcare).
In the inferior lobe of right lung there was a lesion of 2.5cm×1.8 cm in size with intense 18F- FDG uptake. Its CT value and SUVave/max was 22-55 HU and 8.0/10.9 respectively. Besides the lesion in right lung, there was a high density and intense 18F- FDG uptake lesion at the lower pole of left parotid gland (Figure 1). The size of the lesion was 0.9cm×1.1cm, while its CT value and SUVave/max was 33-46 HU and 10.9/14.2 respectively. The lesion in the inferior lobe of right lung was regarded as a lung cancer in the PET/CT report. Because of the low incidence rate of the lung cancer metastasis in parotid glands, the lesion in the left parotid gland was regarded as a primary tumor of parotid gland. Furthermore, benign tumors were dominate types of parotid gland tumors and there was often high FDG uptake in some benign parotid gland tumors, particularly in Warthin’s tumor in parotid gland. Finally, the lesion in the left parotid gland was considered as a parotid gland benign tumor in the PET/CT report. In order to evaluate the pathology of the lesion, a parotid gland scintigraphy imaging with Tc-99m pertechnetate was done. It was showed that there was a hot lesion in the corresponding site of the left parotid gland, although the salivary glands showed bilaterally symmetrical and enhanced tracer uptake (Figure 2). After the vitamin C tablet was administered and kept in the mouth, the tracer uptake of the hot lesion increased, while the tracer uptake of the normal parotid gland decreased (Figure 3). Then the patient underwent a fine needle aspiration (FNA) of the lesion in the left parotid gland. The pathology examination showed that there was lymphoid stroma which was covered by double layer of oncocyti epithelial cells. The inner row that are basilar, whereas outer layer tended to palisade toward the luminal surface(Figure 4). The report revealed that it was a Warthin’s tumor. At last, the patient was clinically diagnosed as right lung cancer and left parotid gland Warthin’s tumor. He underwent a operation inferior lobe of right lung resection on Second July 2008. The pathology examination of the resected lung cancer was poorly differentiated adenocarcinoma without lymphatic metastasis (T1N0M0).
DISCUSSION
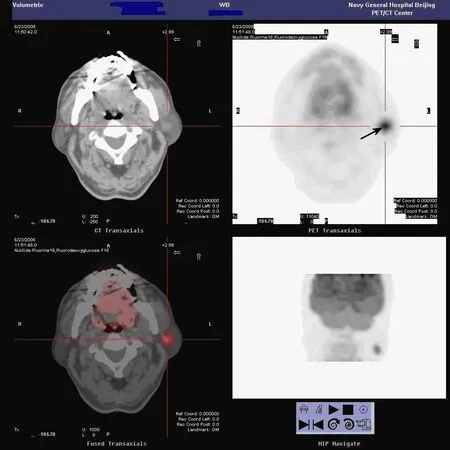
Figure 1. The PET/CT shows that there is a high density and intense 18F- FDG uptake lesion (arrow) in the left parotid gland.

Figure 2. The image before vitamin C tablet is aministered shows that although the salivary glands show bilaterally symmetrical and enhanced tracer uptake, there is a hot lesion (arrow) in the left parotid gland.

Figure 3. The washout image shows the tracer uptake of the hot lesion (arrow) increased, while the tracer uptake of the normal parotid gland decreased.

Fiture 4. The pathology examination shows that there is lymphoid stroma which is covered by double layer of oncocyti epithelial cells. The inner row that is basilar, whereas outer layer tended to palisade toward the luminal surface.
The radioisotope scanning with Tc-99m pertechnetate of Warthin’s tumor was positive and strongly recommended to be used to distinguish the Warthin’s tumor from other parotid gland tumors[3,5,8-10,12,14]. The technique is well established and involves imaging of the parotid gland in the posterior projection after the intravenous infusion of 5 mCi of the tracer at 60s intervals for 20 min and obtaining final images of the patient after hydration in right lateral and left lateral positions, followed by washout images obtained 3 min after stimulation with orally administered lemon juice or Vitamin C tablet to determine adequacy and symmetry of glandular secretion[3,5,8-10]. While both normal parotid glands and most other parotid abnormalities drain upon stimulation, the washout pattern images of Warthin’s tumor show unchanged or even increased activity uptake[3,5]. This is very important in diagnosing Warthin’s tumor. With respect to the mechanism of positive imaging of Warthin’s tumor, Nishiyama Y reported that the Na+-K+ATPase was found on the baso-lateral side of the epithelial cells of adenolymphoma and the striated duct cells of the parotid gland, and this activity of Na+-K+ATPase may enhance the accumulation of Tc-99m pertechnetate in these cells[8]. Because Warthin’s tumor does not communicate with ductal system, the accumulated Tc-99m pertechnetate remains in the gland without being secreted after administering[3,5]. Although the oncocytoma yields a similar hot scan, it demonstrates a cavitary appearances which the Wathin’s tumor would not show, because the former concentrates the nuclide within the proper tumor cells whereas Warthin’s tumor concentrates within the tumor mass[3].
The 18F- FDG PET imaging was an extensively used malignant tumor diagnosis and staging protocol. The malignant tumor was usually high uptake mainly because of its high level of glucose metabolism. However, 18F- FDG was not a specific malignant tumor tracer. Except the physiological concentration of 18F- FDG, benign lesions with increased FDG uptake are found in more than 25% of the PET/CT studies performed in patients with proven or suspected malignancy, with inflammation being the most common cause[11]. The high FDG uptake in some benign parotid gland tumors, particularly Warthin’s tumor, was extensively observed and reported[9,11-14]. This tumor may be found incidentally during FDG PET studies. Horiuchi M et al reported in the cancer screening with FDG PET for 1,872 medical health club members, high FDG accumulation in the parotid gland was found in four males (age, 57-70 years), who were finally diagnosed as Warthin's tumor by surgical pathology[14]. In a retrospective study of seventy-two patients with benign parotid gland tumors (n=52), malignant parotid tumors (n=12), and inflammation (n=8), Malignant parotid tumors showed significantly higher FDG uptake (standard uptake values [SUVs]) than both benign tumors and inflammation, except in Warthin's tumor[9]. The SUV values of Warthin's tumor and malignant parotid tumors even overlapped somewhat, therefore, the diagnostic value of 18FFDG imaging in the Warthin's tumor was limited[9]. In another retrospective study of 25 patients who underwent conventional whole-body FDG-PET or PET/CT for malignant disease else where and had demonstrated varying patterns of FDG uptake (unilateral, bilateral, symmetric, or asymmetric) in the parotid glands, five of the seven patients who had asymmetric focal uptake in one of the parotids were found to have focal lesions which were finally diagnosed based upon histopathology as primary parotid tumors (e.g., Warthin's tumor and pleomorphic adenoma) or metastatic disease involvement, while patients of other patterns had no clearcut pathology by clinical or radiological examinations[13]. In wholebody 18F- FDG PET, a bilaterally symmetrical increased uptake of parotid glands was usually physiological while a asymmetrical uptake, especially when focal, would warrant further radiological and histopathological correlation to rule out disease involvement[13]. Combining salivary gland scintigraphy with FDG PET may be a promising approach for differentiation of Warthin’s tumor[9].
The CT portion of the PET/CT increased the specificity of the characterization of the benign lesions, especially for which had moderate or marked 18F- FDG uptake[11]. Considering the notable percentage (6%-24%) of Warthin’s tumor in the parotid tumors[1,3,5,6], the positive 18F- FDG PET/CT imaging of parotid glands, especially whenasymmetrical and focal, should be interpreted cautiously with the characterization on the integrated CT and thought as a signal of radioisotope scanning with Tc-99m pertechnetate[9,12,14]and FNA.
REFERENCES
[1] Rice DH. Salivary Gland Disorders∶ neoplastic and nonneoplastic[J]. Med Clin North Am 1999; 83∶197-218.
[2] Saxena A, Memauri B, Hasegawa W. Initial diagnosis of small lymphocytic lymphoma in parotidectomy for Wathin tumour, a rare collision tumour[J]. J Clin Pathol 2005; 58∶ 331-3.
[3] Weinstein GS, Harvey RT, Zimmer W, et al. Technetium-99m pertechnetate salivary gland imaging∶ its role in the diagnosis of Warthin’s tumor [J]. J Nucl Med 1994; 35∶ 179-83.
[4] Lamelas J, Terry JH, Alfonso AE. Warthin’s tumor∶multicentricity and increasing incidence in women[J]. Am J Surg 1987; 154∶ 347-51.
[5] Higashi T, Murahashi H, Iluta H, et al. Identification of Warthin’s tumor with technetium-99m pertechnetate[J]. Clin Nucl Med 1987; 12∶ 796-800.
[6] Batsakis JG. Carcinoma ex papillary cystadenoma lymphomatosum malignant Warthin’s tumor[J]. Ann Otol Rhinol laryngol 1987; 96∶ 234-5.
[7] Finkelstein DM, Noyek AM, Chapnik JS. Multiple bilateral synchronous Warthin’s tumors∶ a case report and review of the literature[J]. J Otolaryngol 1989; 18∶ 357-61.
[8] Nishiyama Y. The mechanism of positive scintigraphy with 99m Tc-pertechnetate in adenolymphomas of the parotid grand[J]. Nippon Jibiinkoka Gakkai Kaiho(in Japanese) 1998; 101∶ 615-9.
[9] Uchida Y, Minoshima S, Kawata T, et al. Diagnostic value of FDG PET and salivary gland scintigraphy for parotid tumors[J]. Clin Nucl Med 2005; 30∶ 170-6.
[10] Sostre S, Medina L, de Arellano GR. The various scintigraphic patterns of Warthin's tumor[J]. Clin Nuc Med 1987; 12∶ 620-6.
[11] Metser U, Miller E, Lerman H, et al. Benign nonphysiologic lesions with increased 18F- FDG uptake on PET/CT∶ characterization and incidence[J]. AJR Am J Roentgenol 2007; 189∶1203-10.
[12] Ozawa N, Okamura T, Koyama K, et al. Retrospective review∶ usefulness of a number of imaging modalities including CT, MRI, technetium-99m pertechnetate scintigraphy, gallium-67 scintigraphy and F-18-FDG PET in the differentiation of benign from malignant parotid masses[J]. Radiat Med 2006; 24∶ 41-9.
[13] Basu S, Houseni M, Alavi A. Significance of incidental fluorodeoxyglucose uptake in the parotid glands and its impact on patient management[J]. Nucl Med Commun 2008; 29∶ 367-73.
[14] Horiuchi M, Yasuda S, Shohtsu A, et al. Four cases of Warthin's tumor of the parotid gland detected with FDG PET[J]. Ann Nucl Med 1998; 12∶ 47-50.
R735.7 Document code: A Article ID: 1000-9604(2010)02-0163-04
10.1007/s11670-010-0163-z
2009−12−15; Accepted 2010−02−26
*Corresponding author.
E-mail∶ jiarui_zhu@sina.com
© Chinese Anti-Cancer Association and Springer-Verlag Berlin Heidelberg 2010
杂志排行
Chinese Journal of Cancer Research的其它文章
- Triptolide Inhibits Cell Growth and Induces G0- G1 Arrest by Regulating P21wap1/cip1 and P27 kip1 in Human Multiple Myeloma RPMI-8226 Cells
- Different Outcome of Myeloid Sarcoma with Spinal Cord Compression Preceding Acute Myeloid Leukemia: Report of Two Cases and Review of Literatures
- Effects of Triptolide on Histone Acetylation and HDAC8 Expression in Multiple Myeloma in vitro
- CGI-100 Specific shRNA Inhibits Proliferation and Induces Differentiation in Leukemia K562 Cells
- Expression of Embryonic Stem Cell Marker Oct-4 and Its Prognostic Significance in Rectal Adenocarcinoma
- Synergistic Action of fMLP-boanmycin Combination on the Growth of Mouse Colon Carcinoma and Its Action Mechanisms
