心血管病患者的P波峰值时间与阵发性房颤的相关性研究
2024-12-18杜幸张永军
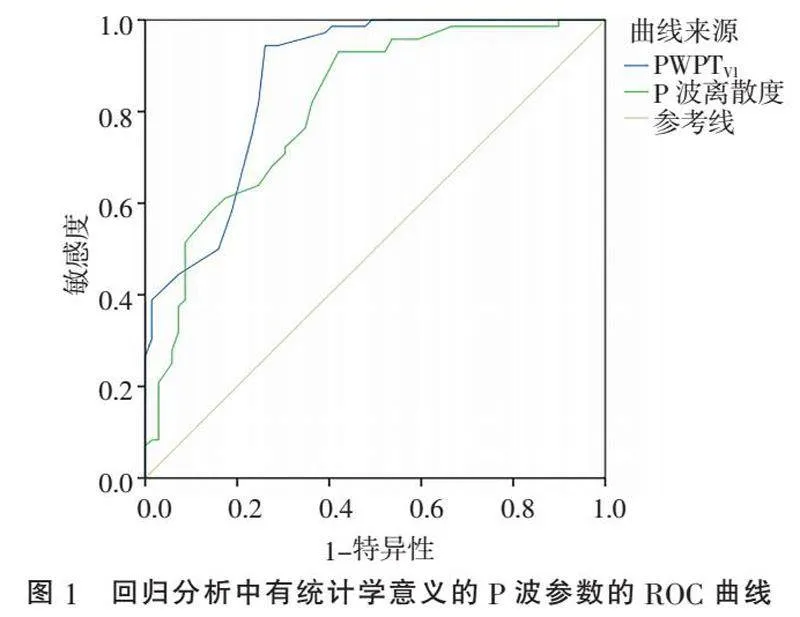
[摘" "要]" "目的:在心血管病人群中,探讨P波峰值时间(P-wave peak time, PWPT)与阵发性房颤(paroxysmal atrial fibrillation, PAF)的潜在关联。方法:随机选择2022年8月—2023年2月期间在皖南医学院第一附属医院心血管内科住院治疗的141例患者,根据有无房颤病史、常规心电图及动态心电图结果,分为PAF组和非PAF组。回顾性分析患者在住院期间的超声心动图、常规心电图结果并搜集相关数据。采用SPSS 23.0软件对数据进行统计分析。结果:PAF组的PR间期(P=0.006)、P波离散度(Plt;0.001)、P波最大时限(Plt;0.001)、PWPTV1(Plt;0.001)及P波电轴(P=0.041)均显著大于非PAF组。PAF组的QT间期(P=0.001)及QTc(Plt;0.001)要长于非PAF组。多因素Logistic回归分析结果显示,P波离散度(OR=1.11,Plt;0.001)及PWPTV1(OR=1.32,Plt;0.001)是PAF的独立危险因素。在ROC曲线的分析及比较中,PWPTV1和P波离散度的AUC分别为0.870和0.811(P=0.1903),最佳诊断分界点分别为37.5 ms(敏感度94.4%,特异度73.9%)和29.5 ms(敏感度93.1%,特异度58.0%)。结论:PWPTV1是PAF的独立危险因素,可以早期识别房颤高风险人群。
[关键词]" "阵发性房颤;P波峰值时间;P波指数;P波离散度
[中图分类号]" "R541.7" " " " " " " "[文献标志码]" "A" " " " " " " "[文章编号]" "1674-7887(2024)05-0411-05
A clinical study on the correlation between P-wave peak time and paroxysmal atrial fibrillation in patients with cardiovascular disorders
DU Xing ZHANG Yongjun" " " "(Department of Electrophysiology, the First Affiliated Hospital of Wannan Medical College, Anhui 241000)
[Abstract]" "Objective: In the patients with cardiovascular disorders, to explore the potential association between P-wave peak time(PWPT) and paroxysmal atrial fibrillation(PAF). Methods: Between August 2022 and February 2023, 141 patients admitted to the First Affiliated Hospital of Wannan Medical College Cardiovascular Department for inpatient treatment were randomly selected and divided into PAF and non-PAF groups based on a history with or without atrial fibrillation, routine electrocardiogram, and dynamic electrocardiogram results. Review of patients' echocardiography and routine electrocardiogram results during hospitalization and collection of relevant data were conducted. Data were analyzed using SPSS 23.0 software. Results: There were statistically significant differences between the two groups in PR interval(P=0.006), P-wave dispersion(Plt;0.001), P-wave maximum duration(Plt;0.001), PWPTV1(Plt;0.001), and P-wave axis(P=0.041), with all of these P-wave parameters being significantly larger in the PAF group than non-PAF group. The QT interval(P=0.001) and QTc(Plt;0.001) were longer in the PAF group. Multivariate Logistic regression analysis results showed that P-wave dispersion(OR=1.11, Plt;0.001) and PWPTV1(OR= 1.32, Plt;0.001) were independent risk factors for PAF. In ROC curve analysis and comparison, the AUC for PWPTV1 and P-wave dispersion were 0.870 and 0.811, respectively(P=0.1903), with optimal diagnostic cutoff points of 37.5 ms(sensitivity 94.4%, specificity 73.9%) and 29.5 ms(sensitivity 93.1%, specificity 58.0%), respectively. Conclusion: PWPTV1 is an independent risk factor for PAF and can identify high-risk individuals for atrial fibrillation early.
[Key words]" "paroxysmal atrial fibrillation; P-wave peak time; P-wave index; P-wave dispersion
心房颤动(简称房颤)是临床上常见的心律失常,随着人口老龄化和心血管疾病发生率的不断升高,房颤的患病率也在随之增加[1]。房颤与较高的死亡率和各种心脑血管事件的发生率相关,并会导致患者生活质量降低、运动能力下降和心力衰竭症状加重[2],这极大地增加了社会负担,使其成为全球性的公共卫生问题[3]。尽管目前有常规心电图、动态心电图等检查手段用于筛查房颤,但因其监测时间的限制,仍有相当一部分阵发性房颤(paroxysmal atrial fibrillation, PAF)的患者可能未被及时发现。因此,寻求相关指标对房颤进行早期准确的预测是十分有价值的。
近年来,研究[4]发现,PR间期和P波指数(P-wave indices, PWIs)在普通人群中预测房颤的发生有一定价值。PWIs包括PR间期、P波最大时限、P波离散度、V1导联P波终末电势(P-wave terminal force, PWTF)和P波电轴[5]。与这些经典的参数不同,P波峰值时间(P-wave peak time, PWPT)是一个新的心电参数,其与心肌梗死患者的再灌注损伤有关[6]。本研究旨在探讨心血管病患者的PWPT与房颤之间的潜在关联。
1" "对象与方法
1.1" "研究对象" "选择2022年8月—2023年2月期间在皖南医学院第一附属医院心血管内科住院治疗的141例患者为研究对象,根据有无房颤病史、常规心电图及动态心电图结果,分为PAF组(n=72)和非PAF组(n=69)。PAF组纳入标准:(1)以PAF收住入院;(2)既往无房颤病史,此次入院经动态心电图检查诊断为PAF;(3)有常规心电图检查并记录到窦性心律。非PAF组纳入标准:既往无房颤病史,且此次入院行常规心电图及动态心电图检查显示主导节律均为窦性心律的患者。排除标准:(1)持续性房颤;(2)房颤行射频消融术后;(3)起搏器植入术后;(4)急性心肌梗死;(5)心电图检查结果缺失。本研究方案经皖南医学院第一附属医院医学伦理委员会批准(审批号:202230)。
1.2" "方法
1.2.1" "超声心动图检查" "回顾患者在住院期间的超声心动图检查结果,并搜集左室射血分数、有无中重度心脏瓣膜病变、有无左室肥厚、室间隔厚度、左房前后径、左室舒张末期内径及升主动脉内径等相关参数。
1.2.2" "心电图检查" "患者在静息状态下行常规12导联心电图检查,要求电极摆放准确、基线平稳、无伪差干扰,走纸速度25 mm/s,振幅10 mm/mV。患者常规心电图均使用麦迪克斯心电系统记录,由同一名心电图医师复测审核。每份心电图共复测3次,取平均值作为最终参数。(1)PR间期:自P波起点至QRS波群起点的一段时间。(2)PWPT:自P波起点至P波顶点的垂线之间的时间,分别在Ⅱ导联和V1导联进行测量。如果为负向或双相P波(指负向部分振幅≥0.1 mV),则从P波起点测量至负向部分最低点的垂线之间的时间。(3)P波最大时限:同步测量12个导联的P波起始至结束的持续时间,取其中最长者。(4)P波离散度:在12导联中测量到的最长P波持续时间和最短P波持续时间之差。(5)V1导联PWTF:P波负向部分的深度乘以它的宽度,异常PWTF是指PWTF≥40 mm·ms。(6)P波电轴:P波的额面平均心电轴,正常参考值范围为0°~+75°。
1.2.3" "统计学方法" "采用SPSS 23.0软件对数据进行统计分析。数据正态性检验用Kolmogorov-Smirnov方法,符合正态分布的计量资料以x±s表示,偏态分布计量资料以M(P25, P75)表示,计数资料以n(%)表示。正态分布计量资料的组间比较采用t检验,偏态分布计量资料采用秩和检验,计数资料的组间比较采用χ2检验。用Logistic回归分析确定PAF的独立危险因素。对回归分析确定的参数进行ROC曲线分析。P<0.05为差异有统计学意义。
2" "结" " " 果
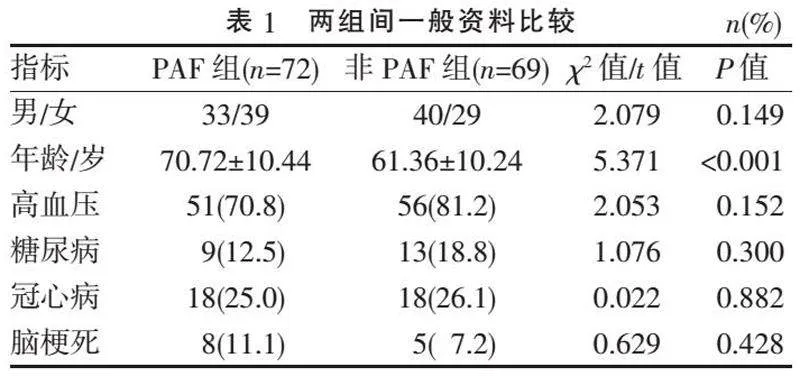
2.1" "两组一般资料比较" "PAF组年龄大于非PAF组(Plt;0.001),两组间性别构成、合并基础疾病情况比较,差异均无统计学意义(均P>0.05),见表1。
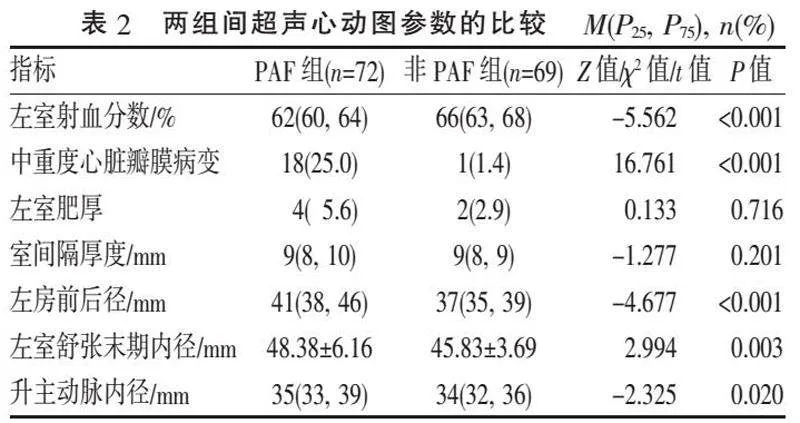
2.2" "两组超声心动图参数比较" "PAF组重度心脏瓣膜病变比例、左房前后径、左室舒张末期内径及升主动脉内径均明显大于非PAF组(均Plt;0.05);PAF组左室射血分数低于非PAF组(Plt;0.001);两组间左室肥厚和室间隔厚度差异无统计学意义(Pgt;0.05),见表2。
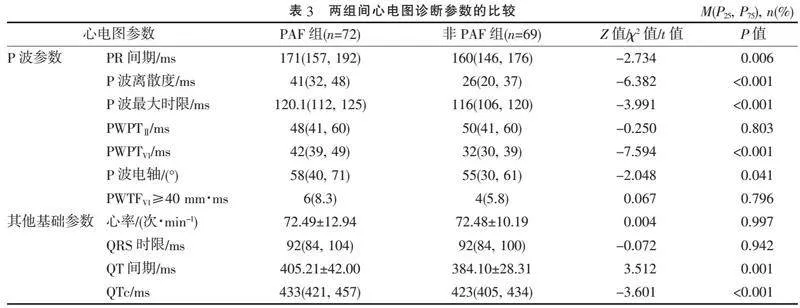
2.3" "两组心电图参数比较" "两组P波参数比较,PAF组的PR间期、P波离散度、P波最大时限、PWPTV1及P波电轴均显著大于非PAF组(均Plt;0.05),PWPTⅡ和PWTFV1则在两组间差异无统计学意义(Pgt;0.05);在其他基础心电图参数中,PAF组的QT间期和QTc要长于非PAF组(均Plt;0.05),而心率和QRS时限差异无统计学意义(Pgt;0.05),见表3。
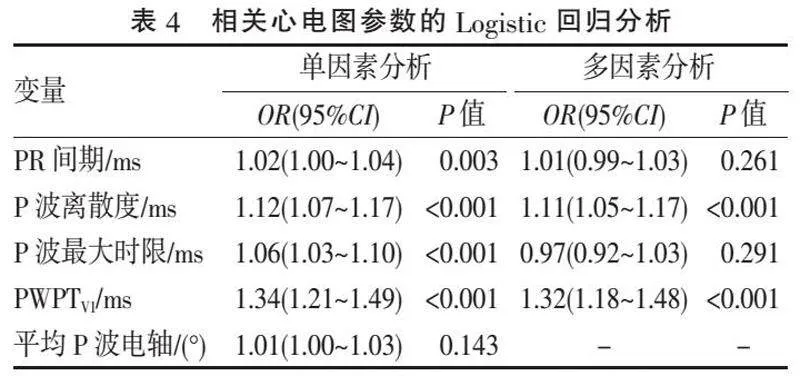
2.4" "Logistic回归与ROC曲线分析" "采用Logistic回归分析PAF与P波参数的关联性,先用单因素分析对相关参数进行筛选,对筛选出的有统计学意义的参数再做多因素Logistic回归分析。结果显示,P波离散度(OR=1.11,Plt;0.001)及PWPTV1(OR=1.32,Plt;0.001)是PAF的独立危险因素,见表4。
PWPTV1和P波离散度的AUC分别为0.870和0.811(图1),两者间差异无统计学意义(P=0.190)。PWPTV1和P波离散度的最佳诊断分界点分别为37.5 ms(敏感度94.4%,特异度73.9%)和29.5 ms(敏感度93.1%,特异度58.0%)。
3" "讨" " " 论
PAF患者通常会伴有心房结构重构和电重构。房颤的发生与心房结构重构密切相关,左心房内径增大可较好地早期预测PAF的发生[7]。本研究中PAF组左房前后径、左室舒张末期内径、升主动脉内径及中重度心脏瓣膜病变比例均大于非PAF组,而左室射血分数则小于非PAF组,差异均有统计学意义。上述结构性改变会使心房的电传导发生相应变化,表现为伴随心电图上多个P波参数的改变。
PWIs是由体表心电图测量得出的心房电活动的定量指标[8]。近年来,随着PWIs与房颤之间相关性的研究越来越多,人们逐渐认识到P波的分析在预测房颤上具有重要价值[9]。当然,其中也有部分PWIs如PWTF、P波最大时限等的意义存在争议。研究[10]表明,PWTF在缺血性卒中患者中对PAF的预测敏感性较高,但特异性不强。而在M.A.BATUROVA等[11]的研究中,PWTF可能不是脑卒中患者有PAF的一个很好的预测指标。本研究结果与后者一致,V1导联PWTF在两组间差异无统计学意义。此外,P波时限通常被认为是反映心房传导最可靠的无创性指标,它的延长与PAF有关。但在一些报道[12-13]中,PAF患者没有表现出显著的P波时限延长。本研究中,P波最大时限有组间差异,但不是PAF的独立危险因素。同样地,房颤与P波离散度[14]、P波电轴[15]、PR间期[16]、QT间期和QTc[17]之间的关系也在本研究中得到了验证,上述参数在PAF与非PAF组间差异均有统计学意义,但仅有P波离散度是PAF的独立危险因素。
据报道[6],冠心病患者的PWPT与左心房功能受损显著相关。也有学者[18]发现在非ST段抬高的心肌梗死患者中,Ⅱ导联PWPT的延长可能与冠脉病变严重程度有关。PWPT延长代表房内或房间传导时间延长,在糖尿病和血液透析患者中可以预测左心房容积指数的升高[19]。另一项研究[20]表明,P波振幅的减小与冷冻球囊消融术后房颤复发率的降低有关。虽然该参数与本研究的PWPT不同,却揭示了房颤与P波波峰(包括振幅及时限)之间有着潜在的联系。V.SGRIGNA等[21]在二尖瓣狭窄并发房颤患者的P波持续时间与左房大小的相关性研究中发现:PAF患者P波达到最大振幅的时间明显较晚,支持了本研究结果。本研究发现PAF组的PWPTV1显著大于非PAF组(Plt;0.05),而PWPTⅡ在两组间则差异无统计学意义。这与A.ÖZ等[22]报道的急性缺血性脑卒中患者PWPTⅡ与PAF显著相关有所不同。临床上有一部分心电图Ⅱ导联的P波会呈没有明显波峰的低平形态,或呈现“等电线-负向-正向”的形态[23],这就对Ⅱ导联PWPT的测量结果造成一定影响,也可能是本研究中PWPTⅡ并无组间差异的原因。起搏点位于窦房结尾部,前结间束或上房间支传导阻滞[23]或心房肌纤维化[24]等均会导致Ⅱ导联窦性P波形态发生上述变异。此外,本研究还显示PWPTV1与经典的心电图参数P波离散度一样,是PAF的独立危险因素,PWPTV1值越大,患者发生房颤的风险就越高。PWPTV1对心血管病患者PAF的预测(截断点为37.5 ms)具有较高的敏感度和特异度。与P波离散度相比,PWPTV1在常规心电图上更方便测量,因而具有更高的实用性。
综上所述,在心血管病人群中,PWPTV1是PAF的独立危险因素。PWPTV1可以早期识别房颤高风险人群,从而实施有针对性的密切监测和更积极的危险因素治疗。
[参考文献]
[1]" "DILAVERIS P E, GIALAFOS E J, ANDRIKOPOULOS G K, et al. Clinical and electrocardiographic predictors of recurrent atrial fibrillation[J]. Pacing Clin Electrophysiol, 2000, 23(3):352-358.
[2]" "CHÁVEZ-GONZÁLEZ E, DONOIU I. Utility of P-wave dispersion in the prediction of atrial fibrillation[J]. Curr Health Sci J, 2017, 43(1):5-11.
[3]" "WOLF P A, MITCHELL J B, BAKER C S, et al. Impact of atrial fibrillation on mortality, stroke, and medical costs[J]. Arch Intern Med, 1998, 158(3):229-234.
[4]" "GERMAN D M, KABIR M M, DEWLAND T A, et al. Atrial fibrillation predictors: importance of the electrocardiogram[J]. Ann Noninvasive Electrocardiol, 2016, 21(1):20-29.
[5]" "MAHESHWARI A, NORBY F L, SOLIMAN E Z, et al. Refining prediction of atrial fibrillation risk in the general population with analysis of P-wave axis(from the atherosclerosis risk in communities study)[J]. 2017, 120(11):1980-1984.
[6]" "ÇAGDAS M, KARAKOYUN S, RENCÜZOGULLAR1 Ì, et al. P wave peak time; a novel electrocardiographic parameter in the assessment of coronary no-reflow[J]. J Electrocardiol, 2017, 50(5):584-590.
[7]" "曹鹏, 廉伟, 曹源, 等. 心房结构性重构与阵发性心房颤动的相关性和预测意义[J]. 中国慢性病预防与控制, 2020, 28(9):696-698.
[8]" "MAGNANI J W, WILLIAMSON M A, ELLINOR P T, et al. P wave indices: current status and future directions in epidemiology, clinical, and research applications[J]. Circ Arrhythm Electrophysiol, 2009, 2(1):72-79.
[9]" "PLATONOV P G. P-wave morphology: underlying mechanisms and clinical implications[J]. Ann Noninvasive Electrocardiol, 2012, 17(3):161-169.
[10]" "GODA T, SUGIYAMA Y, OHARA N, et al. P-wave terminal force in lead V1 predicts paroxysmal atrial fibrillation in acute ischemic stroke[J]. J Stroke Cerebrovasc Dis, 2017, 26(9):1912-1915.
[11]" "BATUROVA M A, SHELDON S H, CARLSON J, et al. Electrocardiographic and echocardiographic predictors of paroxysmal atrial fibrillation detected after ischemic stroke[J]. BMC Cardiovasc Disord, 2016, 16(1):209.
[12]" "JURKKO R, VÄNÄNEN H, MÄNTYNEN V, et al. High-resolution signal-averaged analysis of atrial electromagnetic characteristics in patients with paroxysmal lone atrial fibrillation[J]. Ann Noninvasive Electrocardiol, 2008, 13(4):378-385.
[13]" "NEMIROVSKY D, HUTTER R, GOMES J A. The electrical substrate of vagal atrial fibrillation as assessed by the signal-averaged electrocardiogram of the P wave[J]. Pacing Clin Electrophysiol, 2008, 31(3):308-313.
[14]" "ACAMPA M, LAZZERINI P E, GUIDERI F, et al. Electrocardiographic predictors of silent atrial fibrillation in cryptogenic stroke[J]. Heart Lung Circ, 2019, 28(11):1664-1669.
[15]" "RANGEL M O, O'NEAL W T, SOLIMAN E Z. Usefulness of the electrocardiographic P-wave axis as a predictor of atrial fibrillation[J]. Am J Cardiol, 2016, 117(1):100-104.
[16]" "CHUN K J, HWANG J K, PARK S J, et al. Electrical PR interval variation predicts new occurrence of atrial fibrillation in patients with frequent premature atrial contractions[J]. Medicine, 2016, 95(14):e3249.
[17]" "LEHTONEN A O, LANGÉN V L, PORTHAN K, et al. Electrocardiographic predictors of atrial fibrillation in nonhypertensive and hypertensive individuals[J]. J Hypertens, 2018, 36(9):1874-1881.
[18]" "BURAK C, YESIN M, TANIK V O, et al. Prolonged P wave peak time is associated with the severity of coronary artery disease in patients with non-ST segment elevation myocardial infarction[J]. J Electrocardiol, 2019, 55:138-143.
[19]" "YILDIZ Ï, ÖZMEN YILDIZ P, BURAK C, et al. P wave peak time for predicting an increased left atrial volume index in hemodialysis patients[J]. Med Princ Pract, 2020, 29(3):262-269.
[20]" "KIZILIRMAK F, DEMIR G G, GOKDENIZ T, et al. Changes in electrocardiographic P wave parameters after cryoballoon ablation and their association with atrial fibrillation recurrence[J]. Ann Noninvasive Electrocardiol, 2016, 21(6):580-587.
[21]" "SGRIGNA V, DELLA MONICA G, VILLANI M, et al. Automatic analysis of high resolution atrial activation in mitral valve stenosis[J]. Int J Cardiol, 1993, 42(1):63-70.
[22]" "ÖZ A, CINAR T, KIZILTO GÜLER C, et al. Novel electrocardiography parameter for paroxysmal atrial fibrillation in acute ischaemic stroke patients: P wave peak time[J]. Pos-tgrad Med J, 2020, 96(1140):584-588.
[23]" "黄赛银, 袁琳. 窦性P波变异的分析[J]. 中国实用医药, 2008, 3(26):72-73.
[24]" "KISHIMA H, MINE T, FUKUHARA E, et al. Is the abnormal conduction zone of the left atrium a precursor to a low voltage area in patients with atrial fibrillation?[J]. J Cardiovasc Electrophysiol, 2020, 31(11):2874-2882.
[收稿日期] 2024-03-23
