血小板相关参数对腹膜透析患者伴发焦虑、抑郁状态的诊断效能
2024-04-10刘辰玲朱静怡王琳琳高媛闫子毅王佳音刘圣君
刘辰玲 朱静怡 王琳琳 高媛 闫子毅 王佳音 刘圣君

基金项目:河北省政府资助省级临床医学优秀人才项目(ZF2024228)和河北省科技计划项目技术创新引导计划(20477750D)
摘要:目的 分析血小板相关参数与腹膜透析(PD)患者焦虑、抑郁发病的相关性,及其对PD患者伴发焦虑、抑郁状态的诊断效能。方法 选取2022年9月至2023年2月河北北方学院附属第一医院PD患者245例,采用广泛性焦虑量表(GAD-7)和患者健康问卷(PHQ-9)分别评估患者焦虑、抑郁情况。收集患者个人信息和生化指标,并检测血小板计数(PLT)、平均血小板体积(MPV)和血小板分布宽度(PDW),采用Logistic回归分析血小板相关参数与PD患者伴发焦虑、抑郁状态的关系。结果 245例PD患者中,焦虑发病率为15.9%,抑郁发病率为38.0%。患者透析龄(Z=-2.358,P=0.018;Z=-3.079,P=0.002)、MPV(Z=-4.953,P<0.001;Z=-7.878,P<0.001)、PDW(Z=-4.587,P<0.001;Z=-7.367,P<0.001)在焦虑组和无焦虑组、抑郁组和无抑郁组间差异均有统计学意义。相关性分析显示,MPV(r=0.358,P<0.001;r=0.489,P<0.001)、PDW(r=0.340,P<0.001;r=0.447,P<0.001)与PD患者伴发焦虑、抑郁状态具有正相关性。Logistic回归模型结果显示,MPV(P=0.022,P=0.011)、PDW(P=0.041,P=0.018)、透析龄(P=0.011,P=0.030)是PD患者伴发焦虑、抑郁状态的独立危险因素。MPV診断PD患者伴发焦虑、抑郁状态的受试者工作特征曲线下面积分别为0.750、0.800;PDW诊断PD患者伴发焦虑、抑郁状态的受试者工作特征曲线下面积分别为0.732、0.780。结论 MPV和PDW对PD伴发焦虑、抑郁状态具有较高的诊断效能,可作为评估PD患者伴发焦虑、抑郁状态的客观参考指标。
关键词:腹膜透析;焦虑;抑郁;平均血小板体积;血小板分布宽度;联合诊断效能
中图分类号: R692.5 文献标识码: A 文章编号:1000-503X(2024)01-0043-06
DOI:10.3881/j.issn.1000-503X.15731
Diagnostic Efficacy of Platelet-Related Parameters on Anxiety and Depression in Patients Undergoing Peritoneal Dialysis
LIU Chenling1,ZHU Jingyi1,WANG Linlin2,GAO Yuan1,YAN Ziyi1,WANG Jiayin1,LIU Shengjun2
1Graduate School,Hebei North University,Zhangjiakou,Hebei 075000,China
2Department of Nephrology,The First Affiliated Hospital of Hebei North University,Zhangjiakou,Hebei 075000,China
Corresponding author:LIU Shengjun Tel:0313-8041569,E-mail:15530396533@163.com
ABSTRACT:Objective To analyze the correlations between platelet-related parameters and the incidence of anxiety and depression in the patients undergoing peritoneal dialysis(PD),and evaluate the efficacy of the parameters in the diagnosis of anxiety and depression in PD patients.Methods A total of 245 patients undergoing PD in the First Affiliated Hospital of Hebei North University from September 2022 to February 2023 were enrolled.The generalized anxiety scale(GAD-7) and the patient health questionnaire(PHQ-9) were used to evaluate the anxiety and depression of the patients,respectively.The personal information and biochemical indicators of the patients were collected,and the platelet count(PLT),mean platelet volume(MPV),and platelet distribution width(PDW) were measured.Logistic regression was adopted to analyze the relationships of platelet-related parameters with anxiety and depression in PD patients.Results Among the 245 patients undergoing PD,the incidences of anxiety and depression were 15.9% and 38.0%,respectively.There were differences in the dialysis period(Z=-2.358,P=0.018;Z=-3.079,P=0.002),MPV(Z=-4.953,P<0.001;Z=-7.878,P<0.001),and PDW(Z=-4.587,P<0.001;Z=-7.367,P<0.001) between the anxiety group and the non-anxiety group as well as between the depression group and the non-depression group.The correlation analysis showed that MPV(r=0.358,P<0.001;r=0.489,P<0.001) and PDW(r=0.340,P<0.001;r=0.447,P<0.001) were positively correlated with anxiety and depression in the patients undergoing PD.The Logistic regression model showed that MPV(P=0.022,P=0.011),PDW(P=0.041,P=0.018),and dialysis period(P=0.011,P=0.030) were independent risk factors for the anxiety and depressive state in PD patients.The areas under the receiver operating characteristic curve of MPV in the diagnosis of anxiety and depression in PD patients were 0.750 and 0.800,respectively,and those of PDW were 0.732 and 0.780,respectively.Conclusion MPV and PDW have high efficacy in the diagnosis of anxiety and depression associated with PD and can be used as objective indicators to evaluate the anxiety and depression in the patients undergoing PD.
Key words:peritoneal dialysis;anxiety;depression;mean platelet volume;platelet distribution width;diagnostic efficacy of combined parameters
Acta Acad Med Sin,2024,46(1):43-48
慢性肾脏病(chronic kidney disease,CKD)的发病率逐年上升,已成为全球公共卫生问题之一[1-3]。截至2018年底我国登记存活的PD患者约86 264例[4]。腹膜透析(peritoneal dialysis,PD)治疗能在一定程度上改善CKD患者的生活质量,并延长生存期,但由于患者常合并多种并发症及躯体不适症状极易诱发焦虑、抑郁状态。Palmer等[5]研究发现CKD患者焦虑、抑郁的发病率是普通人群的5倍,且随着肾功能减退其发病率逐渐增加[6]。CKD患者的抑郁状态是不良临床结局的独立预测因素,及早发现并干预可提高患者对PD治疗的依从性[7]。但现有文献报道的CKD患者抑郁症的患病率差异较大,且在透析治疗情况下有可能被高估[5]。既往研究提示,焦虑、抑郁的发生与神经系统炎症反应[8-9]、5-羟色胺(5-hydroxytryptamine,5-HT)及脑源性神经营养因子缺乏密切相关[10-11]。脑源性神经营养因子储存于血小板(platelet,PLT)内,当PLT被激活时可将其释放到血液循环中,从而发挥调节神经元和神经胶质的生长发育及保护认知功能的作用[12-14]。PLT细胞膜上含有5-HT受体[15],激活的PLT还可以分泌促炎因子、抗炎因子及多种生物活性物质[16]。平均血小板体积(mean platelet volume,MPV)、血小板分布宽度(platelet distribution width,PDW)是评估PLT活性及功能的可靠指标。本研究旨在分析PLT相关参数与PD患者焦虑、抑郁发病的相关性,及其对PD患者伴发焦虑、抑郁状态的诊断效能,为PD患者不良情绪的早期识别提供客观的实验室检测指标。
1 对象和方法
1.1 对象
选取2022年9月至2023年2月河北北方学院附属第一医院PD门诊规律随访的PD患者,纳入标准:(1)符合CKD诊断标准[3];(2)年龄>18岁,透析龄6个月以上;(3)2个月内病情平稳,无住院、外伤或手术史;(4)使用传统的葡萄糖基乳酸缓冲透析液治疗,采用持续不卧床PD治疗方案;(5)无沟通障碍可以正确理解问卷内容。排除标准:(1)既往有精神疾病病史或精神疾病家族史;(2)器质性脑损伤病史;(3)血液系统疾病及急性感染期患者;(4)免疫系统疾病;(5)近3个月内输血史;(6)正在服用精神病类药物、镇静催眠药物、激素类药物或抗凝药物;(7)沟通障碍或对问卷内容不理解者。本研究为横断面研究,通过河北北方学院附属第一医院伦理委员会审批(伦理审查编号:W2023046),并获得所有患者的知情同意。
1.2 方法
采用广泛性焦虑量表(generalized anxiety disorder,GAD-7)評估患者焦虑状态,评分标准:0~4分为无焦虑,5~9分为轻度焦虑,10~14分为中度焦虑,15~21分为重度焦虑[17-18];采用患者健康问卷(patient health questionnaire,PHQ-9)评估患者抑郁状态,评分标准:0~4分为无抑郁,5~9分为轻度抑郁,10~14分为中度抑郁,15~19分为中重度抑郁,20~27分为重度抑郁[19]。
由经过培训的人员对患者进行问卷调查,采用统一的指导用语,问卷过程无家属及其他人员在场。问卷现场回收后由两名人员核对并进行评分。根据GAD-7评分结果,将患者分为焦虑组和无焦虑组;根据PHQ-9评分结果,将患者分为抑郁组和无抑郁组。对于符合纳入标准的患者次日空腹12 h后静脉采血,采用血小板分析仪PL-12对所有血液样本进行检测,记录PLT、MPV和PDW值。
1.3 观察指标
通过电子病历系统获取患者年龄、性别、受教育程度、婚姻状况、工作状况、体重指数(body mass index,BMI)、血尿素氮(blood urea nitrogen,BUN)、肌酐(creatinine,Cr)、肾小球滤过率(glomerular filtration rate,GFR)、内生肌酐清除率(creatinine clearance rate,Ccr)等指标。采用肾脏病饮食改良简化公式计算估算肾小球滤过率(estimated glomerular filtration rate,eGFR),采用Cockcroft-Gault公式计算Ccr[20-21]。分析观测指标与PD患者发生焦虑、抑郁状态的相关性,及其对PD患者伴发焦虑、抑郁状态的诊断效能。
1.4 统计学处理
采用SPSS 26.0统计软件,采用Kolmogorov-Smirnov对数据进行正态性检验,符合正态分布的连续性变量以均数±标准差表示,组间比较采用独立样本t检验;非正态分布的连续性变量以M(Q1,Q3)表示,组间比较采用Mann-Whitney U检验。分类变量和等级变量以例数和百分数表示,组间比较采用χ2检验。采用Spearman相关性分析观测指标与焦虑、抑郁的相关性,采用Logistic回归分析PD患者伴有焦虑、抑郁状态的独立危险因素。采用受试者工作特征(receiver operator characteristic,ROC)曲线描绘各独立危险因素的诊断效能及截断值,并计算曲线下面积(area under curve,AUC)。所有检验均为双侧检验,P<0.05为差异有统计学意义。
2 结果
2.1 一般资料
共纳入PD患者245例,其中,男124例(50.6%),女121例(49.4%),平均年龄(55.24±0.81)岁,焦虑发病率为15.9%,抑郁发病率为38.0%。焦虑组(n=39)和无焦虑组(n=206)患者透析龄(Z=-2.358,P=0.018)、MPV(Z=-4.953,P<0.001)、PDW(Z=-4.587,P<0.001)、Ccr(Z=-2.202,P=0.028)、GFR(Z=-1.968,P=0.049)、婚姻状况(χ2=5.232,P=0.022)差异均有统计学意义,而在年龄、性别、受教育程度、工作状况、BMI、PLT、BUN、Cr方面差异均无统计学意义(P均>0.05)。抑郁组(n=93)和无抑郁组(n=152)患者透析龄(Z=-3.079,P=0.002)、MPV(Z=-7.878,P<0.001)、PDW(Z=-7.367,P<0.001)、PLT(Z=-2.77,P=0.006)差异均有统计学意义,而在年龄、性别、婚姻状况、受教育程度、工作状况、BMI、BUN、Cr、Ccr、GFR方面差异均无统计学意义(P均>0.05)。
2.2 相关性分析结果
Spearman相关性分析结果显示,MPV(r=0.358,P<0.001)、PDW(r=0.340,P<0.001)与PD患者伴发焦虑状态具有正相关性;MPV(r=0.489,P<0.001)、PDW(r=0.447,P<0.001)与PD患者伴发抑郁状态具有正相关性。
2.3 回归分析结果
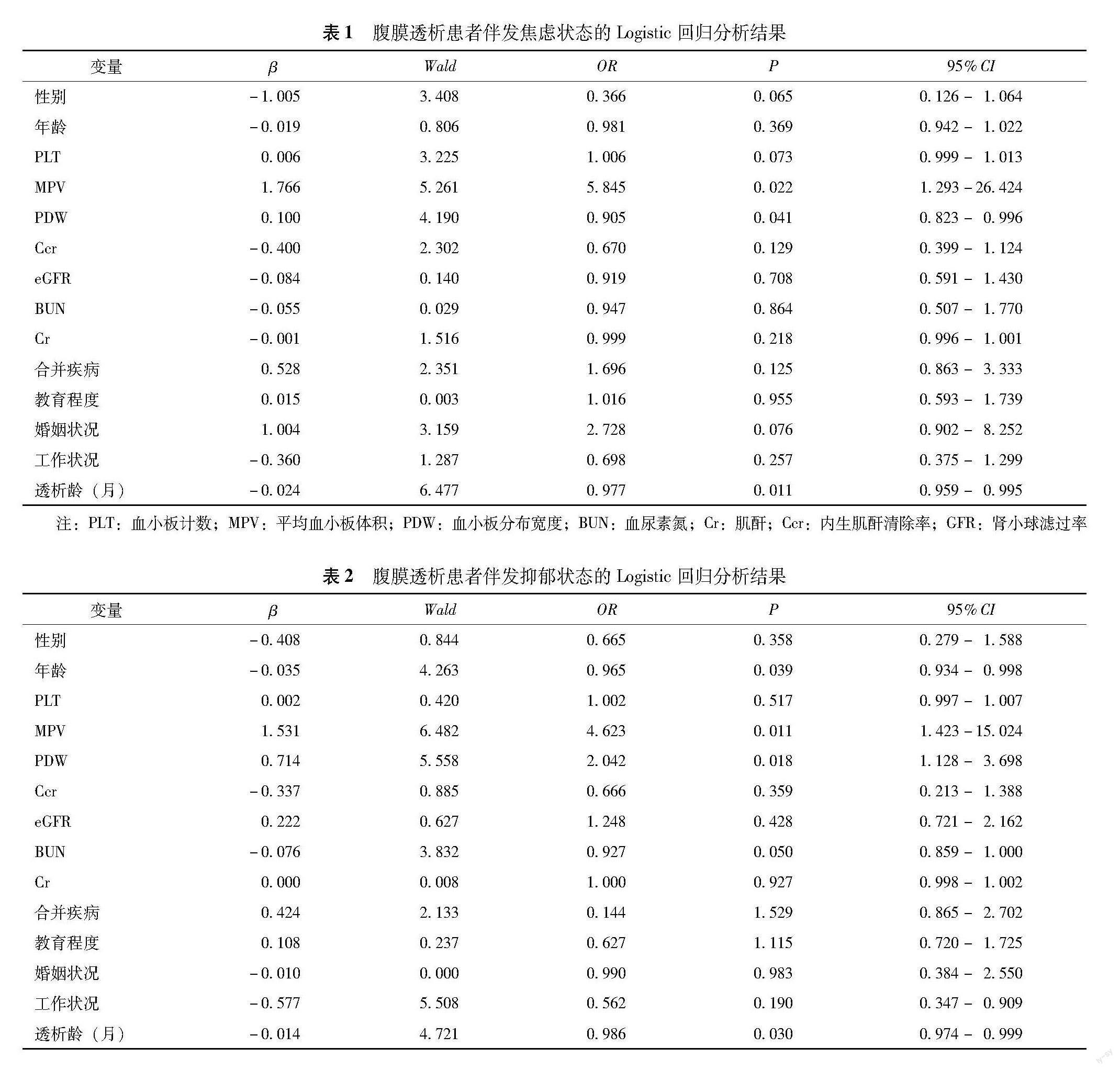
将焦虑作为因变量,以患者年龄、性别、PLT、MPV、PDW、BUN、Cr、eGFR、Ccr、合并疾病、教育程度、婚姻状况、工作状况和透析龄为自变量,纳入Logistic回归模型结果显示,MPV(OR=5.845,95%CI=1.293~26.424,P=0.022)、PDW(OR=0.905,95%CI=0.823~0.996,P=0.041)、透析龄(OR=0.977,95%CI=0.959~0.995,P=0.011)是PD患者伴发焦虑状态的独立危险因素(表1)。将抑郁作为因变量,以患者年龄、性别、PLT、MPV、PDW、BUN、Cr、eGFR、Ccr、合并疾病、教育程度、婚姻状况、工作状况和透析龄为自变量,纳入Logistic回归模型结果显示,MPV(OR=4.623,95%CI=1.423~15.024,P=0.011)、PDW(OR=2.042,95%CI=1.128~3.698,P=0.018)、透析龄(OR=0.986,95%CI=0.974~0.999,P=0.030)是PD患者伴发抑郁状态的独立危险因素(表2)。
2.4 诊断效能分析
ROC曲线分析显示,MPV诊断PD患者伴发焦虑状态的AUC为0.750(95%CI=0.661~0.839),当截断值为10.35时,灵敏度为64.1%,特异度为78.2%;PDW诊断PD患者伴发焦虑状态AUC为0.732(95%CI=0.641~0.822),当截断值为11.45时,灵敏度为
59.0%,特异度为79.6%;MPV和PDW聯合诊断效能的AUC为0.859(95%CI=0.793~0.925)(图1)。
MPV诊断PD患者伴发抑郁状态的AUC为0.800(95%CI=0.740~0.859),当截断值为10.15时,灵敏度为63.4%,特异度为84.2%;PDW诊断PD患者伴发抑郁状态AUC为0.780(95%CI=0.718~0.843),当截断值为10.85时,灵敏度为66.7%,特异度为81.6%;MPV和PDW联合诊断效能的AUC为0.870(95%CI=0.826~0.915)(图2)。
3 讨论
既往研究提示,5-HT是大脑内重要的单胺类神经递质,由色氨酸在肠道内经色氨酸羟化酶转化生成,通过5-HT转运体进入PLT内,储存在致密颗粒中[22]。PLT是体内5-HT主要转运载体和储存场所[23-25]。MPV和PDW作为评估PLT活性的特异性指标,其水平升高通常提示PLT功能更为活跃[26-27]。本研究通过分析PLT相关参数,发现MPV和PDW与PD患者伴发焦虑、抑郁状态呈显著正相关,且具有较高的诊断效能,与Fabian等[28]和Gialluisi等[29]的研究结果一致。Kokacya等[30]研究发现PLT活性的改变可以间接反映惊恐障碍患者中枢神经系统5-HT1A受体功能的异常状态。Canan等[31]研究证实MPV是一种有效的精神障碍生物标志物,在抑郁症患者中表现出更高的PLT活化水平。
本研究结果显示,MPV和PDW是PD患者伴发焦虑、抑郁状态的独立危险因素。ROC曲线分析表明,MPV和PDW对PD患者伴发焦虑、抑郁状态具有较高的诊断效能。这些易于获取的检测指标可为PD患者伴发不良情绪的临床早期识别提供客观指标参考,在一定程度上提高PD患者伴发焦虑、抑郁状态的早期就诊及临床诊断效率。此外,本研究单因素分析显示,透析龄在焦虑组和无焦虑组、抑郁组和无抑郁组间的差异有统计学意义,Logistic回归分析显示透析龄是PD患者伴发焦虑、抑郁状态的独立危险因素。随着透析龄的增加患者伴发焦虑、抑郁的可能性降低,这可能与适应性或逃避性心理反应有关[32]。
本研究存在一些局限性。首先,本研究为单中心横断面研究,因受区域和时间限制,只分析了PLT相关参数与PD患者伴发焦虑、抑郁状态的关系。其次,由于条件限制未能从分子生物学角度对相关机制进行更深层次的探究。
综上,本研究结果表明,MPV和PDW对PD伴发焦虑、抑郁状态具有较高的诊断效能,可作为评估PD患者伴发焦虑、抑郁状态的客观参考指标,为肾内科医师早期识别PD患者出现不良情绪提供便捷、有效的临床参考指标。
利益沖突 所有作者声明无利益冲突
作者贡献声明 刘辰玲、朱静怡:起草论文、收集整理并分析数据;王琳琳:指导修改论文;高媛、闫子毅、王佳音:数据收集;刘圣君:制定选题、设计实施研究
参 考 文 献
[1]Zhang L,Wang F,Wang L,et al.Prevalence of chronic kidney disease in China:a cross-sectional survey[J].Lancet,2012,379(9818):815-822.DOI:10.1016/S0140-6736(12)60033-6.
[2]Lv JC,Zhang LX.Prevalence and disease burden of chronic kidney disease[J].Adv Exp Med Biol,2019,1165:3-15.DOI:10.1007/978-981-13-8871-2_1.
[3]高翔,梅长林.慢性肾脏病早期筛查、诊断及防治指南(2022年版)解读[J].中国实用内科杂志,2022,42(9):735-738.DOI:10.19538/j.nk2022090108.
[4]倪兆慧,金海娇.中国腹膜透析发展70年[J].中国血液净化,2019,10(18):661-663.DOI:10.3969/j.issn.1671-4091.2019.10.001.
[5]Palmer S,Vecchio M,Craig JC,et al.Prevalence of depression in chronic kidney disease:systematic review and meta-analysis of observational studies[J].Kidney Int,2013,84(1):179-191.DOI:10.1038/ki.2013.77.
[6]Zhang Z,He P,Liu M,et al.Association of depressive symptoms with rapid kidney function decline in adults with normal kidney function[J].Clin J Am Soc Nephrol,2021,16(6):889-897.DOI:10.2215/CJN.18441120.
[7]Tsai YC,Chiu YW,Hung CC,et al.Association of symptoms of depression with progression of CKD[J].Am J Kidney Dis,2012,60(1):54-61.DOI:10.1053/j.ajkd.2012.02.325.
[8]Zhang MM,Guo MX,Zhang QP,et al.IL-1R/C3aR signaling regulates synaptic pruning in the prefrontal cortex of depression[J].Cell Biosci,2022,12(1):90.DOI:10.1186/s13578-022-00832-4.
[9]Beurel E,Toups M,Nemeroff CB.The bidirectional relationship of depression and inflammation:double trouble[J].Neuron,2020,107(2):234-256.DOI:10.1016/j.neuron.2020.06.002.
[10]Turner EH,Loftis JM,Blackwell AD.Serotonin a la carte:supplementation with the serotonin precursor 5-hydroxytryptophan[J].Pharmacol Ther,2006,109(3):325-338.DOI:10.1016/j.pharmthera.2005.06.004.
[11]Lee BH,Kim YK.Reduced platelet BDNF level in patients with major depression[J].Prog Neuropsychopharmacol Biol Psychiatry,2009,33(5):849-853.DOI:10.1016/j.pnpbp.2009.04.002.
[12]Le Blanc J,Fleury S,Boukhatem I,et al.Platelets selectively regulate the release of BDNF,but not that of its precursor protein,proBDNF[J].Front Immunol,2020,11:575607.DOI:10.3389/fimmu.2020.575607.
[13]Kowianski P,Lietzau G,Czuba E,et al.BNDF:a key factor with multipotent impact on brain signaling and synaptic plasticity[J].Cell Mol Neurobiol,2018,38(3):579-593.DOI:10.1007/s10571-017-0510-4.
[14]Gibon J,Barker PA.Neurotrophins and proneurotrophins:focus on synaptic activity and plasticity in the brain[J].Neuroscientist,2017,23(6):587-604.DOI:10.1177/1073858417697037.
[15]Stratz C,Trenk D,Bhatia HS,et al.Identification of 5-HT3 receptors on human platelets:increased surface immunoreactivity after activation with adenosine diphosphate(ADP) and thrombin receptor-activating peptide(TRAP)[J].Thromb Haemost,2008,99(4):784-786.DOI:10.1160/TH07-10-0630.
[16]Golebiewska EM,Poole AW.Platelet secretion:from haemostasis to wound healing and beyond[J].Blood Rev,2015,29(3):153-162.DOI:10.1016/j.blre.2014.10.003.
[17]Spitzer RL,Kroenke K,Williams JB,et al.A brief measure for assessing generalized anxiety disorder:the GAD-7[J].Arch Intern Med,2006,166(10):1092-1097.DOI:10.1001/archinte.166.10.1092.
[18]Kroenke K,Spitzer RL,Williams JB,et al.Anxiety disorders in primary care:prevalence,impairment,comorbidity,and detection[J].Ann Intern Med,2007,146(5):317-325.DOI:10.7326/0003-4819-146-5-200703060-00004.
[19] Kroenke K,Spitzer RL,Williams JB.The PHQ-9:validity of a brief depression severity measure[J].J Gen Intern Med,2001,16(9):606-613.DOI:10.1046/j.1525-1497.2001.016009606.x.
[20]Levey AS,Bosch JP,Lewis JB,et al.A more accurate method to estimate glomerular filtration rate from serum creatinine:a new prediction equation.Modification of Diet in Renal Disease Study Group[J].Ann Intern Med,1999,130(6):461-470.DOI:10.7326/0003-4819-130-6-199903160-00002.
[21]陳文彬,潘祥林,康熙雄,等.诊断学[M].第7版.北京:人民卫生出版社,2008:78-81.
[22]Ayme-Dietrich E,Aubertin-Kirch G,Maroteaux L,et al.Cardiovascular remodeling and the peripheral serotonergic system[J].Arch Cardiovasc Dis,2017,110(1):51-59.DOI:10.1016/j.acvd.2016.08.002.
[23]Gialluisi A,Izzi B,Di Castelnuovo A,et al.Revisiting the link between platelets and depression through genetic epidemiology:new insights from platelet distribution width[J].Haematologica,2020,105(5):e246-e248.DOI:10.3324/haematol.2019.222513.
[24]Lv J,Liu F.The role of serotonin beyond the central nervous system during embryogenesis[J].Front Cell Neurosci,2017,11:74.DOI:10.3389/fncel.2017.00074.
[25]Ye JY,Liang EY,Cheng YS,et al.Serotonin enhances megakaryopoiesis and proplatelet formation via p-Erk1/2 and F-actin reorganization[J].Stem Cells,2014,32(11):2973-2982.DOI:10.1002/stem.1777.
[26]Slavka G,Perkmann T,Haslacher H,et al.Mean platelet volume may represent a predictive parameter for overall vascular mortality and ischemic heart disease[J].Arterioscler Thromb Vasc Biol,2011,31(5):1215-1218.DOI:10.1161/ATVBAHA.110.221788.
[27]De Luca G,Venegoni L,Iorio S,et al.Platelet distribution width and the extent of coronary artery disease:results from a large prospective study[J].Platelets,2010,21(7):508-514.DOI:10.3109/09537104.2010.494743.
[28]Fabian B,Horvath IF,Shemirani AH,et al.Depression and anxiety symptoms are associated with mean platelet volume in autoimmune disorders[J].Int J Environ Res Public Health,2022,19(17):11006.DOI:10.3390/ijerph191711006.
[29]Gialluisi A,Bonaccio M,Di Castelnuovo A,et al.Lifestyle and biological factors influence the relationship between mental health and low-grade inflammation[J].Brain Behav Immun,2020,85:4-13.DOI:10.1016/j.bbi.2019.04.041.
[30]Kokacya MH,Copoglu US,Kivrak Y,et al.Increased mean platelet volume in patients with panic disorder[J].Neuropsychiatr Dis Treat,2015,11:2629-2633.DOI:10.2147/NDT.S94147.
[31]Canan F,Dikici S,Kutlucan A,et al.Association of mean platelet volume with DSM-IV major depression in a large community-based population:the MELEN study[J].J Psychiatr Res,2012,46(3):298-302.DOI:10.1016/j.jpsychires.2011.11.016.
[32]Segerstrom SC,Smith GT.Personality and coping:individual differences in responses to emotion[J].Annu Rev Psychol,2019,70:651-671.DOI:10.1146/annurev-psych-010418-102917.
(收稿日期:2023-06-19)
