Different timing for abdominal paracentesis catheter placement and drainage in severe acute pancreatitis complicated by intraabdominal fluid accumulation
2024-03-07RuiChenHuaQiangChenRuiDieLiHuiMinLu
Rui Chen,Hua-Qiang Chen,Rui-Die Li,Hui-Min Lu
Abstract BACKGROUND Non-surgical methods such as percutaneous drainage are crucial for the treatment of patients with severe acute pancreatitis (SAP).However,there is still an ongoing debate regarding the optimal timing for abdominal paracentesis catheter placement and drainage.AIM To explore the influence of different timing for abdominal paracentesis catheter placement and drainage in SAP complicated by intra-abdominal fluid accumulation.METHODS Using a retrospective approach,184 cases of SAP complicated by intra-abdominal fluid accumulation were enrolled and categorized into three groups based on the timing of catheter placement: group A (catheter placement within 2 d of symptom onset,n=89),group B (catheter placement between days 3 and 5 after symptom onset,n=55),and group C (catheter placement between days 6 and 7 after symptom onset,n=40).The differences in progression rate,mortality rate,and the number of cases with organ dysfunction were compared among the three groups.RESULTS The progression rate of group A was significantly lower than those in groups B and groups C (2.25% vs 21.82% and 32.50%,P < 0.05).Further,the proportion of patients with at least one organ dysfunction in group A was significantly lower than those in groups B and groups C (41.57% vs 70.91% and 75.00%,P < 0.05).The mortality rates in group A,group B,and group C were similar (P > 0.05).At postoperative day 3,the levels of C-reactive protein (55.41 ± 19.32 mg/L vs 82.25 ± 20.41 mg/L and 88.65 ± 19.14 mg/L,P < 0.05),procalcitonin (1.36 ± 0.51 ng/mL vs 3.20 ± 0.97 ng/mL and 3.41 ± 0.98 ng/mL,P < 0.05),tumor necrosis factor-alpha (15.12 ± 6.63 pg/L vs 22.26 ± 9.96 pg/L and 23.39 ± 9.12 pg/L,P < 0.05),interleukin-6 (332.14 ± 90.16 ng/L vs 412.20 ± 88.50 ng/L and 420.08 ± 87.65ng/L,P < 0.05),interleukin-8 (415.54 ± 68.43 ng/L vs 505.80 ± 66.90 ng/L and 510.43 ± 68.23ng/L,P < 0.05) and serum amyloid A (270.06 ± 78.49 mg/L vs 344.41 ± 81.96 mg/L and 350.60 ± 80.42 mg/L,P < 0.05) were significantly lower in group A compared to those in groups B and group C.The length of hospital stay in group A was significantly lower than those in groups B and group C (24.50 ± 4.16 d vs 35.54 ± 6.62 d and 38.89 ± 7.10 d,P < 0.05).The hospitalization expenses in group A were also significantly lower than those in groups B and groups C [2.70 (1.20,3.55) ten-thousand-yuan vs 5.50 (2.98,7.12) ten-thousand-yuan and 6.00 (3.10,8.05) ten-thousand-yuan,P < 0.05).The incidence of complications in group A was markedly lower than that in group C (5.62% vs 25.00%,P < 0.05),and similar to group B (P > 0.05).CONCLUSION Percutaneous catheter drainage for the treatment of SAP complicated by intra-abdominal fluid accumulation is most effective when performed within 2 d of onset.
Key Words: Abdominal paracentesis catheter drainage;Timing;Severe acute pancreatitis;Intra-abdominal fluid;Application value
lNTRODUCTlON
Acute pancreatitis is typically caused by the abnormal activation of digestive enzymes within the pancreas.Under normal circumstances,the pancreas secretes digestive enzymes,which are activated before entering the small intestine to help break down fats,proteins,and carbohydrates in food[1].However,in patients with acute pancreatitis,these digestive enzymes undergo abnormal activation within the pancreas.This leads to the digestion of pancreatic tissue itself and can trigger a series of inflammatory reactions that rapidly spread to surrounding tissues and organs.This cascade of events can result in the occurrence of systemic inflammatory response syndrome and,in severe cases,can lead to organ failure and patient death[2].According to global statistics,the annual incidence of acute pancreatitis falls between 13 to 45 cases per 100000 people,with approximately 15% of patients progressing to severe acute pancreatitis (SAP)[3].SAP,as a severe form of acute pancreatitis,is characterized by rapid progression,a higher incidence of complications,and a higher mortality rate,necessitating urgent medical intervention and treatment[4].While minimally invasive surgery can effectively remove necrotic tissue in SAP,it can be challenging to completely clear necrotic tissue during the early stages of SAP due to the difficulty in accurately distinguishing between normal and necrotic pancreatic tissue.This can affect the surgical outcome[5].Therefore,in order to effectively control infection in patients and avoid surgical risks,non-surgical methods such as percutaneous drainage are crucial for the treatment of patients with SAP.However,there is still ongoing debate regarding the optimal timing for abdominal paracentesis catheter placement and drainage.Given this background,the aim of the present study was to explore the application value of different timing for abdominal paracentesis catheter placement and drainage in SAP complicated by intra-abdominal fluid accumulation.This study aims to provide more precise guidance for clinicians,optimizing treatment strategies,and improving the quality of life for SAP patients.
MATERlALS AND METHODS
Basic data of the study subjects
Using a retrospective research method,a total of 184 patients with SAP complicated by intra-abdominal fluid accumulation treated at our hospital from August 2022 to July 2023 were enrolled in this study.Inclusion criteria: (1) Diagnosis of SAP in accordance with the criteria outlined in the "Chinese Guidelines for the Diagnosis and Treatment of Acute Pancreatitis"[6],confirmed through imaging studies such as computed tomography with pelvic/abdominal fluid accumulation of ≥ 100 mL;(2) admission to the hospital within 72 h of symptom onset;(3) adult patients;(4) underwent abdominal paracentesis catheter placement and drainage;and (5) completely available of clinical data.The exclusion criteria were: (1) Patients with a history of abdominal surgery;(2) a history of chronic pancreatitis;(3) secondary acute pancreatitis caused by drugs,surgery,and malignant tumors;and (4) concurrent blood system diseases,infectious diseases,and other serious diseases.Patients were divided into different groups according the puncture time point,as follows: Group A (puncture ≤ 2 d),group B (puncture 3-5 d),and group C (puncture 6-7 d),with 89,55,and 40 cases,respectively.
Treatment methods
All patients underwent abdominal paracentesis catheter drainage (APD).Puncture procedure: An ultrasound device was used to scan the patient's abdomen to determine the location and optimal puncture point for intra-abdominal fluid.Then,local infiltration anesthesia was applied using 4% lidocaine around the puncture site.The operator then employed the Seldinger technique to complete the puncture and utilized an 8 F catheter (from Shenzhen Cooper Business Trading Co.,Ltd.) for drainage.A sterile drainage bag was connected to ensure unobstructed drainage.After 3 to 5 d of drainage,another abdominal ultrasound examination was performed to assess the status of intra-abdominal fluid.If the ultrasound suggested that intra-abdominal fluid was still present,the catheter was replaced with a larger diameter catheter to improve drainage efficiency.
Criteria for catheter removal: The drainage catheters were removed when the patient's symptoms and signs significantly improved,and the drainage volume gradually decreased to less than 10 mL continuously for ≥ 2 d,and abdominal ultrasound examination does not detect residual fluid.
Step-up therapy for SAP: When SAP patients experienced worsening symptoms,increased organ failure,or the presence of free gas around the pancreas despite initial treatment with APD,ultrasound-guided percutaneous catheter drainage (PCD) was considered.If the patient's condition did not significantly improve after PCD treatment,and symptoms continue to worsen with no improvement in organ failure,further intervention with endoscopic necrosectomy may be necessary.
Check methods
Before and after treatment,3 mL of peripheral fasting venous blood was collected from the patients.After centrifugation at a speed of 3600 revolutions per minute for 12 min,enzyme-linked immunosorbent assays with reagent kits from R and D Systems were used to detect interleukin-6 (IL-6) and interleukin-8 (IL-8).Procalcitonin (PCT),C-reactive protein (CRP),and tumor necrosis factor-alpha (TNF-α) were detected using electrochemiluminescence assays,with reagent kits from Roche Diagnostics.Serum amyloid A (SAA) was measured using the scattering turbidity method,with reagent kits from Beckman Coulter.
Observation indicators
The advanced rate (calculated as advanced cases/total cases × 100%,with advanced cases defined as patients who underwent PCD within 4 wk of hospitalization according to the ascending ladder treatment plan),mortality,organ failure,hospitalization time and hospitalization expenses,as well as serum CRP,PCT,TNF-α,IL-6,IL-8 and SAA levels before and after treatment were collected.
Statistical processing
SPSS 22.0 software was used for all analyses.Normally distributed quantitative data are expressed as (mean ± SD),while non-normally quantitative distributed data are expressed as M (Q25,Q75).Count data are represented asn(%).For intergroup comparisons,analysis of variance,the Mann-Whitney U test,orχ2test is employed.The significance level was set at α=0.05.
RESULTS
Comparison of general clinical data among the patient groups
Gender,age,acute physiology and chronic health evaluation II score at admission,and etiology showed no significant differences between groups A,B,and C (P> 0.05,Table 1)

Table 1 Comparison of general clinical data among the groups of patients
Comparison of progression rate,mortality rate,and organ dysfunction among the groups
The rate of progression to organ failure and the proportion of patients with ≥ 1 organ dysfunction in group A was significantly lower than those in groups B and C (P< 0.05).The rates of progression and the proportion of patients with ≥ 1 organ dysfunction were comparable between groups B and C (P> 0.05).The mortality rates were comparable between all the groups (P> 0.05).These results are summarized in Table 2.

Table 2 Comparison of progression rate,mortality rate,and organ dysfunction among the groups
Comparison of serum indicators among the groups
At 3 d post-operation,the CRP,PCT,TNF-a,IL-6,IL-8,and SAA levels in groups A,B,and C significantly decreased compared to pre-operation (P< 0.05).However,the levels of CRP,PCT,TNF-α,IL-6,IL-8,and SAA in group A were significantly lower than those in groups B and C at this timepoint (P< 0.05).There was no significant difference in the levels of CRP,PCT,TNF-α,IL-6,IL-8,and SAA between groups B and C (P> 0.05).Results are presented in Table 3.
Comparison of length of hospital stay and hospitalization costs among the groups
The length of hospital stay and hospitalization costs in group A were both significantly lower than in groups B and C (P< 0.05).The length of hospital stay and hospitalization costs were similar between groups B and C (P> 0.05).The results are presented in Table 4.
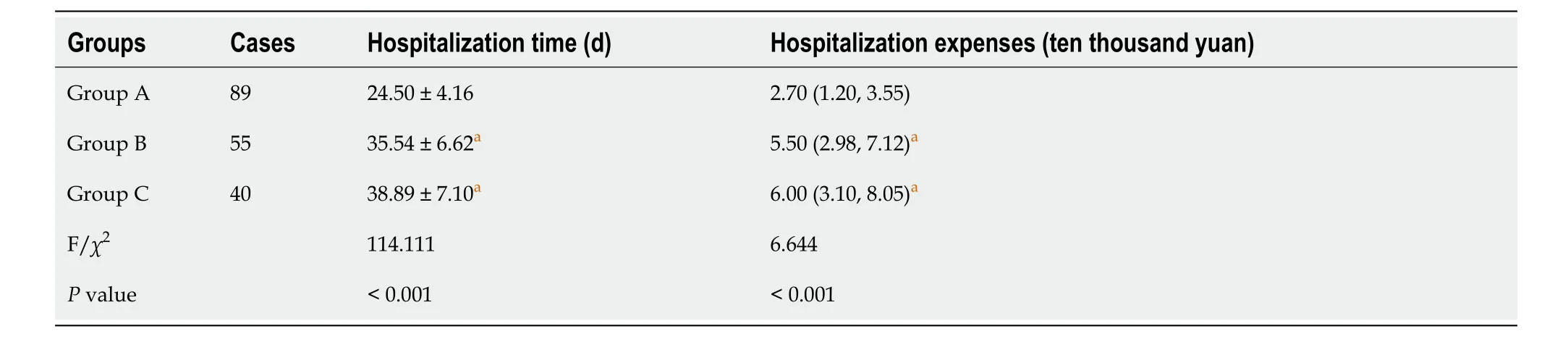
Table 4 Comparison of length of hospital stay and hospitalization costs among the groups
Comparison of complications among the groups
The complication rate in group A was significantly lower than that in group C (P< 0.05),and similar to that group B (P> 0.05).The complication rates were similar between group B and group C (P> 0.05) (Table 5).

Table 5 Comparison of complications among the groups
DlSCUSSlON
Acute pancreatitis is a disease characterized by acute inflammation of the pancreatic tissue,and within it,SAP represents an extreme manifestation of acute pancreatitis[7-9].SAP is a critical condition often associated with widespread inflammation of the pancreas and surrounding tissues.Additionally,the release of inflammatory factors triggers a severe systemic inflammatory response,leading to multi-organ dysfunction,including the cardiovascular system,respiratory system,and kidneys[10-12].In the early stages of SAP (within the first 24 h after onset),patients often exhibit a phenomenon known as pancreatitis-associated ascitic fluid (PAAF).This is primarily due to increased capillary permeability around the pancreas caused by inflammation and cellular damage.This increased permeability leads to the leakage of fluid from blood vessels into the surrounding tissues,resulting in the formation of ascitic fluid within the abdominal cavity[13-15].Through abdominal ultrasound examination,the accumulation of fluid within the abdominal cavity,known as abdominal ascites,can be clearly observed.In this situation,PCD serves as a direct and rapid therapeutic approach,effectively removing the accumulated PAAF from the abdominal cavity.This helps reduce intraabdominal pressure,prevent further exacerbation of the inflammatory response,and decrease the occurrence of complications[16-18].While this treatment strategy can effectively prevent the pathological and physiological damage caused by PAAF,thereby aiding in controlling the severity of SAP and improving patient survival rates,the optimal timing for abdominal puncture remains a subject of debate and a focus of clinical research and discussion[19-21].Therefore,there is a need for a systematic study to investigate the impact of different timing for PCD on the treatment outcomes and prognosis of patients with SAP complicated by abdominal ascites.
This study's findings indicated that group A had a significantly lower rate of progression and a lower proportion of patients with ≥ 1 organ dysfunction compared to group B and group C.However,there was no significant difference in the mortality rates among group A,group B,and group C.This suggested that early puncture drainage (group A) can significantly reduce the risk of progression and organ dysfunction,whereas there was no significant difference in progression and organ dysfunction rates between the groups with later puncture drainage (group B and group C).
However,performing puncture drainage at different time points did not have a significant impact on mortality rates.This study conducted further comparative analysis of inflammatory markers among the three groups of patients.The results showed that,postoperatively,CRP,PCT,TNF-α,IL-6,IL-8,and SAA levels significantly decreased compared to preoperative levels in all three groups.However,the reduction in inflammatory markers in group A was significantly greater than that in groups B and C.This suggests that early abdominal puncture drainage (within 2 d of onset) can more effectively clear inflammatory mediators,reduce organ damage,and prevent the progression of the condition.
The reason for this analysis is that PAAF contains a significant amount of toxic substances such as amylase,endotoxins,pancreatic proenzyme activation peptide,pancreatic enzymes,and free fatty acids.These toxic substances can exacerbate the body's inflammatory response,leading to the release of a series of inflammatory factors such as CRP,PCT,IL-6,etc.,resulting in an increase in their serum concentrations[21-24].This implies that PAAF directly promotes the deterioration of the condition in SAP patients.Therefore,for these patients,early abdominal puncture drainage (within 2 d of admission) is crucial.This can rapidly clear harmful substances from the abdominal cavity,alleviate the inflammatory response in SAP,reduce the serum concentrations of various inflammatory factors,and consequently lower the risk of organ dysfunction[25-27].Comparing the APD performed in groups A,B,and C,this study found that group A hadbetter drainage effectiveness.This is because the earlier drainage is performed,the more effectively toxic and harmful substances can be cleared,thereby reducing the inflammatory response,slowing down,or even halting the progression of SAP[28-30].Therefore,compared to patients who undergo drainage later,those who receive early drainage have a lower progression rate,indicating that their disease is less likely to worsen,leading to better clinical outcomes[31-33].
This study's results indicate that in the treatment of patients with SAP complicated by abdominal ascites,early puncture drainage (group A) significantly reduces hospitalization time and costs.Additionally,it demonstrates a significant advantage in terms of complication rates compared to later drainage.This suggests that choosing early puncture drainage can improve patients' hospitalization conditions and treatment outcomes,reducing the occurrence of complications,and simultaneously lowering healthcare costs.This further highlights the importance and advantages of early puncture drainage in the management of SAP complicated by abdominal ascites[34,35].
This study has several limitations that should be mentioned.Firstly,the retrospective study design and limited sample size in each group may have introduced bias and limit the generalizability of the results.Further,the time of catheter placement was only divided into 3 categories.Thus,the results of this study need to be confirmed by further prospective study with large cohort.
CONCLUSlON
When treating patients with SAP complicated by abdominal ascites through abdominal puncture catheter drainage,2 d after disease onset is the optimal treatment time window to perform drainage.
ARTlCLE HlGHLlGHTS
Research background
Severe acute pancreatitis (SAP),a severe form of acute pancreatitis,is characterized by rapid progression,a high incidence of complications,and a high mortality rate among patients.It necessitates urgent medical intervention and treatment.While minimally invasive surgery can effectively remove necrotic tissue in SAP,it can be challenging to completely clear necrotic tissue during the early stages of SAP due to the difficulty in accurately distinguishing between normal and necrotic pancreatic tissue.
Research motivation
Non-surgical methods such as percutaneous drainage are crucial for the treatment of patients with SAP.However,there is still ongoing debate regarding the optimal timing for abdominal paracentesis catheter placement and drainage.
Research objectives
The aim of this study was to explore the application value of different timing for abdominal paracentesis catheter placement and drainage in SAP complicated by intra-abdominal fluid accumulation.This study aims to provide more precise guidance for clinicians,optimizing treatment strategies,and improving the quality of life for SAP patients.
Research methods
Through a retrospective study design,184 cases of SAP complicated by intra-abdominal fluid accumulation were selected from patients treated at our hospital from August 2022 to July 2023.These cases were categorized into three groups based on the timing of catheter placement: Group A (catheter placement within 2 d of symptom onset,n=89),group B (catheter placement between days 3 and 5 after symptom onset,n=55),and group C (catheter placement between days 6 and 7 after symptom onset,n=40).Differences in progression rate,mortality rate,and the number of cases with organ dysfunction were then compared between the three groups.
Research results
The progression rate and proportion of patients with at least one organ dysfunction in group A was significantly lower than those in group B and group C.At postoperative day 3,the levels of C-reactive protein,procalcitonin,tumor necrosis factor-alpha,interleukin-6,interleukin-8,and serum amyloid A were significantly lower in group A compared with those observed in groups B and C.The length of hospital stay and hospitalization expenses in group A were also significantly lower than those in groups B and C.The incidence of complications in group A was markedly lower than that in group C,and similar to group B (P> 0.05).
Research conclusions
Percutaneous catheter drainage for the treatment of SAP complicated by intra-abdominal fluid accumulation is more effective when performed within 2 d of onset.
Research perspectives
Prospective study with large cohort is required.
FOOTNOTES
Author contributions:Chen R,Chen HQ,Li RD,and Lu HM designed the research study;Chen R and Chen HQ performed the research;Li RD contributed new reagents and analytic tools;Chen R,Li RD and Lu HM analyzed the data and wrote the manuscript;all authors have read and approve the final manuscript.
lnstitutional review board statement:The study was reviewed and approved by the Ethics Committee of Chengdu No.6 People's Hospital.
lnformed consent statement:As the study used anonymous and pre-existing data,the requirement for the informed consent from patients was waived.
Conflict-of-interest statement:We have no financial relationships to disclose.
Data sharing statement:Technical appendix,statistical code,and dataset available from the corresponding author.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Rui Chen 0009-0009-9029-0964;Hui-Min Lu 0000-0002-5759-1919.
S-Editor:Qu XL
L-Editor:A
P-Editor:Qu XL
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Prospects in the application of ultrasensitive chromosomal aneuploidy detection in precancerous lesions of gastric cancer
- Prognostic value of ultrasound in early arterial complications post liver transplant
- Added value of ratio of cross diameters of the appendix in ultrasound diagnosis of acute appendicitis
- Single-incision laparoscopic transabdominal preperitoneal repair in the treatment of adult female patients with inguinal hernia
- Predictive value of machine learning models for lymph node metastasis in gastric cancer: A two-center study
- Micro-power negative pressure wound technique reduces risk of incision infection following loop ileostomy closure
