Associations among frailty status,hypertension,and fall risk in community-dwelling older adults
2024-02-27LipingTengDnhuiWngZhouZhouJunSunMinZhuRenrongWng
Liping Teng ,Dnhui Wng ,b ,Zhou Zhou ,Jun Sun ,Min Zhu ,Renrong Wng
aWuxi School of Medicine,Jiangnan University,Wuxi,Jiangsu,China
b Traditional Chinese Medicine Hospital of Qinghai Province,Xining,Qinghai,China
cDepartment of Cardiology,Jiangnan University Medical Center,Wuxi,Jiangsu,China
Keywords:
ABSTRACT Objectives: Frailty and hypertension often coexist in older adults,which may lead to fall risks.This study aimed to examine the relationship between frailty status,hypertension,and fall risk.Methods:In this cross-sectional study,a total of 401 older adults were conveniently recruited from communities in Wuxi,China,between September 2022 and November 2022.The fall risk self-assessment checklist from the Stopping Elderly Accidents,Deaths &Injuries (STEADI) Toolkit was used to evaluate their fall risks.The FRAIL scale questionnaire was used to assess frailty status.Participants’demographic information and comorbidities were collected.Multivariate logistic regression,generalized additive model,and smooth curve fitting were used to analyze the association between frailty,hypertension,and fall risk.Results:Frailty had a strong association with increased prevalence of fall risk among the participants(OR 8.52,95%CI 3.21-22.57;P <0.001).Hypertension significantly increased the fall risk among older adults(OR 1.87,95% CI 1.11-3.13;P=0.019).The group with hypertension and frailty had the highest prevalence of fall risk (OR 12.24,95% CI 3.51-42.65).Smooth curve fitting showed a nonlinear association between frailty and fall risk in hypertension status.In the progress of pre-frailty to frailty status,a higher tendency to fall was found among older adults with hypertension.Conclusions:Frailty status and hypertension independently and jointly influenced the increased prevalence of fall risk.Enhanced frailty and hypertension management may help decrease fall risk among this population.
What is known?
· Frailty and hypertension often coexist in older adults,which may lead to falls.
· Frailty is closely related to hypertension.
· Older adults with hypertension are more likely to have fall risk.
· Frailty has been confirmed to be related to more fall events in older adults.
What is new?
· Older adults with hypertension and frailty had a higher fall risk compared with those without these conditions.
· There was a nonlinear association between frailty and fall risk in adults with hypertension.
· Older adults with hypertension had a higher tendency to fall in the progress of pre-frailty to frailty status.
1.Introduction
Aging is the general trend of global population development.The proportion of the world’s population aged 65 years and over exceeded 7% in 2002 and reached 10% in 2022,thus posing severe challenges to society.China is one of the fastest-aging countries,and by 2050,the population over 65 years is expected to account for 30% of the total national population [1].Due to increased attention and interest,frailty in older adults has become a hot topic.Frailty is generally defined as losing reserves,leading to increased vulnerability to adverse health outcomes [2].Many studies have confirmed that frailty is closely related to cardiovascular diseases such as hypertension [3].
In China,more than 50%of older adults have hypertension,and the prevalence of hypertension in people aged 80 years and over reached 90% [4].Older adults with hypertension have significant blood pressure fluctuations and high heterogeneity,resulting in differences in their frailty status [5].In the treatment of frail older adults with hypertension,blood pressure within normal limits is overemphasized,leading to the growing risk of falls [6,7].Therefore,evaluating the overall status of the frail older adults with hypertension is prioritized [8].Furthermore,older adults with hypertension were nearly seven times more likely to have fall risk than those who do not have hypertension [9].Adults experience decreased body function in aging,quickly leading to falls and frailty [10].About 30% and 50% of older adults over 65 and 80 years experienced a fall yearly,respectively [11],which is the leading cause of injury and heavy economic burden [12].In a 12-year longitudinal study in Korea,frailty was confirmed to be related to more fall events in older adults[13],suggesting that the two components of frailty,namely,social isolation and exhaustion,are independently associated with fall risk.Similarly,frailty was proven to be a risk factor for falls and fractures in community-dwelling participants aged 75 years or older [14].
Previous studies showed the relationship between frailty,falls,and orthostatic hypotension in long-term care facilities [15].They indicated that older adults with frailty and impaired orthostatic blood pressure control had a higher fall risk.However,the correlation between fall risk and the frailty score of older adults with hypertension remains unclear.In the present study,the interrelationship among various frailty statuses,hypertension,and fall risk was explored for enhanced intervention to reduce fall risk in older adults with frailty and hypertension.
2.Participants and methods
2.1.Study design and sample
This study was a cross-sectional study.The sample size was calculated using the following formula: n=Z2P (1-P)/δ2,using a confidence level of 0.95 (Z=1.96),a fall risk prevalence of 27.5%(P=27.5%) [16],and a permissible error (δ) of 0.0495 (δ=0.18 P).We calculated the minimum sample size is 313.
2.2.Participants and recruitment
Community-dwelling adults aged ≥60 were recruited between September 2022 and November 2022 in Wuxi,Jiangsu Province,China.There are five districts with 590 communities in Wuxi.In this study,two communities from each district were conveniently chosen.A total of 10 communities were included.The participants from these communities were recruited by convenience sampling.Banners and posters were put up in public places in the community to reach respondents interested in this study.All participants were 60 years old and over,and those with advanced dementia,hearing and communication disorders,severe mental disorders,and terminal illness were excluded.Well-trained researchers identified interested respondents using established inclusion and exclusion criteria.Trained researchers conducted in-person interviews with enrolled participants in the community healthcare center or their homes after obtaining informed consent.A total of 401 participants were recruited from the community-dwelling older people,surpassing the calculated minimum sample size of 313.
2.3.Variables and measures
2.3.1.Demographic characteristics
In this study,demographic information was collected,including age,gender,marital status,education level,per capita monthly income of households,smoking history (yes/no),drinking history(yes/no),polypharmacy (yes/no),and comorbidities (yes/no,if“yes”,options for pre-existing conditions include coronary heart disease,congestive heart failure,cerebrovascular disease,asthma,chronic obstructive pulmonary disease [COPD],diabetes,kidney disease,peptic ulcer,cancer,arthritis,intervertebral disc disease,and osteoporosis).
2.3.2.Assessment of fall risk
Fall risk was measured using a fall risk self-assessment checklist from the Stopping Elderly Accidents,Deaths &Injuries (STEADI)Toolkit[17].The checklist consists of 12 items that require a“yes”or “no” response.For the first two items,a “yes” response scores 2 points each,and a “yes” response to the remaining ten questions scores 1 point each.The score ranged from 0 to 14 points,with a higher score indicating a higher risk of falls.Those who scored 4 points or more were considered at risk for falling.The Chinese version translated by Li and Ding [18] was validated,and the Cronbach’s α coefficient is 0.608 in community participants.
2.3.3.Assessment of frail scale
The frailty status was assessed using the Chinese version of the FRAIL scale with a Cronbach’s α coefficient of 0.705[19].The scale includes five self-reported items: fatigue,resistance,ambulation,illnesses,and loss of weight.A response of“yes”to each was scored as 1 point.The participant was given 1 point for each illness out of the 11 listed,and 1 point for a 5%or more weight loss in the past 12 months.The total score ranges from 0 to 5.Individuals are classified into three categories based on their scores: robust (0 points),prefrail (1-2 points),and frail (3-5 points).In addition,frailty can also be divided into binary category variables (robust or frailty)[20,21].
2.3.4.Assessment of hypertension
The diagnosis of hypertension referred to the“Guidelines for the Management of Hypertension in China”[4].Only participants with a definitive hypertension diagnosis confirmed by their physicians were included in the hypertension group;others were included in the non-hypertension group.
2.4.Data collection
Participants were comprehensively informed about the study’s aims,procedures,and data protection and were willing to be volunteers.Those who agreed to participate in this study were asked to sign an informed consent form.The data was collected through face-to-face,one-on-one interviews in participants’ homes or community healthcare centers.If any participants had questions or concerns,the researchers were available to provide face-to-face assistance as needed.
2.5.Data analysis
SPSS version 25.0 for Windows (SPSS Inc,Chicago,IL) and R version 4.0.5 (R Foundation for Statistical Computing,Vienna,Austria) were used for analyses.The categorical variables were displayed as frequencies and percentages.These characteristics were compared in the groups with and without hypertension.In each group,the distribution of distinct frailty statuses was estimated using the Kruskal-Wallis rank sum test,followed by post-hoc Bonferroni tests.Logistic regression models were used to assess the odds ratio(OR)and 95%confidence interval(CI)for the associations among frailty,hypertension,and fall risk.A series of regression models were constructed as follows:Model 1 adjusted for age and sex,and Model 2 additionally adjusted for marital status,education level,per capita monthly income of households,smoking history,drinking history,polypharmacy,and comorbidities.The generalized additive model (GAM) and smooth curve fitting (penalized spline method) were used to estimate the association between frailty and fall risk in different hypertension statuses.The model calculated P for the trend by entering the frail scores as the three categories.P-values <0.05 were considered statistically significant.
2.6.Ethical considerations
The Ethics Committee of Jiangnan University approved this study(JNU202209011RB06).The study was conducted according to the guidelines of the Declaration of Helsinki.
3.Results
3.1.Characteristics of participants
As shown in Table 1,a total of 401 participants were included in this study.Of all 401 older adults,152 (37.9%),211 (52.6%),and 38 (9.5%) were considered to be robust,pre-frail and frail.A total of 205(51.1%)patients with hypertension and 196(48.9%)older adults without hypertension were included in this study.139 (34.6%)participants had high fall risk by the STEADI screening checklist.
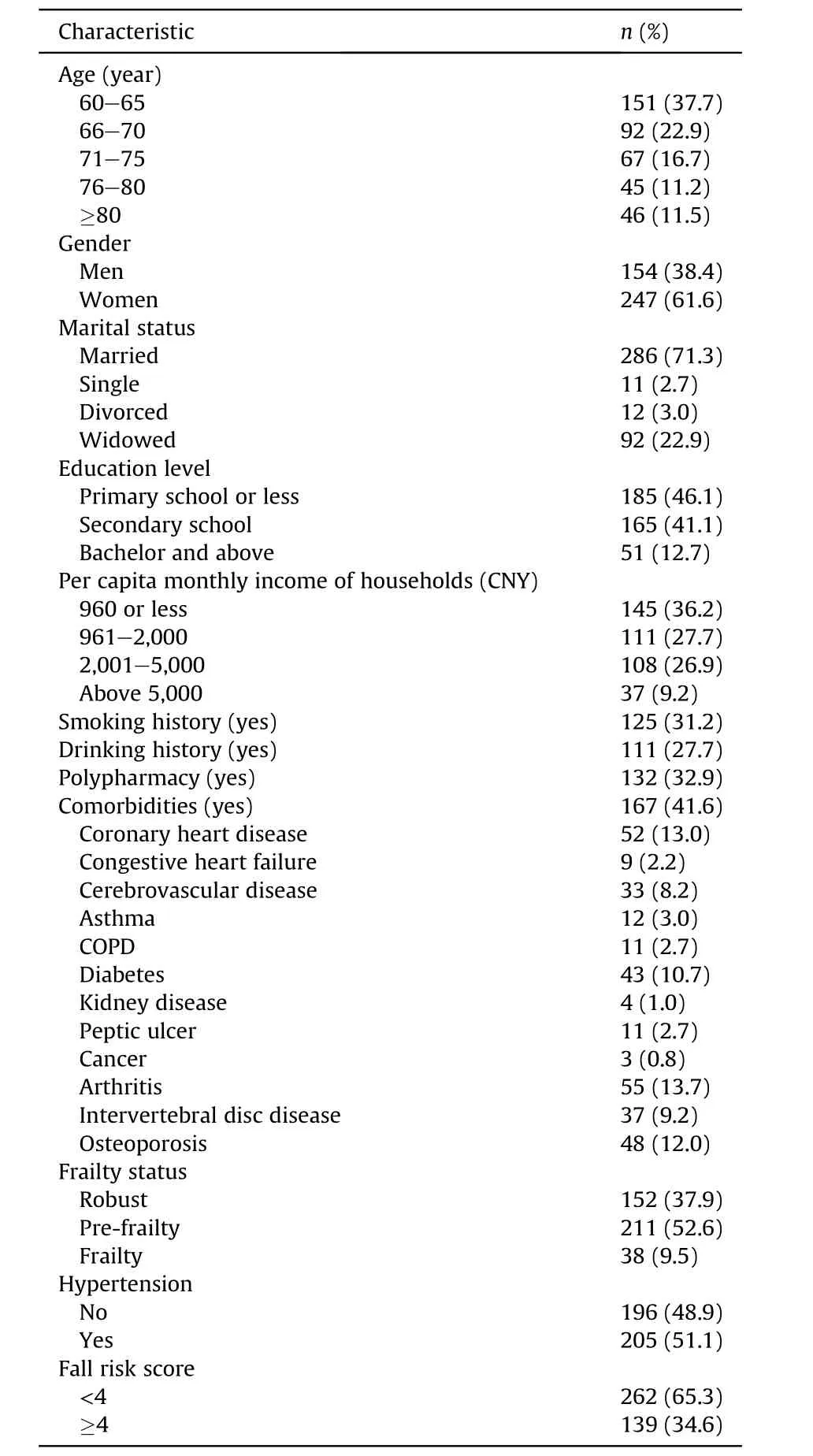
Table 1 Participant characteristics (n=401).
In Table 2,the prevalence rates of pre-frailty or frailty in older adults with hypertension were 61.0% and 11.2%,respectively.No statistically significant differences were found in age,gender,marital status,education level,and per capita monthly income of households among different groups of older adults with hypertension.However,significant differences in falls can be observed among the robust,pre-frailty,and frailty groups(P <0.001).In the hypertension group,post-hoc tests showed significant differences in fall risk between the robust group and the pre-frailty group (P <0.001),the robust group and the frailty group (P <0.001).In addition,statistically significant differences were observed in polypharmacy and comorbidities (coronary heart disease,cancer,arthritis,or osteoporosis) among the robust group,the pre-frailty group,and the frailty group with hypertension (P <0.05).

Table 2 characteristics of participants with hypertension and different frailty statuses (n=205).
3.2.Independent effect of frailty status and hypertension on fall risk
The individual effect of frailty and hypertension on the prevalence of fall risk is shown in Table 3.In contrast with robust,frailty had a strong relationship with the higher fall risk.The OR were 19.79(95% CI 8.31-47.10;P <0.001) in the crude model.Confounding variables were controlled to explore the independent effect of frailty and hypertension on falls.In Model 2,after adjusting for age,gender,marital status,education level,per capita monthly income of households,smoking history,drinking history,polypharmacy,and comorbidities,the older adults with frailty were more likely to have higher fall risk (OR 8.52,95% CI 3.21-22.57;P <0.001).Furthermore,an apparent linear trend of frailty status with fall risk was detected (P for trend < 0.001).Similarly,compared with the non-hypertension group,hypertension significantly increased the prevalence of fall risk (OR 1.87,95% CI 1.11-3.13;P=0.019).
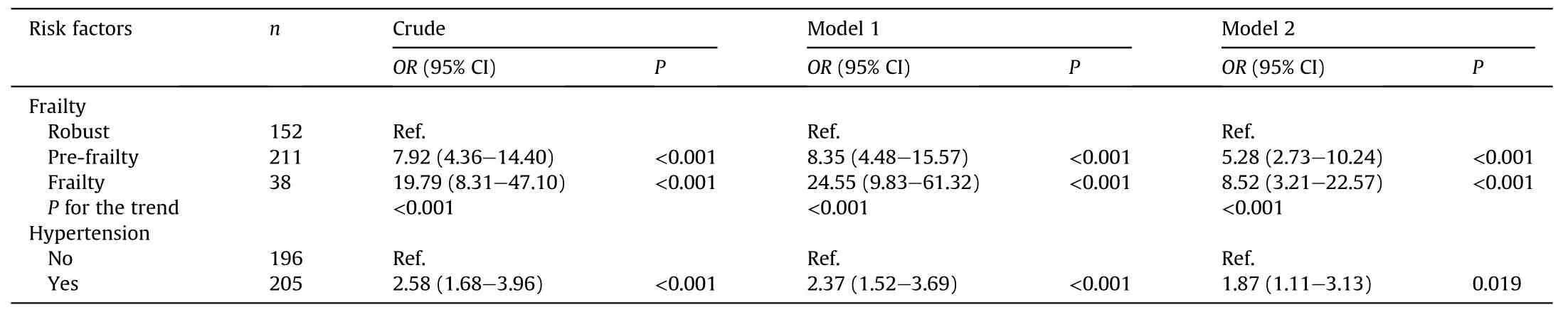
Table 3 Independent effects of frailty and hypertension on fall risk.
3.3.Associations between frailty status and fall risk among older adults with and without hypertension
Frailty and hypertension were examined together,as shown in Fig.1a.The group with hypertension and frailty had the highest fall risk,with an OR of 12.24.In the non-hypertension group,the older adults with higher frailty scores had a higher fall risk.Furthermore,the fall risk in older adults with hypertension was higher than that in the non-hypertension group.As shown in Table 4,the participants were separated into four groups further to explore the joint effect of frailty and hypertension.Frailty was defined as being pre-frail or frail,which was grouped in analysis.The crude models,Model 1 and Model 2 showed a higher fall risk in the frailty groups.Compared with their counterparts,frailty with hypertensives had the highest prevalence of fall risk (OR 8.34,95% CI 3.30-21.04;P <0.001).In the non-hypertension-merged frailty group,the OR (95% CI) of fall risk was 4.63 (1.81-11.86) in multivariate-adjusted model 2 (P=0.001).However,no significant relationshipbetween robust status and fall risk was found among those with hypertension.
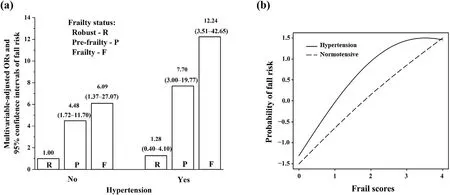
Fig.1. In-depth relationship among frailty,hypertension,and fall risk.
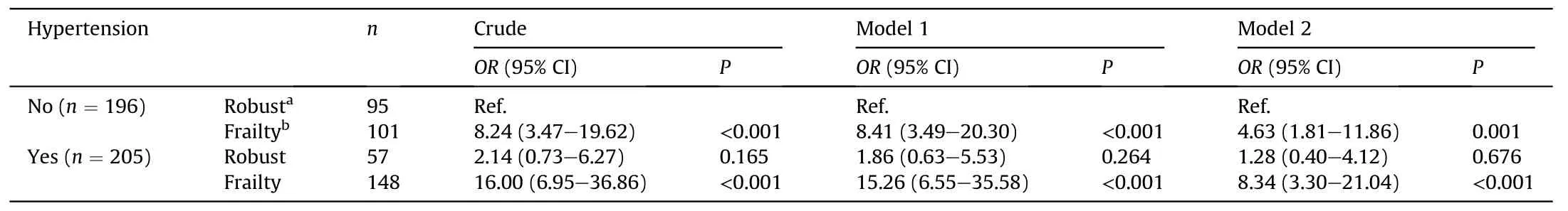
Table 4 Joint effects of frailty status and hypertension on fall risk.
The GAM and fully adjusted smooth curve fitting were used to assess further the association between frailty and fall risk in different hypertension groups.Fig.1b shows a nonlinear association between frailty and fall risk in all participants.However,the participants with hypertension had a higher risk of falls with growing frailty status than the non-hypertension group,especially during the middle (1-3 points) of the frailty scores.This finding suggested that the progress of pre-frailty to frailty status was associated with an increased prevalence of fall risk among older adults with hypertension.
4.Discussion
The present study found that in the hypertension group,the ratios of pre-frailty and frailty were 61.0% and 11.2%,respectively,and those in the non-hypertension group were 43.9% and 7.7%,respectively (data not shown).The findings indicated that older adults with hypertension were more likely to be pre-frail or frail than those without hypertension.In line with the results of the non-hypertension group in this study,pre-frailty and frailty prevalence rates of 43.1% and 8.0%,respectively,were reported among Chinese community-dwelling older adults [22].The prevalence of frailty with hypertension was slightly lower in the present study than in other studies [23-26] due to the different frailty assessment methods and diverse personal characteristics,which may be explained as follows: (a) more health promotion activities among hypertensive adults may contribute to the lower prevalence of frailty[27],and(b)bedridden older adults were not included in this study,which may result in a slightly lower prevalence of frailty.However,our data presented a high prevalence of frailty integrated with hypertension.The previous review indicated that the increasing prevalence of hypertension and the risk-benefit ratio of hypertension therapy were affected by frailty [6].In the present study,the prevalence of hypertension in frail individuals was 60.5%(23/38),which was lower than that in the previous systematic review [23],potentially due to the relatively low awareness rate of hypertension among older adults with frailty in the community.According to the guideline [28],proper treatments should be performed to improve older adults’ physical status,indicating that future interventions to manage hypertension may need to consider the frailty status [8,29].
In the present study,the findings indicated significant differences in polypharmacy and comorbidities among older hypertensive adults with robust,pre-frail,or frail status,which was in accordance with other studies [30].Data suggested older hypertensive adults with multiple medications and comorbidities could have an increased risk of iatrogenesis adverse effects [31],which may increase frailty degree.Medical staff should assess the polypharmacy and comorbidities of older patients with hypertension to delay the progress of frailty.Moreover,more effective management of medications and comorbidities in frail older adults should be performed [32].However,the indicators of frailty,not blood pressure or antihypertensive medication,were confirmed to increase the fall risk in older adults taking antihypertensive medication[33].Similarly,the present study indicated that the risk of falls in the hypertension group was significantly different between robust adults and pre-frail/frail participants.A systematic review and meta-analysis showed that frailty,polypharmacy,and comorbidities,such as hypertension,diabetes,and cardiac disease,increased the risk of falls in the aging population[34].These findings implied complex relationships among frailty status,hypertension,and fall risk in older adults.
Several studies found that hypertension is a risk factor for falls in older adults[9,35].In the present study,community-dwelling older adults with hypertension were found to have a higher risk of falling (OR 1.87,95% CI 1.11-3.13).Considering the influencing factors of hypertension and falls,researchers presented that vascular calcification resulted in hypertension and osteoporosis [36].In addition,the effects of different frailty statuses on fall risk were investigated,suggesting that frail older adults had a higher risk of falls than the pre-frailty or robust group [37].In a recent meta-analysis,a significant association between frailty status,hypertension,and fall risk was indicated [38].However,few studies explained the joint effects of hypertension and frailty on fall risk.No studies have presented the profound relationship between various frailty statuses,hypertension,and fall risk.The present results showed that older adults with frailty had a higher fall risk among hypertension than pre-frail older adults.Moreover,the smooth curve fitting showed the relationship between frailty and fall risk among different blood-pressure groups.In the hypertension group,the older adults with pre-frailty to frailty status had a higher tendency to fall.In those with the highest frailty scores,the risk of falls no longer increased,just as the effect of injurious falls occurs mainly in people younger than 75,probably because they drop their guard until falls happen [39].Therefore,during the prevention of falls in older patients with hypertension,great importance should be attached to the intervention for the development of pre-frailty to frailty.
5.Limitations
Despite the strength of the evidence in this study,several limitations should be considered.Firstly,this cross-sectional study could not confirm the causal relationship between frailty,hypertension,and fall risk.A longitudinal study should be conducted to explore whether older adults with merged frailty and hypertension could develop a higher risk of falls.Secondly,we included only those whose health status was better and not the disabled ones or those lying in bed for a long time,which may lead to a possible bias of non-respondents.Thirdly,this was a single-center study with a small sample size conducted by convenience sampling,limiting the generalizability of our findings.Furthermore,the results of this study showed the observation performance.In the future,largescale and multi-center studies are needed,and the mechanisms of the fluctuation among frailty,hypertension,and fall risk should be examined in depth.
6.Conclusion
In summary,higher frailty status may lead to higher fall risk in older adults with hypertension compared with those without hypertension.The status of pre-frailty to frailty may generate a higher tendency to fall among older adults with hypertension.These findings suggested that the combined assessment and intervention of frailty,hypertensive status,and fall risk are essential.Practitioners should focus more on the management of the progression of pre-frailty to frailty in older adults with hypertension to decrease fall risk.Further investigations should verify these findings in depth and explore the possible causality in the associations among frailty,hypertension,and fall risk for enhanced intervention to decrease fall risk in frail older adults with hypertension.
CRediT authorship contribution statement
Liping Teng:Conceptualization,Methodology,Supervision,Investigation,Formal Analysis,Writing-Review and Editing,Project a dministration.Danhui Wang:Conceptualization,Methodology,Investigation,Formal Analysis,Writing-Original Draft,Writing -Review &Editing.Zhou Zhou,Jun Sun,Min Zhu:Methodology,Investigation,Formal Analysis,Writing -Review and Editing .Renrong Wang:Conceptualization,Methodology,Funding acquisition,Supervision,Writing-Review and Editing,Project administration.
Funding
Nothing to declare.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declaration of competing interest
All authors declared no conflict of interest or any potential competing interest.
Acknowledgments
The authors wish to acknowledge all participants for their selfless collaboration and Yuping Wu,Liqun Guo,Jinping Li,Kewei Wang,Jingquan Li,and Yi Pan for their advice during the project.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2023.12.010.
杂志排行
International Journal of Nursing Sciences的其它文章
- Nursing leadership: Key element of professional development☆
- Comparison of the performance of four screening tools for sarcopeni a in patients with chronic liver disease
- Facilitators and barriers to the implementation of dietary nutrition interventions for community-dwelling older adults with physical frailty and sarcopenia: A qualitative meta-synthesis
- The prevalence and factors associated with sarcopenia in Thai older adults: A systematic review and meta-analysis Phatcharaphon Whaikid,Noppawan Piaseu*
- Air quality self-management in asthmatic patients with COPD: An integrative review for developing nursing interventions to prevent exacerbations
- Measurement properties of assessment tools of Kinesophobia in patients with cardiovascular disease: A systematic review
