The prevalence and factors associated with sarcopenia in Thai older adults: A systematic review and meta-analysis Phatcharaphon Whaikid,Noppawan Piaseu*
2024-02-27RamathibodiSchoolofNursingFacultyofMedicineRamathibodiHospitalMahidolUniversityThailand
Ramathibodi School of Nursing,Faculty of Medicine Ramathibodi Hospital,Mahidol University,Thailand
Keywords:
ABSTRACT Objective:This systematic review and meta-analysis aimed to assess the prevalence and identify factors associated with sarcopenia in older Thais.Methods:Research studies were searched in online databases,including PubMed,Embase,Scopus,and Thai-Journal Citation Index.The articles included in this review were limited to being published between January 1,2013 and January 31,2023 and observational study designs.The research quality was evaluated using the Joanna Briggs Institute (JBI) critical appraisal tool for prevalence studies.A metaanalysis was performed using the JBI SUMARI software.The review protocol has been registered on PROSPERO with the assigned ID CRD42023420514.Results:A total of 265 research articles were initially identified,out of which 17 articles were included in this study,including a total of 4,668 participants aged 60 years and over,consisting of 1,380(29.6%)men and 3,288 (70.4%) women.The overall prevalence of sarcopenia in Thai older adults was 20.7% (95% CI 14.4%-27.8%).Subgroup analysis of the sarcopenia prevalence based on the study areas revealed that the prevalence was 33.4% (95% CI 28.7%-38.3%) in hospitalized individuals,23.2% (95% CI 12.5%-35.9%) in outpatient clinic settings,and 17.3%(95%CI 9.4%-26.8%)in community-living older adults.Advanced age(OR=4.60,95% CI 3.07-6.91),being male (OR=2.30,95% CI 1.37-3.85),low body mass index (BMI)(OR=8.95,95% CI 6.05-13.25),and malnutrition (OR=2.78,95% CI 2.09-3.70) are strong predictors of sarcopenia in older adults in Thailand.Conclusions:This systematic review represents the first assessment of the overall prevalence and factors associated with sarcopenia in Thai older adults,indicating its significant concern within this population.These findings are of importance for public health management aimed at preventing and managing sarcopenia in the country.
What is known?
· In the rapidly aging global population,sarcopenia has emerged as a prominent health condition,garnering widespread attention from the general public and the healthcare system.
· The comprehensive systematic review assessing the prevalence and factors associated with sarcopenia in older adults has yet to be reported in Thailand.
What is new?
· The systematic review represents the first assessment of the overall prevalence and factors associated with sarcopenia in Thai older adults.
· The overall prevalence of sarcopenia in Thai older adults was 20.7% (95% CI 14.4%-27.8%).
· The study found that factors associated with sarcopenia in Thai older adults include age,gender,low physical activity,poor physical ability,prefrailty,body mass index,underweight status,waist circumference,calf circumference,type 2 diabetes,depression,mild cognitive impairment,malnutrition,and protein intake.
1.Introduction
The global aging population was increasing rapidly.According to a WHO survey,the proportion of the population aged 60 years and over will almost double by 2050 compared to 2015[1].Thailand is a country facing a growing aging population.Based on the latest data from a 2021 survey on Thai older persons,there has been a significant increase in the number of older adults compared to that in 1971.In fact,the proportion of older people now accounts for an astounding 19%of the entire population nationwide[2].Aging leads to profound physiological changes in body composition.One of the critical issues is the decline in skeletal muscle mass,together with an increase in fat mass[3].Previous studies have demonstrated that the age-related decline in muscle mass,commonly referred to as “sarcopenia,” is described by a progressive reduction in muscle mass,muscle strength,and physical performance[4].Furthermore,malnutrition,inadequate physical activity,and the presence of comorbidities are significant factors that contribute to the development of sarcopenia,in addition to the effects of increasing age [4].In 2016,the WHO officially recognized sarcopenia as a distinct disease concomitant with older adults,assigning it the disease code M62.84 [5].
Older adults with sarcopenia experience a loss of balance,which significantly increases the risk of falls and fractures [6].Furthermore,it contributes to functional decline[7],disability,diminished quality of life,longer hospitalization periods,and an increased risk of mortality from other complications[8],compared to older adults without sarcopenia [9].All these outcomes contribute to a more complex treatment process,increase treatment costs,and have an impact on the national public health system.The causes of sarcopenia in older adults can be attributed to various factors,which can be classified into two types based on the underlying cause [10].Firstly,primary sarcopenia is primarily associated with the natural aging process,where changes in body composition occur,leading to a decrease in muscle mass and bone mass,resulting in sarcopenia [3].Secondly,secondary sarcopenia is linked to underlying diseases,particularly chronic conditions associated with complex metabolic syndrome (MetS),such as type 2 diabetes [11],hypertension[12],end-stage renal disease(ESRD)[13],heart failure[14],solid tumors [15],and others.The use of statins can cause an abnormal elevation in creatine kinase (CK) levels,leading to rhabdomyolysis [16].Unintentional weight loss [17] and a lower body mass index (BMI) [18] contribute to the loss of muscle lean mass and bone mass.On the other hand,increased BMI [19] and expanded waist circumference [20] have been associated with an increased distribution of body fat,which in turn results in a decrease in muscle mass.Inadequate physical activity is closely associated with decreased body composition and diminished functional capacities in older adults [21].In older adults with depression,the body tends to produce elevated levels of interleukin-6 (IL-6) and tumor necrosis factor (TNF-α) [22,23].These factors are directly linked to muscle protein synthesis and the occurrence of rhabdomyolysis,eventually leading to a decline in muscle mass and muscle strength in older adults.
Recent systematic reviews and meta-analyses have highlighted variations in the prevalence of sarcopenia across different studies.Globally,the estimated prevalence of sarcopenia ranges from 10%to 27% [24],as evidenced by these findings.In Chinese older adults,the prevalence of sarcopenia was found to be 14% [25].In Korean older adults,the range varied from 11.4%to 14.9%[26].In Japan,the prevalence of sarcopenia among older adults was reported as 10%[27].The variations in the diagnostic criteria used for the diagnosis of sarcopenia can potentially account for the differences observed in the prevalence of sarcopenia across different studies.Additionally,factors such as the nationality and ethnicity of the older adults in each country can also contribute to these variations.In Thailand,the Asia Working Group for Sarcopenia (AWGS) consensus criteria are commonly utilized for diagnosing sarcopenia [28].However,the prevalence of sarcopenia among older Thai adults varies across different studies.
Due to the rapidly aging global population,there is an anticipated rise in the prevalence of sarcopenia among older individuals worldwide.Sarcopenia has emerged as a prominent health condition,garnering widespread attention from the general public and the healthcare system.This is primarily due to the potential impact of sarcopenia on health services utilization,making it a critical concern for public health.This places a significant burden on the healthcare system,particularly in the face of an aging population.Consequently,there is a growing need for a comprehensive understanding of the age-related diseases associated with sarcopenia to effectively prepare,manage,and alleviate the strain on healthcare resources.Furthermore,in order to achieve the goal of healthy aging,it is crucial to assess the overall prevalence of sarcopenia among older Thai adults.This assessment will help guide the development of guidelines aimed at promoting health and facilitating appropriate behavioral changes for older adults.Despite recent studies focusing on the prevalence of sarcopenia,there is a lack of consistency in the results across different studies.Furthermore,Thailand has yet to report a systematic review and metaanalysis that comprehensively assesses the prevalence and factors associated with sarcopenia in older adults.Therefore,the aim of this systematic review and meta-analysis is to assess the prevalence of sarcopenia and identify the factors associated with it in the Thai population aged 60 years and above.The findings of this study can serve as a basis for developing guidelines aimed at effectively managing and preventing sarcopenia among older Thai adults,thereby promoting their overall well-being.
2.Methods
This study is a systematic review and meta-analysis.It aims to explore the prevalence of sarcopenia and examine the factors associated with it among Thai older adults aged 60 years and above.The review protocol has been registered on PROSPERO,with the assigned ID CRD42023420514.It is reported in accordance with the PRISMA guidelines.
2.1.Search strategy
In this systematic review,the researchers employed a comprehensive search strategy across four databases,both in Thailand and internationally.The databases included one database in Thailand,namely the Thai-Journal Citation Index (TCI),and three English language databases:PubMed,EMBASE,and Scopus.The publication period under consideration covered a duration of ten years (between January 1,2013 and January 31,2023).
We conducted a systematic review and meta-analysis following the PICo framework[29].We established a PICo framework using the following terms.Population:Older adults aged 60 and over(referred to as“elderly people,”“older adults,”“aged people,”“aging people,”“older people,” “seniors,” “geriatric people,” “late life adults,” or “older patients”).Phenomenon of Interest: The prevalence and factors related to sarcopenia (including terms such as “prevalence of sarcopenia,” “factors of sarcopenia,” “sarcopenia,” “low muscle mass,” “low skeletal muscle,” “low muscle strength,” “low gait speed,” “low physical performance,” “low physical functional performance,” “low walking speed,” “muscle loss,” and “amyotrophy”).Context: Thailand (referred to as “Thai context,” “Thai population,”“Thai people,” “Thai persons,” “Thai elderly,” “Thai communitydwelling,”“Thai patient,”or“Southeast Asian population”).
2.2.Inclusion and exclusion criteria
We included studies that focused on older people with sarcopenia,considering various diagnostic criteria used to assess sarcopenia.The study was not limited to any specific diagnostic criterion,as long as the chosen criterion was supported by reliable evidence.Furthermore,there were no restrictions based on the gender of older adults.This study selected cross-sectional or cohort studies,including follow-up studies.The selection process adhered to the following inclusion criteria:
The research article had to provide information in the abstract and full text regarding the prevalence of sarcopenia,related factors,and/or older adults.The sample of the research article had to include: 1) Thai individuals aged 60 years and over exclusively;2)The research articles considered were published in either Thai or English;3) The research articles had undergone a peer-reviewed procedure and are accessible in full text through a reliable database;and 4) The publication date of the research article fell between January 1,2013 and January 31,2023.The following criteria were excluded from this study: unsourced studies,research with inadequate methodology,conference abstracts,and reviews.Specifically,randomized controlled trials and systematic reviews involving animal research were excluded.
2.3.Study selection process and data extraction
Two researchers conducted a thorough search across all databases,evaluated the retrieved studies,and compared their results to ensure no studies were unintentionally excluded.Disagreements were resolved via discussion between the two researchers.Data extraction from all selected research articles was compiled into a systematic review record table.A table summarizing the characteristics of the included studies was created,which included information such as author names,publication year,language,study design,diagnostic criteria for sarcopenia,participant details (e.g.,age,gender distribution),geographic region,study setting,prevalence of sarcopenia,and factors associated with sarcopenia.During the screening process,all research articles utilized in the analysis were independently evaluated,reviewed,and discussed by two reviewers to reach a consensus on the extracted data.
2.4.Quality appraisal
The credibility of the empirical evidence was assessed independently by two researchers using the Joanna Briggs Institute(JBI)critical appraisal checklist for studies reporting prevalence data[30] to evaluate the risk of bias.Nine items on the JBI critical appraisal checklist for studies reporting prevalence data tool assigns a score ranging from 0 to 9,with a higher score indicating lower risk of bias.Responses for each item include“yes=1”or“no,unclear or not applicable=0”.In terms of interpretation,a score below 4 indicates low research quality,a score between 5 and 7 suggests moderate research quality,and a score between 8 and 9 indicates high research quality.
2.5.Statistical analysis
The meta-analysis was performed with the JBI SUMARI software to calculate the pooled prevalence of sarcopenia among Thai older adults.A random-effects model was employed using the Freeman-Tukey transformation approach,accounting for various instruments used to measure sarcopenia.Subgroup analysis was conducted to determine the pooled prevalence of men and women.The pooled prevalence of sarcopenia was calculated using effect size and weighted mean,along with 95%confidence intervals(95%CI).A meta-analysis was conducted to examine factors associated with sarcopenia,employing a fixed-effect model through the inverse variance approach.The primary analysis uses 95% CI for an effect size with odds ratio(OR).Statistical analysis of heterogeneity in this study was carried out using I2statistics,with the following interpretation: 1) may not be important (I20-24.9%),2) may represent moderate heterogeneity (I225.0%-49.9%),3) may represent substantial heterogeneity (I250.0%-74.9%),and 4)considerable heterogeneity (I275.0%-100%).Moreover,heterogeneity is acknowledged,considering Chi-square (χ2) P-values <0.1,indicating the presence of heterogeneity.Subgroup analyses were performed with sufficient data.For factors where statistical analysis was not feasible,the results were presented through descriptive narrative.
3.Results
3.1.Selection of included studies
The literature search yielded a total of 265 research articles from the electronic database/search engine.After removing duplicate records,183 research articles were evaluated and screened for eligibility based on predetermined criteria.Upon reviewing the titles and abstracts,133 research articles were excluded.Furthermore,during the assessment of full-text articles,an additional 33 research articles were deemed ineligible,as they did not meet the inclusion criteria.As a result,17 research articles [19,31-46] met the inclusion criteria and were included in the quantitative synthesis,as illustrated in Fig.1.
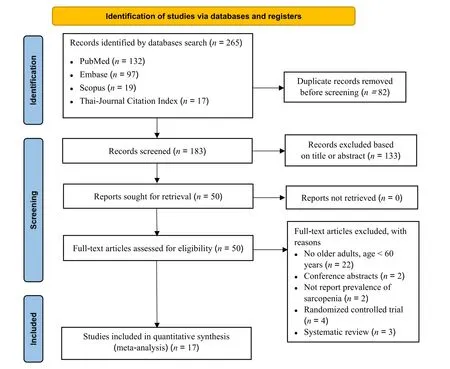
Fig.1. Flow chart of study selection.
3.2.Characteristics of included studies
The search encompassed research articles published over a period of ten years,from 2013 to 2023,resulting in the identification of 17 articles that met the inclusion criteria.Among these articles,two were conducted in hospital settings [31,46],five in outpatient clinics [32,35,43e45],and nine in community settings [19,33,34,36,37,37,38,38,39,39e42].Of the included articles,three were published in Thai,while the remaining fourteen were published in English.The systematic review included a total of 4,668 individuals,with 3,288 women and 1,380 men.One study focused exclusively on women,while the rest of the studies included both genders.The sample sizes varied across the studies,ranging from a minimum of 82 participants to a maximum of 510 participants.All of the research articles included older individuals aged 60 years and over.Regarding the criteria used for diagnosing sarcopenia in Thai older adults,the criteria set by the AWGS in 2014 was used in eight articles,the AWGS criteria from 2019 in six articles,both the AWGS 2014 and AWGS 2019 criteria were used to assess participants in one article,and SARC-F (the 5-component questionnaire that measures strength,assistance walking,rise from a chair,climb stairs,and falls) criteria in one article.Additionally,one study utilized handgrip strength (HS)-based criteria.The majority of the research designs employed were cross-sectional in nature(Table 1).
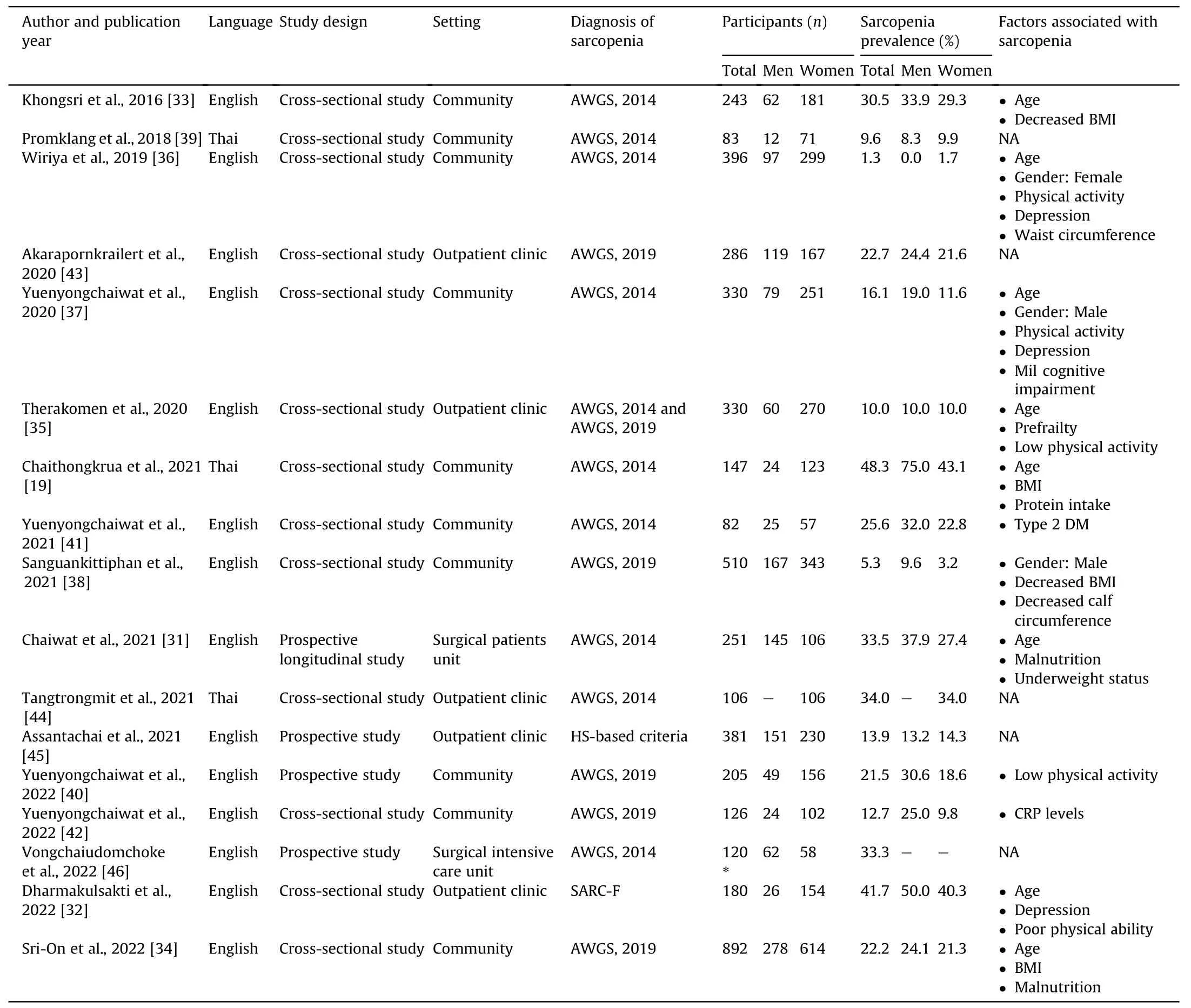
Table 1 Summary of study characteristics.
3.3.Methodological quality of included studies
As for methodological quality,the score ranged from 7 to 9 out of 9 points according to the JBI checklist.All studies appropriately addressed the target population,used a validated method to identify sarcopenia,and measured it in a reliable way for participants.Among these studies,15 were classified as low risk,while two were classified as moderate risk,as indicated in Table 2.
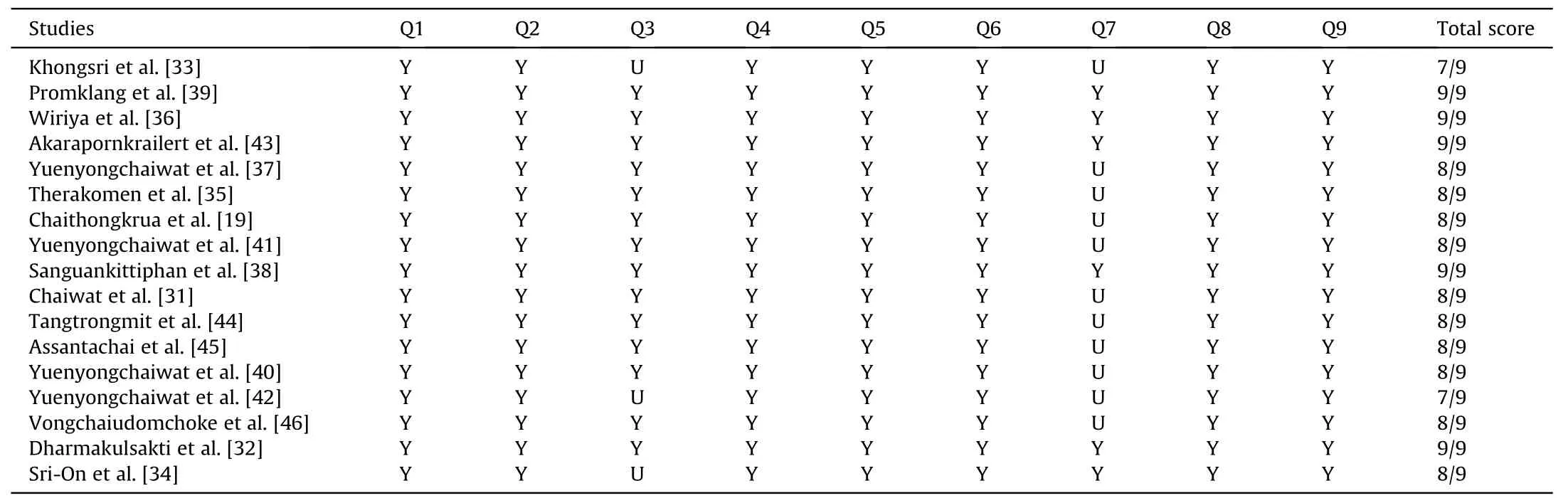
Table 2 Quality appraisal of included studies.
3.4.Prevalence of sarcopenia
Overall prevalence of sarcopenia.Among the 17 studies included in the review,the overall prevalence of sarcopenia in Thai older adults was 20.7% (95% CI 14.4%-27.8%),with high heterogeneity(I2=96.8%,P <0.001) (Fig.2).Furthermore,when study settings were considered,the prevalence of sarcopenia was as follows:33.4% (95% CI 28.7%-38.3%) in hospitals,with no heterogeneity (I2=0.0%,P=0.991);23.2 % (95% CI 12.5%-35.9%) in outpatient clinics,with high heterogeneity (I2=96.0%,P <0.001);and 17.3%(95% CI 9.4%-26.8%) among older adults living in the community,with high heterogeneity (I2=97.4 %,P <0.001) (Fig.3).
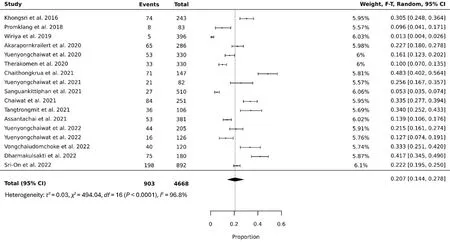
Fig.2.Forest plot of the pooled prevalence of sarcopenia in Thai older adults.
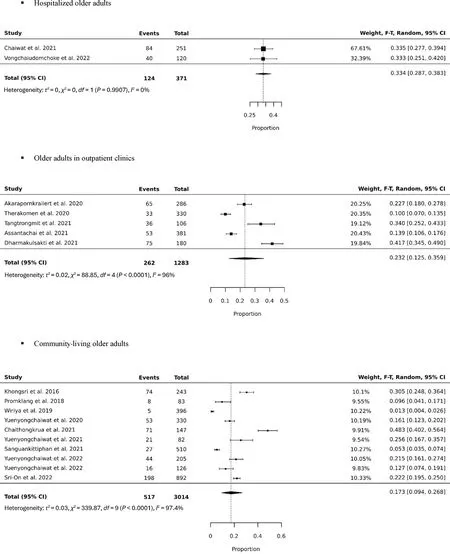
Fig.3.Subgroup analysis: Forest plot of the pooled prevalence of sarcopenia among Thai older adults in hospitals,outpatient clinics,and communities.
Prevalence of sarcopenia in male older adults.Out of the 17 studies,16 studies reported data on a total of 1,380 men.The prevalence of sarcopenia among older men was 26.2% (95% CI 18.0%-35.4%),with high heterogeneity (I2=90.5%,P <0.001)(Fig.4).Specifically,the prevalence of sarcopenia among hospitalized older men was 38%.In the outpatient clinic,the prevalence of sarcopenia was 21.8%(95%CI 8.4%-39.1%),with high heterogeneity(I2=91.1%,P <0.001).Among older men living in the community,the prevalence of sarcopenia was 27.1%(95%CI 16.0%-39.7%),with high heterogeneity (I2=90.2 %,P <0.001) (Fig.5).
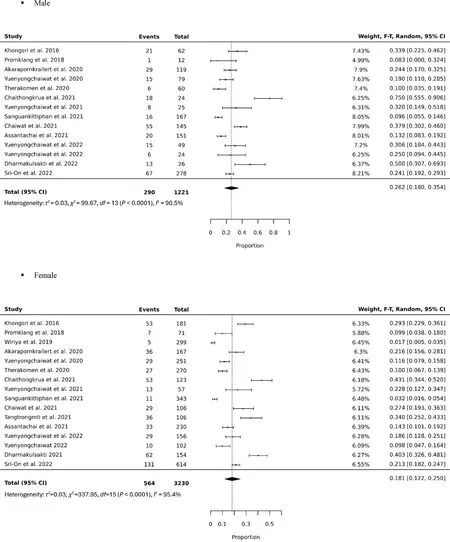
Fig.4.Subgroup analysis: Forest plot of the pooled prevalence of sarcopenia in Thai male and female older adults.
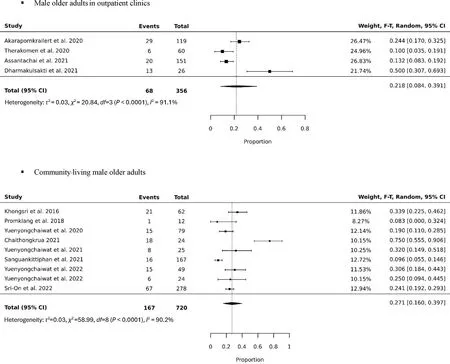
Fig.5.Subgroup analysis: Forest plot of the pooled prevalence of sarcopenia among Thai male older adults in outpatient clinics and communities.
Prevalence of sarcopenia in female older adults.Among the 17 studies included in the analysis,data on a total of 3,288 women were reported.The prevalence of sarcopenia among older women was 18.1% (95% CI 12.2%-25.0%),with high heterogeneity(I2=95.4%,P <0.001) (Fig.4).Specifically,in hospitals,the prevalence of sarcopenia was 27.0 %.In the outpatient clinic,the prevalence was 22.8% (95% CI 12.5%-35.0%),with high heterogeneity(I2=94.1%,P <0.001).Among older women living in the community,the prevalence of sarcopenia was 15.1% (95% CI 8.0%-23.9%),with high heterogeneity (I2=96.1%,P <0.001) (Fig.6).
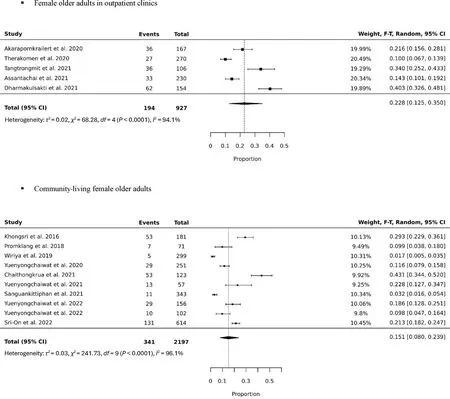
Fig.6.Subgroup analysis: Forest plot of the pooled prevalence of sarcopenia among Thai female older adults in outpatient clinics and communities.
3.5.Factors associated with sarcopenia
Based on the review of 12 studies,several factors associated with sarcopenia in Thai older adults were identified.These factors were categorized into two groups: personal factors and healthrelated factors.
Personal Factors.Personal factors refer to the biological characteristics of each older person that affect the development of sarcopenia.Age is a personal factor associated with sarcopenia[19,31-37].Gender is also found to be associated with sarcopenia.One study reported that females are associated with sarcopenia[36],while two other studies revealed an association between males and the development of sarcopenia[37,38].Results of metaanalysis for three studies revealed that age was associated with sarcopenia with an OR of 4.60 (95% CI 3.07-6.91),with low heterogeneity(I2=41.0%,P <0.001).Two studies of males revealed an OR of 2.30 (95% CI 1.37-3.85) associated with sarcopenia,with no clinically significant heterogeneity (I2=15.0%,P <0.01),as illustrated in Fig.7.
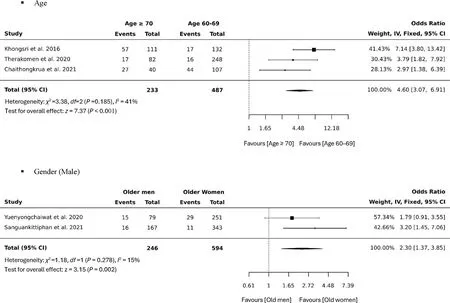
Fig.7.Forest plot of the pooled odds ratios for sarcopenia in Thai older adults by age and gender (male).
Health Related Factors.Several factors have been identified as associated with the development of sarcopenia in Thai older adults.These factors include physical activity levels,poor physical ability,prefrailty,BMI,underweight status,waist circumference,calf circumference,type 2 diabetes,depression,mild cognitive impairment (MCI),malnutrition,protein intake,and C-reactive protein levels.Among the identified factors,physical activity levels [35-37,39,40] and poor physical ability [32] were found to contribute to sarcopenia in the majority of the five studies.Additionally,four studies reported an association between BMI and the development of sarcopenia [19,33,34,38].Other factors associated with sarcopenia included underweight status[31],increased waist circumference [36,38],type 2 diabetes in older adults [41],anddepression in older adults [32,36,37].Furthermore,prefrailty [35],malnutrition in older adults[31,34],inadequate protein intake[19],and elevated C-reactive protein levels [42] were also identified as factors associated with the development of sarcopenia.Nevertheless,the outcomes of the study compilation indicate a lack of available studies at present.Consequently,a mere two factors possess an adequate of data for analysis.Subsequently,the factors selected for integration into the meta-analysis encompass low BMI and malnutrition.
Meta-analyses of five studies on low BMI showed an ORof 8.95(95%CI 6.05-13.25),with high heterogeneity(I2=79.0,P <0.001).It was indicated that lower BMI was significantly associated with sarcopenia.Older adults with lower BMI were 8.95 times more likely to have sarcopenia than those with normal and high BMI.The analysis of two studies on malnutrition revealed an OR=2.78(95%CI 2.09-3.70),with moderate heterogeneity(I2=62.0%,P <0.001),as illustrated in Fig.8.The meta-analysis likewise showed that malnutrition was associated with sarcopenia.Older adults with malnutrition were 2.78 times more likely to have sarcopenia compared to those with no malnutrition.
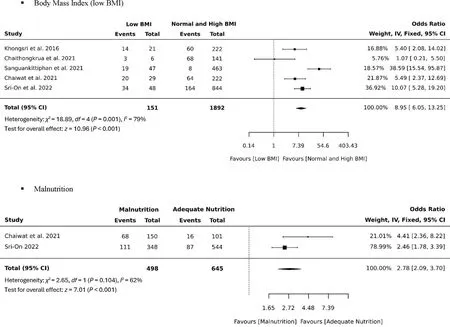
Fig.8.Forest plot of pooled odds ratios for sarcopenia in Thai older adults with low BMI and malnutrition.
4.Discussion
This systematic review provides valuable insights into the overall prevalence of sarcopenia among older adults in Thailand.Additionally,the evaluation of factors associated with sarcopenia in Thai older adults takes into consideration the potential influence of nationality,ethnicity,and cultural backgrounds of the country.It recognizes the importance of environmental factors that may contribute to the development of sarcopenia.Environmental factors affecting food consumption behaviors include economic,social,and cultural aspects.The current social situation and shifts within the community also contributed to these changes.A growing population has transitioned from the traditional lifestyle,characterized by labor-intensive farming,gardening,and outdoor activities,to a sedentary lifestyle that frequently underutilizes core muscles.Therefore,this literature review successfully addresses the gaps in knowledge by presenting the overall prevalence and identifying factors associated with sarcopenia,specifically in the context of Thailand’s older adult population.
The prevalence of sarcopenia in Thailand varies depending on the diagnostic criteria used,including AWGS 2014,AWGS 2019,SARC-F,and HS-based criteria.The overall prevalence of sarcopenia among Thai older adults was 20.7%(95%CI 14.4%-27.8%),showing a descending trend in the prevalence of sarcopenia in hospitals,outpatient clinics,and communities.Even when considering the same diagnostic criteria,there are still variations in the prevalence of sarcopenia among the older Thai population.However,the results consistently demonstrate that sarcopenia is a prevalent condition among older adults in Thailand.Therefore,understanding the factors associated with sarcopenia in Thai older adults is crucial for implementing strategies aimed at preventing sarcopenia in this population.
Our systematic review reveals that the causes and factors associated with sarcopenia can be categorized into two main factors: personal factors and health-related factors.Personal factors include age and gender,which have been identified as significant contributors to the development of sarcopenia.Health-related factors include as follows: low physical activity,poor physical ability,prefrailty,low BMI,underweight status,waist circumference,calf circumference,type 2 diabetes,depression,MCI,malnutrition,protein intake,and C-reactive protein levels.
Age is a significant factor associated with sarcopenia[19,31-37].As individuals enter older adulthood,physiological and body composition changes occur,resulting in various declines in performance [3].Older adults experience reductions in musculoskeletal weight[47]and vitamin D absorption[48],as well as decreased production of testosterone,estrogen,and growth hormones [49].This population also faces various health issues,including sarcopenia [4].Previous studies have shown that the prevalence of sarcopenia increases with age:19.2%in the age group of 20-39 years,29.1%in the age group of 40-64 years,and 42.3%in the age group of 65 years and above [50].These findings suggest that sarcopenia is not exclusive to older adults.However,the prevalence of sarcopenia was found to be more than twice as high among older adults compared to adolescents and adults aged 20-39 years.
Gender is a factor associated with sarcopenia,and the evidence shows varying results.One research article found that women have a higher association with sarcopenia compared to men[36],which is consistent with several previous studies reporting a higher prevalence of sarcopenia in women than in men[25].Menopause,a physiological process experienced by all women as they age,is associated with a decrease in estrogen levels,leading to a reduction in muscle mass [51].A previous systematic review and metaanalysis found a 15% prevalence of sarcopenia in women,which was higher than the 14%prevalence in men[25].On the other hand,two research articles reported that men had a higher incidence of sarcopenia compared to women [37,38].This may be attributed to age-related hormonal changes that affect men more significantly than women[52].Other studies have also found that men are more likely to develop sarcopenia compared to women [18].The prevalence of sarcopenia was found to be 11% higher in men than 9% in women[53].Similarly,in a meta-analysis of sarcopenia prevalence in older Chinese individuals,the prevalence was 12.9%in men and 11.2% in women [54].These findings highlight the complex relationship between gender and sarcopenia,suggesting that hormonal and physiological factors contribute to the gender differences observed in sarcopenia prevalence.
Low physical activity and poor physical ability have been consistently associated with sarcopenia in Thai older adults,as indicated by multiple studies [32,35-37,39,40].These findings align with previous research demonstrating that low levels of physical activity and impaired ability to perform daily activities are risk factors for sarcopenia [55].A study on sedentary behavior in older adults revealed that the average sedentary time was 6.1 h per day,and the risk of developing sarcopenia was 1.33 times higher in individuals with increased sedentary behavior compared to those with moderate-intensity physical activity [56].Conversely,adequate levels of physical activity have been shown to reduce the incidence of sarcopenia[57].Regular exercise in older adults leads to increased mitochondrial content,similar to that observed in younger adults,highlighting the importance of maintaining appropriate physical activity levels to delay the onset of sarcopenia [58].Furthermore,studies have demonstrated that sufficient physical activity decreases the risk of sarcopenia in older adults with obesity,with a risk reduction of 45%in men and 29%in women [59].These findings underscore the vital role of maintaining an active lifestyle and engaging in regular physical activity to mitigate the risk of sarcopenia among older individuals.
Prefrailty has been identified as an association with sarcopenia in Thai older adults [35].The definitions of frailty and sarcopenia share common characteristics [60].Frailty can be characterized by at least three of the following physical features: unintentional weight loss,exhaustion,weakness,slow gait speed,and low physical performance[61].Previous research has indicated that the most prevalent diagnostic criteria for community-dwelling older adults with prefrailty were slow gait speed in 43% of cases and weakness in 54% of cases [62],which are indicative of sarcopenia.These findings are consistent with previous studies that have shown that older adults with prefrailty are 2.77 times more likely to have sarcopenia compared to those without prefrailty [63].
In Thai older adults,both lower BMI and higher BMI have been associated with sarcopenia [19].Older adults with lower BMI [33,34,38] and underweight status [31] have shown associations with sarcopenia,which aligns with previous studies indicating that underweight older individuals experience muscle deterioration,similar to older adults with obesity[18].These associations can be attributed to factors such as malnutrition and inadequate protein intake,which can impede muscle mass development and contribute to sarcopenia [64].The prevalence of sarcopenia is markedly high in older adults with low body weight or low BMI,reaching up to 92.9% [65],while it is reduced by 91.81% in older adults with high BMI[65].Conversely,obesity and higher BMI have also been associated with sarcopenia in Thai older adults [19],in line with studies demonstrating that excessive fat mass in the body can interfere with glucose pathways,induce insulin resistance,and contribute to sarcopenia [66].A previous systematic review and meta-analysis found that lower BMI is associated with a decreased risk of sarcopenia[67].Additionally,a research has shown that the prevalence of sarcopenia is 37.0% in older adults with a BMI of 25.0-29.9 kg/m2and 54.3%in those with a BMI greater than 30 kg/m2[68].These findings emphasize the key role of sufficient and nutritious food in promoting healthy aging,emphasizing a focal strategy for delaying the onset of sarcopenia.Therefore,underweight older adults should be encouraged to gain weight and enhance muscle strength,considering both calories and sufficient protein intake.Screening for sarcopenia should also be conducted for older adults who are overweight,allowing for support in selfcare,including recommendations for resistance exercises tailored to this population.
In Thai older adults,a waist circumference greater than 80 cm in females and greater than 90 cm in males has been associated with sarcopenia [36].A higher waist circumference reflects a higher proportion of body fat and abdominal obesity[20].Abdominal and visceral fat accumulation stimulates the production of proinflammatory cytokines,which contribute to chronic inflammation and muscle loss [52,69].Previous studies have shown that older adults with larger waist circumferences experience reduced walking speed,which is one of the key indicators used in diagnosing sarcopenia [70].Conversely,in postmenopausal women,higher waist circumferences have been associated with a decreased risk of developing sarcopenia[28].This can be attributed to the fact that abdominal fat stores high concentrations of sex hormones,which have a positive impact on musculoskeletal health [71].
In Thai older adults,a decrease in calf circumference,specifically below 33 cm in women and below 34 cm in men,has been associated with sarcopenia [38].Calf circumference serves as an indicator of muscle mass in the body [72].Previous studies have consistently shown that older adults with higher calf circumferences tend to have muscle mass within the normal range[73-75].In 2019,the AWGS introduced screening tools for potential sarcopenia,beginning with calf circumference measurement.This initial screening step is deemed appropriate for both community and hospital settings[28].These findings suggest that a decrease in calf circumference is associated with sarcopenia.
Type 2 diabetes is found to be associated with sarcopenia in Thai older adults [41].In individuals with type 2 diabetes,there is an elevation in growth hormone levels,while insulin-like growth factor 1 (IGF-1) levels decrease,leading to a reduction in muscle mass and an increase in body fat mass[76].Therefore,maintaining glycemic control is crucial for adequate synthesis of IGF-1,which helps prevent muscle atrophy and loss of muscle mass.Additionally,older adults with type 2 diabetes often experience abnormalities in glucose absorption and metabolism[77,78],along with type 2 muscle fiber atrophy and motor nerve impairment [79].These conditions collectively increase the risk of sarcopenia in older adults with type 2 diabetes.Consistent with previous studies,the prevalence of sarcopenia was found to be higher in older adults with type 2 diabetes compared to those without diabetes [80,81].Specifically,the prevalence of sarcopenia among older adults with type 2 diabetes was 21.4%,whereas it was 15.1%among older adults without type 2 diabetes [80].These findings suggest a higher likelihood of developing sarcopenia among older adults with type 2 diabetes compared to those without the condition.
Depression is found to be associated with sarcopenia in Thai older adults [32,36,37].Older adults with depression experience changes in the body’s hypothalamic-pituitary-adrenal axis,leading to an inflammatory process [82].This results in increased production of IL-6 and TNF-α,which are inflammatory cytokines that contribute to rhabdomyolysis,causing a decline in muscle mass and strength [22,23].Furthermore,older adults with depression often exhibit sedentary behavior and reduced physical activity levels [83,84],which can further contribute to the development of sarcopenia,in line with previous research[85,86].The prevalence rate of sarcopenia was also found to be 5.49 times higher among older adults with depression compared to those without depression[87].These findings highlight the association between depression and sarcopenia,emphasizing the importance of addressing mental health and promoting physical activity in the prevention and management of sarcopenia in older adults.
MCI is found to be associated with sarcopenia in Thai older adults [37].Older adults with MCI often experience reduced physical activity levels [88,89],which is linked to decreased grip strength and slower walking speed [90].Additionally,individuals with impaired brain function may suffer from anorexia,resulting in reduced food intake and malnutrition [91].Consequently,older adults with MCI are at risk of developing sarcopenia due to decreased physical activity and malnutrition.These findings align with previous research indicating an association between MCI and sarcopenia [87,91].The prevalence of sarcopenia was found to be 5.5 times higher in older adults with MCI compared to those with normal cognitive function [87].These results highlight the importance of addressing cognitive impairment and promoting physical activity and proper nutrition to prevent and manage sarcopenia in older adults with MCI.
Malnutrition is strongly associated with sarcopenia in Thai older adults [31,34].When older adults experience malnutrition,their bodies lack sufficient energy and amino acids,which can lead to muscle breakdown and rhabdomyolysis [73].Moreover,malnutrition can cause a deficiency in essential micronutrients like vitamin D and B12,further contributing to muscle loss and functional decline [92,93].It has been observed that older adults with malnutrition are four times more likely to develop sarcopenia compared to those with adequate nutrition [94].These findings emphasize the critical role of proper nutrition in preserving muscle mass and function,underscoring the importance of addressing malnutrition as a preventive measure against sarcopenia in older adults.
Inadequate protein intake and low C-reactive protein levels are strongly associated with sarcopenia in Thai older adults [19,41].Older adults who do not consume enough protein are at risk of muscle mass loss due to reduced muscle protein synthesis,which leads to an imbalance between muscle protein breakdown and synthesis,resulting in negative nitrogen balance and,ultimately,sarcopenia [95].Several systematic reviews and meta-analyses support the notion that inadequate protein intake may contribute to the development of sarcopenia in older adults [96].It is recommended that older adults consume 1.0-1.2 g of protein per kg of body weight daily to maintain and optimize muscle mass,strength,and physical performance [97].By ensuring sufficient protein intake,older adults can support muscle health and mitigate the risk of sarcopenia,thereby maintaining their functional capacity and overall quality of life.
5.Conclusions
The prevalence of sarcopenia among Thai older adults has been observed in various population groups.However,there is considerable variability in the prevalence of sarcopenia among older adults living in the community and outpatient clinics.Limited research is available on the prevalence of sarcopenia in hospitalized older adults,with only a few studies conducted in this context.Therefore,it is important to conduct further investigations to explore the prevalence of sarcopenia in hospitalized individuals.
Multiple factors have been identified as associated with sarcopenia in Thailand,including personal factors such as age and gender,as well as health-related factors such as low physical activity,poor physical ability,prefrailty,BMI,underweight status,waist circumference,calf circumference,type 2 diabetes,depression,mild cognitive impairment,malnutrition,and protein intake.Encouraging appropriate exercise among older adults and ensuring sufficient daily protein intake through counseling and advice can be effective strategies for managing and preventing sarcopenia in Thai older adults.These interventions can help maintain muscle mass and prevent the onset of sarcopenia.This approach should be developed as a guideline in Thailand to achieve the goal of healthy aging.Further studies are needed to investigate interventions,particularly focusing on resistance exercises and protein supplements.
Furthermore,it is crucial to expand the assessment of sarcopenia to encompass all population groups,particularly in primary care facilities and communities.This strategy will contribute to raising awareness and understanding of sarcopenia among the Thai population.Additionally,future studies should investigate changes in the prevalence and risk factors of sarcopenia in Thailand over time to enhance our understanding of this condition and inform effective preventive strategies.
Funding
The research was supported by Ramathibodi School of Nursing,Faculty of Medicine Ramathibodi Hospital,Mahidol University,Thailand.All the funding organizations do not have any roles in the survey’s design,implementation,and analysis.
Declaration of competing interest
The authors have declared no conflict of interest.
Data availability statement
The data generated and scrutinized throughout this study have been integrated into this published article.
CRediT authorship contribution statement
Phatcharaphon Whaikid:Conceptualization,Methodology,Validation,Formal analysis,Investigation,Data curation,Writing -original draft,Writing -review &editing,Visualization,Project administration.Noppawan Piaseu:Conceptualization,Methodology,Validation,Formal analysis,Investigation,Data curation,Writing -original draft,Writing -review &editing,Visualization,Supervision,Project administration.
Acknowledgments
The authors express their gratitude to the Ramathibodi School of Nursing and the Center for Health Promotion and Well-Being,Faculty of Medicine Ramathibodi Hospital,Mahidol University for providing support to facilitate this research endeavor.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2023.11.002.
杂志排行
International Journal of Nursing Sciences的其它文章
- Editorial Board of International Journal of Nursing Sciences
- Chinese Abstract
- Corrigendum to “Relationship between nurses’ perception of professional shared governance and their career motivation in Egypt:A cross-sectional study” [Int J Nurs Sci 10/4 (2023) 485-491]
- 《国际护理科学(英文)》进入中科院分区护理类2 区
- 关于翻译量表使用授权的问答
- Summary of Guide for Authors