Rhegmatogenous retinal detachment in highly myopic eyes with implantable collamer lens
2024-02-23JunLiChongLinChenJiaQingLiXiaoLingLiangChunZhang
Jun Li, Chong-Lin Chen, Jia-Qing Li, Xiao-Ling Liang, Chun Zhang
State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangdong Provincial Key Laboratory of Ophthalmology and Visual Science, Guangzhou 510060, Guangdong Province, China
Abstract
● KEYWORDS: high myopia; implantable collamer lens;rhegmatogenous retinal detachment
INTRODUCTION
Implantable collamer lens (ICL), a highly biocompatible advanced lens material containing a small amount of purified collagen, are widely used to correct vision in eyes with high myopia with or without astigmatism, especially if the cornea is unsuitable for laser refractive surgery[1-2].As a kind of phakic posterior chamber intraocular lens, the ICL is implanted into the eye through a clear corneal incision and finally placed in the ciliary sulcus, correcting the state of refractive error.The greatest advantage of this treatment is its reversibility, enabling the treatment of a much wider range of myopia without permanent modification of the cornea.Particularly, with the development of “Central FLOW Technology”, which allows aqueous humor to flow between the anterior and posterior chambers, the need for pre-operative peripheral iridectomy was eliminated.This new type ICL with a central hole (V4c-ICL) significantly promoted ICL implantation surgery[3-4].
As with all refractive surgeries, ICL implantation surgery preciously corrects the state of refractive error, but does not influence the original condition of the fundus.Eyeballs with high myopia are prone to rhegmatogenous retinal detachment(RRD)[5-6].Thus, the occurrence of RRD in highly myopic eyes that have received ICL implantation deserves serious attention,especially considering the existence of ICL and its potential restrictions to the treatment to RRD[7-8].
At present, there is little information about RRD in highly myopic eyes with ICL due to the low incidence of this condition in these eyes.Here, we present a study which investigated the clinical characteristics, treatment methods and outcomes of RRD in high myopia patients with ICL.
SUBJECTS AND METHODS
Ethical ApprovalThis was a retrospective study that adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Zhongshan Ophthalmic Center, Sun Yat-sen University (2020KYPJ179).Informed consent was obtained from all subjects involved in the study.
SubjectsWe screened the clinical information of all high myopia patients who received treatment for nontraumatic RRD after ICL implantation surgery at the Retinal Department of Zhongshan Ophthalmic Center from Jan 2018 to Dec 2022.The inclusion criteria were as follows: 1) axial length (AL)≥26.5 mm; 2) treatment with laser photocoagulation alone or surgical operations for RRD in the Retinal Department of Zhongshan Ophthalmic Center.The exclusion criteria were as follows: 1) a history of intraocular surgery other than ICL implantation before retinal detachment repair; 2) the presence of any coexisting ocular diseases, such as ocular trauma,cataract, glaucoma, uveitis or any other non-myopia-related conditions, excluding high myopia, at the initial visit; 3) a follow-up time of ≤3mo after treatment for RRD.
Data CollectionClinical data, including age at presentation,sex, refractive errors, AL, and family history, were collected.A complete ophthalmic examination was conducted in the RRD patients, including best corrected visual acuity (BCVA) and intraocular pressure determination, slit-lamp biomicroscopy,and binocular indirect ophthalmoscopy.The retinas of the affected eyes were assessed under mydriatic conditions with a Goldman three-mirror contact lens.Digital fundus photography (Topcon Retinal Camera TRC-50LX, Topcon,Japan) or scanning laser ophthalmoscopy (SLO; Daytona,United Kingdom) was performed.The severity of macular atrophy was identified based on the META-PM classification[9].Ophthalmic findings at presentation included the lens and vitreous status, type and location of retinal holes, status of the macula (on or off), and extent of retinal detachment.
Statistical AnalysisAll categorical variables are expressed as numbers and percentages, and all numerical variables are expressed as the mean±standard deviation.The BCVA was documented with Snellen visual acuity test and then converted to the logarithm of the minimal angle of resolution (logMAR)for statistical analyses.The Wilcoxon signed-rank test was used to statistically evaluate the differences in BCVA before and after treatment.The threshold of thePvalue for statistical significance was <0.05.Statistical analyses were performed with SPSS Statistics version 22 (IBM, New York, USA).
RESULTS
General Data of the Included PatientsIn total, nine highly myopic eyes from nine patients were included in this research.All these patients underwent V4c-ICL implantation before the occurrence of RRD.The mean age was 30.33±7.31y (range,18-40 years old), and there were 2 (22.22%) females and 7(77.78%) males, respectively (female:male=1:3.5).The meantime from ICL implantation surgery to the diagnosis of RRD was 32.44±22.56mo (range, 1-60mo).The mean BCVA was 1.76±1.06 logMAR, and the average AL was 27.80±1.23 mm(range, 26.13 to 29.45 mm).According to the META-PM classification system, 77.78% (7/9), 11.11% (1/9), 11.11%(1/9) and 0 of the eyes were identified as grade C1 (tessellated fundus only), C2 (diffuse chorioretinal atrophy), C3 (patchy chorioretinal atrophy), and C4 (macular atrophy), respectively.The demographic information is summarized in Table 1.
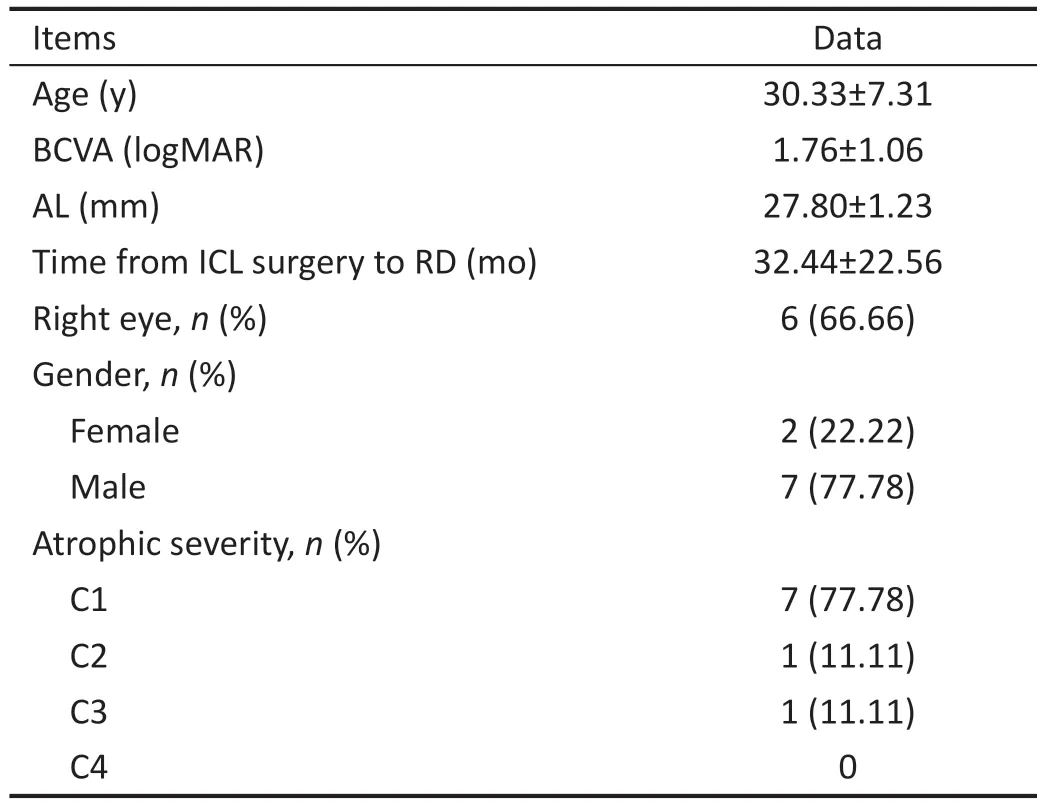
Table 1 Demographic information for nine eyes from nine included patients mean±SD
Fundus Features of the Included Eyes with Rhegmatogenous Retinal Detachment at DiagnosisThe types of retinal breaks were diverse.Giant retinal tear (GRT) was detected in 33.33% (3/9) of eyes, horseshoe tear in 33.33% (3/9) of eyes,simple round hole in 22.22% (2/9) of eyes, and horseshoe tear combined with round hole in 11.11% (1/9) of eyes (Figure 1).The area of retinal detachment was less than 1 quadrant in 1 eye (11.11%), between 1 and 2 quadrants in 3 eyes (33.33%),and more than 2 quadrants in 5 eyes (55.56%).At the initial visit for RRD diagnosis, fundus examinations revealed macula-off status in 88.89% (8/9 eyes) of eyes.Moreover,choroidal detachment was detected in 2 eyes (22.22%).The characteristics of the RRD eyes at diagnosis are shown in Tables 2 and 3.
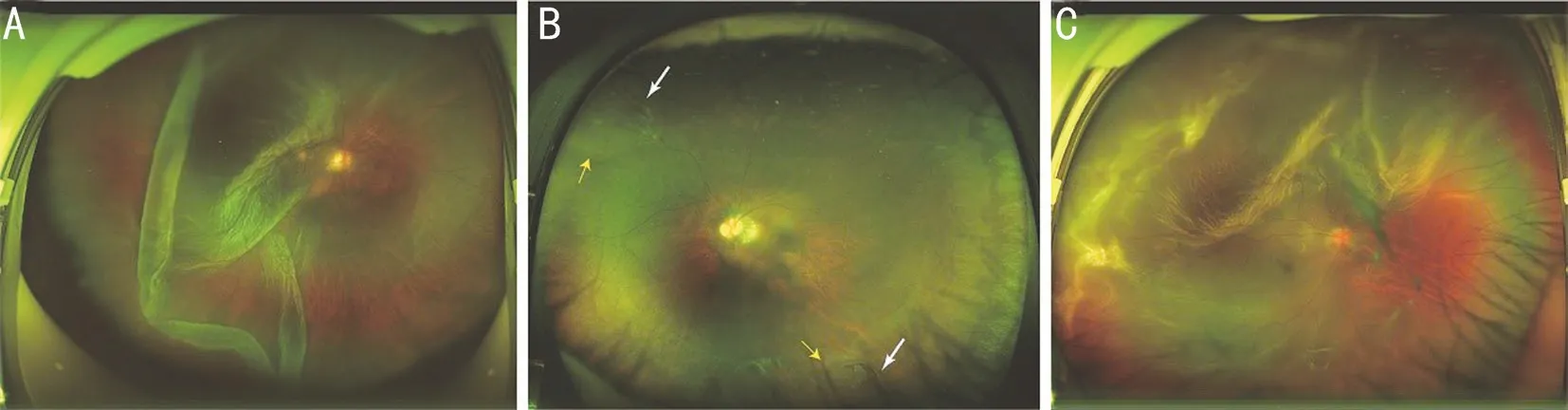
Figure 1 Representative images showing three types of retinal breaks in RRD eyes with high myopia received ICL implantation: GRT,horseshoe tear, and atrophic round hole A: GRT in the right eye of a 33-year-old male patient.Fundus photography detected a GRT located in the temporal retina with a rolled back posterior edge.The scope of retinal detachment exceeded two quadrants, and the macula was involved.B: Horseshoe tears in the left eye of a 28-year-old male patient.Two horseshoe tears were located in the supranasal and inferotemporal periphery.The white arrows and yellow arrows indicate the horseshoe tear and the scope of retinal detachment, respectively.C: Atrophic round holes in the right eye of an 18-year-old male patient.Fundus photography revealed two small round holes located in the temporal periphery with extensive retinal detachment.RRD: Rhegmatogenous retinal detachment; ICL: Implantable collamer lens; GRT: Giant retinal tear.

Table 2 Fundus features of included eyes at the diagnosis of rhegmatogenous retinal detachment
Management and Treatment Outcomes of the Included Eyes with Rhegmatogenous Retinal DetachmentRRD was effectively controlled after surgical treatment in eight patients and by retinal laser photocoagulation alone in one patient due to his limited scope of retinal detachment.Two eyes (22.22%)underwent pars plana vitrectomy (PPV) combined with C3F8tamponade.PPV combined with silicone oil tamponade was performed in four eyes (44.44%), and a second silicone oil tamponade was performed in two of these eyes for the recurrence of retinal detachment.Scleral buckling with and without PPV was performed in one eye each.The ICL was removed from 22.22% (2/9) of the eyes during the course of the treatment for RRD.All patients who underwent silicone oil tamponade operation had the silicone oil completely removed for at least 3mo at the last visit, with no recurrence of retinal detachment.At the final follow-up, the mean BCVA (logMAR)improved significantly from 1.76±1.06 at presentation to 0.81±1.01 (P=0.035), and no case of recurrent retinal detachment was found (Table 3).
DISCUSSION
The new type of ICL (V4c-ICL) has been widely used for the correction of high-degree myopia.Compared with previous types of ICL, the V4c-ICL has been reported to reduce the risk of anterior segment complications, such as cataract formation,anterior capsular opacification, and secondary glaucoma,which significantly promote ICL implantation surgery in recent years[10-11].Remarkably, however, RRD after ICL implantation deserves serious attention because of the potential for severe vision impairment and unsatisfactory therapeutic effects.Thus,it is of great importance to evaluate the clinical characteristics and long-term treatment outcomes of RRD in high myopia patients who have received ICL implantation, which will enable a deeper understanding of this condition.
One of the findings in our data is that 22.22% (2/9) of the RRD eyes was due to round atrophic holes.Studies have shown that round atrophic hole located in sites with lattice degeneration is an important cause of phakic retinal detachment, usually in the peripheral retina[12-13].Our results suggest that timely comprehensive examination, especially of the peripheral retina,should be strictly conducted in highly myopic eyes pre- and post-ICL implantation.
Another interesting finding in our study is that 33.33% (3/9) of the RRD eyes had GRT.GRT is a full-thickness neurosensory retinal break, which extending for 90° or more in the presence of posterior vitreous detachment and is estimated to be the cause of RRD in 0.5% to 8.3% of cases.Over half (55%-60%)of all GRTs are judged to be idiopathic, and 9% of those are caused by high myopia when the vitreous body detaches from the retina, creating a retinal tear of a certain size[14-15].Therefore,we suggest that in addition to examining the peripheral retina,examination for peripheral vitreous degeneration is also of great importance.Studies have also revealed that GRT is closely associated with a high rate of silicone oil tamponade and an unsatisfactory reattachment rate after retinal detachment surgery, which is supported by our data[16-17].In this study,persistent retina reattachment was achieved after two times of silicone oil tamponade in 66.66% (2/3) of RRD eyes caused by GRT.
Currently, few reports on the surgical treatment of RRD in highly myopic eyes with ICL exist.The management of intracapsular artificial lens during retinal detachment repair surgery in the eyes previously treated with cataract surgery has been controversial[18-19].The presence of an artificial lensmay impede the identification of retinal breaks and removal of the artificial lens may improve intraoperative visualization and surgical success.In this study, primary surgical success with ICL preservation was achieved in 6 eyes, highly up to 75%.The two eyes that developed recurrent retinal detachment and required ICL removal in the second surgery both had GRT-associated RRD.In our opinion, the reason for this phenomenon might be the need for complete vitrectomy of the peripheral retina and ora serrata in GRT-associated RRD,which is opposed by the existence of an ICL.
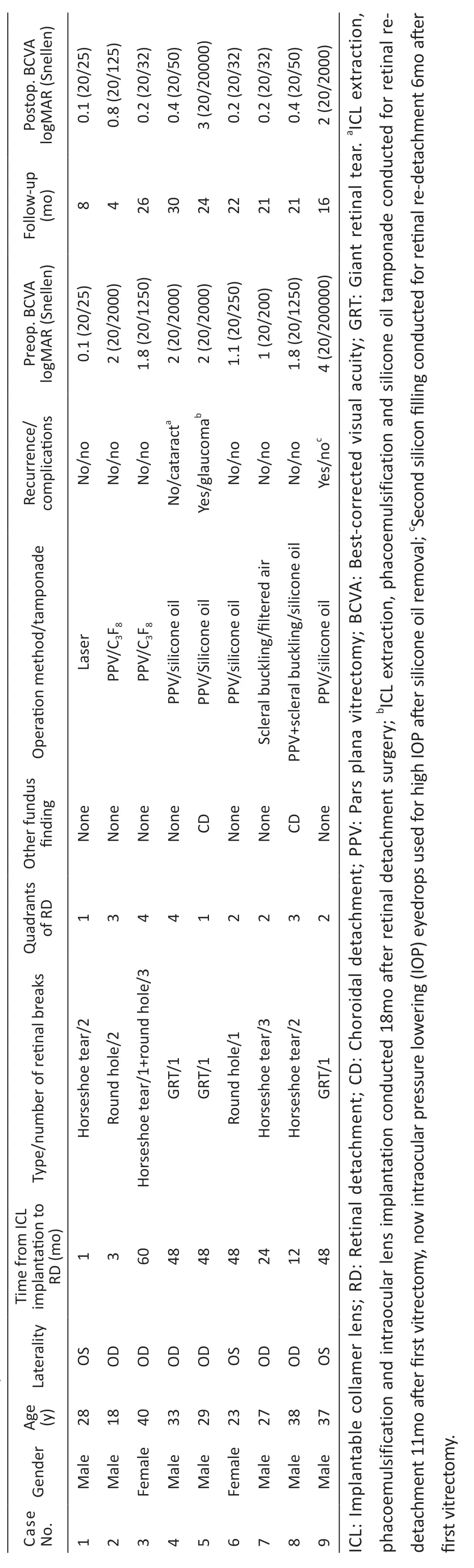
Table 3 Characteristics, treatment methods and outcomes
There are several limitations to our study.First, as RRD in high myopia patients with ICL is considerably rare, the number of patients included in this study was limited and thus did not allow determination of the statistical significance of the potential impact of certain factors.Second, referral bias was likely unavoidable because our hospital is a tertiary referral institute for eye diseases.Thus, further investigation in a larger number of patients from multiple medical institutions might produce more meaningful results.
Several studies published in recent years have revealed that ICL implantation is a safe and effective surgery for correcting high myopia, and even present better visual quality in comparison of corneal refractive surgery[20-22].To the best of our awareness, this study is the first to systematically present the clinical information, including the treatment methods and outcomes, of RRD in highly myopic eyes with ICL.
In this study, the morphologic appearance of retinal breaks in highly myopic eyes previously underwent ICL implantation is diverse.Persistent retinal reattachment was achieved in 7 eyes(77.78%) after the primary treatment and in 2 eyes (22.22%)after a second surgery.In most of our patients, the ICL could be preserved during the course of the treatment for RRD.In addition, we believe that lifelong fundus monitoring in highly myopic eyes with ICL is significant.
ACKNOWLEDGEMENTS
Foundation:Supported by the Fundamental Research Funds of the State Key Laboratory of Ophthalmology(No.303060202400201203).
Conflicts of Interest:Li J,None;Chen CL,None;Li JQ,None;Liang XL,None;Zhang C,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Using choroidal thickness to detect myopic macular degeneration
- lmpact of multifocal gas-permeable lens designs on short-term choroidal response, axial length, and retinal defocus profile
- Baerveldt glaucoma implant with Supramid© ripcord stent in neovascular glaucoma: a case series
- Efficacy and safety of Usights UC100 illuminated microcatheter in microcatheter-assisted trabeculotomy
- Quantifying peripapillary vessel density and retinal nerve fibre layer in type 1 diabetic children without clinically detectable retinopathy using OCTA
- Nomogram to predict severe retinopathy of prematurity in Southeast China
