Efficacy and safety of Usights UC100 illuminated microcatheter in microcatheter-assisted trabeculotomy
2024-02-23ShuoYuKeXuChunZhang
Shuo Yu, Ke Xu, Chun Zhang
1Department of Ophthalmology, Peking University Third Hospital, Beijing 100191, China
2Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Peking University Third Hospital, Beijing 100191, China
Abstract
● KEYWORDS: illuminated microcatheter; microcatheterassisted trabeculotomy; primary open angle glaucoma
INTRODUCTION
Conventional trabeculotomy, a standard surgical procedure in ophthalmology, involves the use of metal trabeculotomy instruments to open approximately 180 degrees of the Schlemm’s canal during a single session.To overcome the limitations of conventional surgeries[1], a 360-degree trabeculotomy was proposed[2].The concept of 360-trabeculotomy was first introduced in 1960, utilizing a polypropylene suture and direct gonioscopy lens to visualize the travel of the suture through the Schlemm’s canal[3].However, threading a suture around Schlemm’s canal poses a risk of misdirection into the suprachoroidal space, leading to potential complications[4-5], particularly in cases with corneal edema or opacification[6-7].In recent advancements,illuminated microcatheter-assisted trabeculotomy, using a non-traumatic tip illuminated microcatheter (iTrack 250A;iScience Interventional, Menlo Park, CA, USA), has emerged as a promising technique.It has shown comparable success to suture trabeculotomy while significantly reducing the risk of false passage[8-9].The illuminated microcatheter aids in direct and sustained visualization of Schlemm’s canal,enabling safe and complete circumferential trabeculotomy with minimized complications[10-13].A new illuminated microcatheter, the Usights UC100, independently developed and designed by Tianjin Gifted Ophthalmology Technology(Tianjin, China), has recently been registered and approved for use in China.With similar basic parameters to the iTrack 250A microcatheter, the Usights UC100 offers a substantial cost reduction, making it potentially accessible for wider adoption.This study aims to assess the safety and effectiveness of Usights UC100 microcatheters in microcatheter-assisted trabeculotomy, comparing its performance to that of the iTrack 250A.
SUBJECTS AND METHODS
Ethical ApprovalThe Ethics Committee of Peking University Third Hospital approved the study, the approval number is(2023) Medical Ethics Review (No.243-01).A consent waiver was approved by the ethics committee, and all participants did not receive the stipend.
This study was conducted retrospectively on patients diagnosed with primary open angle glaucoma (POAG),who underwent microcatheter-assisted trabeculotomy using either the illuminated microcatheter iTrack 250A (iScience Interventional, USA) or Usights UC100 (Tianjin Gifted Ophthalmology Technology, China) between November 2019 and July 2022 at Peking University Third Hospital in Beijing,China.Patients with bilateral or unilateral POAG were included in the analysis if they exhibited consistent clinical features, such as elevated intraocular pressure (IOP), an open and normalappearing anterior chamber angle, glaucomatous cupping of the optic nerve, and visual function loss on perimetry.IOP was measured using Goldmann applanation tonometry before the surgery and during follow-up examinations.
A comprehensive preoperative evaluation was performed on all patients to record their baseline characteristics, and the surgical procedures were conducted under topical anesthesia by a single non-masked surgeon.
The microcatheter-assisted trabeculotomy procedure has been previously described in the literature[14-15].In summary, the surgical approach involved a conjunctival peritomy, followed by the identification and de-roofing of Schlemm’s canal through the creation of superficial and deep scleral flaps.The microcatheter was then inserted into the canal and carefully threaded circumferentially around it, with direct transscleral visualization of the microcatheter tip.Subsequently,circumferential trabeculotomy was performed by gently pulling the two ends of the catheter.The scleral flaps and peritomy were meticulously closed using interrupted and interlocking 10-0 monofilament nylon sutures, respectively.
A standardized postoperative regimen was administered to both groups, which included topical pilocarpine nitrate along with steroid-antibiotic drops in tapering doses for four weeks.Patients were scheduled for follow-up visits on 1, 7d, 1, and 3mo to assess best-corrected visual acuity (BCVA), IOP, and slit lamp examination findings.If elevated IOP was observed during the follow-up, appropriate topical anti-glaucoma therapy was initiated, and the cases were closely monitored.
The success criteria for the surgical procedure were defined as follows: a postoperative IOP of less than 22 mm Hg and a reduction of more than 30% from the preoperative level, along with clinical glaucoma stability.Successful cases should not require further IOP-lowering surgical intervention or oral IOPlowering medication, and they may or may not require the use of topical medications.During the surgery, any intraoperative complications were carefully noted such as hyphema, iris or lenticular damage, Descemet’s membrane detachment, and any microcatheter-related problems like misdirection.These criteria and recorded complications were used to evaluate the overall success and safety of the microcatheter-assisted trabeculotomy procedure.
After each surgery, the surgeon completed an “ease of use”questionnaire to evaluate various aspects of the procedure related to the illuminated microcatheter.The questionnaire assessed the ease of use in terms of three key factors.Insertion:the ease of inserting the microcatheter into Schlemm’s canal; Visualization of the microcatheter tip: how well the surgeon could visualize the tip of the microcatheter during the procedure; Cutting force: the cutting force of the microcatheter while performing the circumferential trabeculotomy.
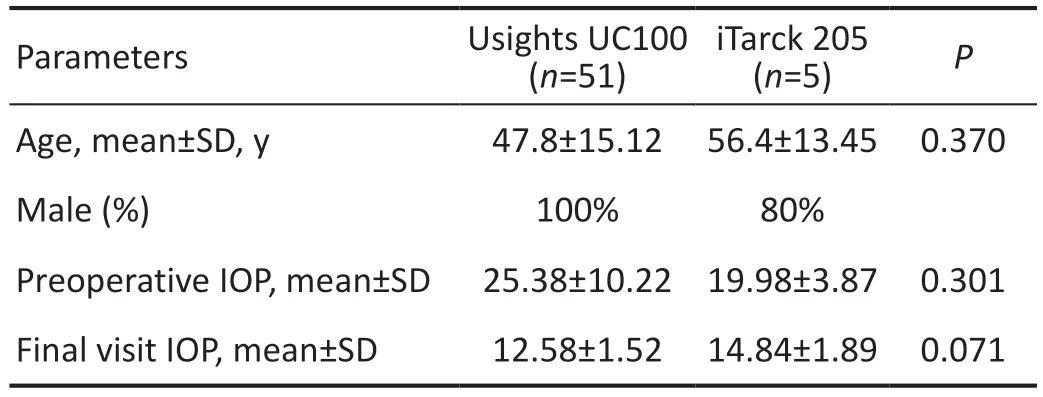
Table 1 Demographic and ocular characteristics
The questionnaire used a five-point Likert Scale for rating the responses, with the following scale: 1-strongly disagree,2-disagree, 3-neither agree nor disagree, 4-agree, 5-strongly agree.By using this Likert Scale, the surgeon provided subjective ratings for each of the specified factors, allowing for a quantitative assessment of the ease of use of the illuminated microcatheter in the surgical procedure.These ratings were then used to evaluate the overall user experience and satisfaction with the microcatheter-assisted trabeculotomy technique.
Statistical analysis was performed with SPSS for Windows version 27 (SPSS Inc., Chicago, IL, USA).Demographic and clinical characteristics between the groups were compared using thet-test.Quantitative variables were compared using independentt-test.A two-sided Wilcoxon signed-rank test was used for comparing the scoring of the “ease-of-use”.
RESULTS
A total of 10 eyes of 10 patients were included, 5 in each group.A summary of the demographic data and ocular parameters is given in Table 1.
Intraoperative and Immediate Postoperative CourseComplete catheterization was achieved in all eyes.Mild and transient hyphema was observed in all five eyes in Usights UC100 group and 3 eyes in iTrack 250A group, of which all resolved spontaneously at 1wk follow-up.The incidence of hyphema was significantly greater in Usights UC100 group compared to iTrack 250A group.Shallow anterior chamber was not noted in any of the eyes in either group.One eye in Usights UC100 group presented with mild dilation of pupil (6 mm) and was slightly improved (5 mm) at 3mo follow up.
Success RateAll patients in both groups underwent a complete 360-degree trabeculotomy with the iTrack 250Amicrocatheter or the Usights UC100 microcatheter.For the Usights UC100 group, the average IOP decreased from 25.38±10.22 mm Hg preoperatively to 12.58±1.52 mm Hg at 3mo post-operation follow-up (Figure 1), a mean overall 50.43% IOP reduction (P=0.024).Mean IOP decreased from 19.98±3.87 mm Hg in iTrack 250A group to 14.84±1.89 mm Hg at 3mo, a mean overall 25.73% IOP reduction (P=0.028).The percentage of IOP reduction showed no significance between the two groups (Figure 2).

Table 2 Comparison of ease-of-use scores

Figure 1 Comparison of mean intraocular pressure (IOP) between Usights UC100 group and iTrack 250A group at 3mo.

Figure 2 Box-and-whiskers plots showing the percentage of intraocular pressure (IOP) reduction across treatment groups(P=0.115).
One patient in iTrack 250A group required oral medication to control IOP at 1wk follow-up.None of the patients required secondary surgery.At 3mo follow-up, success was achieved in 100% (5/5) and 80% (4/5) eyes in Usights UC100 group and iTrack 250A group.
Assessment of Ease-of-useThe Usights UC100 received a slightly higher score of insertion than the iTrack, but there was no statistical significance (P=0.785).The two devices showed no significant difference in the ease of use of achieving a satisfactory visualization of the microcatheter tip and performing the circumferential trabeculotomy (P=1).
DISCUSSION
The primary regulation of IOP is primarily attributed to the outflow system.In both normal eyes and glaucomatous eyes,the removal of the trabecular meshwork resulted in significant reductions in outflow resistance.In normal eyes, trabecular meshwork removal led to a 75% reduction in outflow resistance, while in glaucomatous eyes, it removed abnormal resistance[16-17].
In our single-surgeon retrospective study, we observed a significant reduction in IOP in patients with POAG who underwent illuminated microcatheter-assisted trabeculotomy during the 3-month follow-up period.
Specifically, in the Usights UC100 group, we found a substantial IOP reduction of 50.43%.This exceeded the IOP reduction rate observed in the iTrack 250A group, which was 25.73%.Although the difference in IOP reduction between the two groups did not reach statistical significance, both groups experienced a meaningful reduction in IOP, which indicates the potential effectiveness of the illuminated microcatheterassisted trabeculotomy in managing POAG.
Furthermore, we also assessed the success rates of the two groups based on the defined criteria.The Usights UC100 group demonstrated a higher success rate, with all cases (100%)meeting the success criteria.In contrast, the iTrack 250A group had a success rate of 80%, indicating that illuminated microcatheter-assisted trabeculotomy with Usights UC100 had a better overall success rate in our study population.
These findings suggest that illuminated microcatheterassisted trabeculotomy, particularly with the Usights UC100 microcatheter, may be a promising approach for reducing IOP and achieving a higher success rate in patients with POAG.However, further studies with larger sample sizes may be necessary to validate these findings and establish statistical significance for the observed differences between the two microcatheter groups.
Mild and transient hyphema was observed in all five eyes in the Usights UC100 group and in three eyes in the iTrack 250A group.Fortunately, all cases of hyphema resolved spontaneously by postoperative day 7.Hyphema has been identified as a common postoperative complication following microcatheter-assisted trabeculotomy, with previous studies reporting its occurrence in 90%-100% of postoperative patients[18-19].Hyphema is a result of blood reflux from the aqueous veins through the Schlemm’s canal, instead of being considered a complication, hyphema can be seen as a positive sign of successful angle opening[20].The presence of blood reflux in the Schlemm’s canal after successful microcatheterassisted trabeculotomy indicates proper drainage of the distal pathway and suggests adequate control of IOP in patients with POAG.Notably, the blood observed in the Schlemm’s canal is seen to drop from a point in the original trabecular meshwork region, indicating that tissue remodeling occurs in the margin where the trabecular meshwork was dissected during microcatheter-assisted trabeculotomy[21].This observation further supports the notion that hyphema is not a complication but rather a positive indication of the success of the procedure.Overall, the occurrence of mild and transient hyphema after microcatheter-assisted trabeculotomy in our study is consistent with previous findings and is associated with successful angle opening and adequate IOP control in patients with POAG.
Both the Usights UC100 microcatheter and the iTrack 250A microcatheter demonstrated satisfactory visualization during the surgery, attributed to the illuminated tip continuously guiding the catheter within the Schlemm’s canal.This precise visualization and guidance significantly reduced the likelihood of complications caused by misdirection and tissue disturbance, thus ensuring the safety of the microcatheterassisted trabeculotomy procedure[22-23].Moreover, the use of an illuminated microcatheter for trabeculotomy also contributed to a reduction in the incidence of complications typically associated with conventional full-thickness trabeculotomy.Complications such as shallow anterior chamber and late hypotony, which can be problematic in conventional surgeries,were notably absent in our study for both microcatheter groups[24-26].The absence of these severe adverse effects further highlights the benefits and safety of the illuminated microcatheter-assisted trabeculotomy technique.The illuminated microcatheter’s ability to facilitate precise and controlled canal access while minimizing tissue disturbance played a crucial role in avoiding these complications and achieving positive surgical outcomes for patients with POAG.Glaucoma is not only a vision-related condition but also has significant impacts on the psychological, socioeconomic,and functional well-being of patients.The disease burden of glaucoma extends beyond vision loss, affecting various aspects of patients’ lives and overall quality of life[27-28].The availability of a cheaper and more affordable instrument, such as the Usights UC100 illuminated microcatheter, could play a crucial role in easing the burden of glaucoma on patients and society as a whole[29-30].Lowering the cost of essential medical equipment can reduce the financial strain on patients, making the treatment more accessible and affordable.This, in turn, can lead to improved patient compliance with treatment regimens and follow-up visits, resulting in better overall management of glaucoma and potentially preventing or delaying disease progression.Additionally, by reducing the indirect and societal costs associated with glaucoma care, a more affordable instrument like the Usights UC100 microcatheter can benefit healthcare systems and society at large.Patients may experience fewer financial barriers to accessing appropriate care, leading to earlier diagnosis and intervention, which can be critical in preserving vision and preventing further complications.
The present study indeed acknowledges some limitations that should be considered when interpreting the results.One such limitation is the relatively small number of patients included in the study.A larger sample size would provide more robust and generalizable findings, allowing for better statistical power and more accurate assessments of the outcomes.Another limitation is the short follow-up period.Longer follow-up periods would enable a more comprehensive evaluation of the long-term effects of using different illuminated microcatheters for trabeculotomy.This would provide valuable insights into the sustainability of the treatment effects and potential late complications.It is essential to consider the overall success of the primary surgery and the potential implications for longterm outcomes.However, the short follow-up period may not capture all potential late complications or variations in treatment effects over time.To address these limitations and gain a more comprehensive understanding of the outcomes,future studies with larger sample sizes and longer follow-up periods could provide valuable insights into the efficacy and safety of different illuminated microcatheters for trabeculotomy in patients with POAG.
Based on the findings of our study, it is evident that performing microcatheter-assisted trabeculotomy using either the illuminated microcatheter (Usights UC100) or the iTrack 250A microcatheter yielded comparable efficacy in terms of IOP reduction.Additionally, both microcatheters demonstrated similar safety profiles in eyes with POAG.
However, a noteworthy advantage of the Usights UC100 microcatheter is its potential cost-effectiveness.Being a cheaper and more affordable option, the Usights UC100 microcatheter can help reduce the financial burden on patients and healthcare systems.This accessibility could promote broader adoption of the microcatheter-assisted trabeculotomy technique, making it more widely available to patients with POAG.
In summary, both the illuminated microcatheter (Usights UC100) and the iTrack 250A microcatheter offer comparable efficacy and safety in microcatheter-assisted trabeculotomy for POAG.The Usights UC100 microcatheter stands out as a potentially more cost-effective option, which may benefit patients and healthcare providers alike.
ACKNOWLEDGEMENTS
Foundations:Supported by the Clinical Medicine Plus X-Young Scholars Project, Peking University (No.PKU2020LCXQ023); National Natural Science Foundation of China (No.82101107).
Conflicts of Interest:Yu S,None;Xu K,None;Zhang C,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Using choroidal thickness to detect myopic macular degeneration
- lmpact of multifocal gas-permeable lens designs on short-term choroidal response, axial length, and retinal defocus profile
- Baerveldt glaucoma implant with Supramid© ripcord stent in neovascular glaucoma: a case series
- Quantifying peripapillary vessel density and retinal nerve fibre layer in type 1 diabetic children without clinically detectable retinopathy using OCTA
- Nomogram to predict severe retinopathy of prematurity in Southeast China
- Effect of aflibercept combined with triamcinolone acetonide on aqueous humor growth factor and inflammatory mediators in diabetic macular edema
