Ophthalmic exam and ophthalmology residents’subspecialty preference
2024-02-23AriLeshnoDafShalevDaphnaLandauPrat
Ari Leshno, Daf Shalev, Daphna Landau Prat
1Goldschleger Eye Institute, Sheba Medical Center, Tel Hashomer 5262000, Israel
2Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv 6997801, Israel
3Department of Ophthalmology, Edith Wolfson Medical Center, Holon 5822012, Israel
Abstract
● KEYWORDS: residency; subspecialty; ophthalmic examination; career choice; ophthalmology
INTRODUCTION
Professional training of ophthalmology residents begins with early acquisition of basic skills that are relatively new to the medical graduate, since most of the medical curriculum focuses upon internal medicine and general surgery.Toward this end, residents are required to learn the use of various unique diagnostic and imaging tools which have become standard of care in the 21stcentury.Mastering the various aspects of a comprehensive ophthalmic examination has a learning curve individual to each ophthalmic resident.These tests differ in various aspects: some require patient cooperation, such as visual acuity assessment, while others require special equipment, such as a gonio lens for gonioscopy or Goldmann’s 3-mirror lens for evaluation of the peripheral retina.Few may be technically challenging for the young resident, such as using an indirect ophthalmoscope for optic nerve and retina examinations.Finally, parts of the exam can be relatively cumbersome for the patients, such as posterior segment evaluation.
A physician’s degree of comfort and confidence in performing a certain task might provoke either aversion or proneness[1].While a complete set of these skills is required by all residents in order to become ophthalmic specialists, some are more routinely performed in the setting of certain subspecialties.For example, the use of an indirect ophthalmoscope is more wildly used by retina specialists, while evaluation of ocular movement is commonly performed by pediatric ophthalmology and strabismus specialists.Therefore, residents’ perceptions or apprehension towards executing the various tasks might influence their decision in choosing a subspecialty, by inclining to select those perceived as being associated with a more comfortable clinical examination or with clinical skills that are relatively easier to acquire[2].
Our study evaluated the perceptions of ophthalmology residents toward the ophthalmic examination as a whole and towards its various components.Our goal was to assess the correlation between those perceptions and their choice for future subspecialty, while identifying the major influencing factors.
SUBJECTS AND METHODS
Ethical ApprovalAll authors declared no financial or nonfinancial conflict of interest, and the questionnaire was anonymous, therefore no formal consent to participate was required.The study was approved by the Sheba Medical Center Institutional Review Board.
An anonymous questionnaire was sent to all ophthalmology residents in Israel during November 2019.The sections of the questionnaire were: 1) demographic data including current stage in residency; 2) information relating attitude and perceptions to the various aspects or components of the ophthalmic examination; 3) prospects of future subspecialization and the influence that the perceptions of the ophthalmic exam on this choice.The respondents were asked to rank on a Likert scale how much they liked or disliked performing 13 different aspects of the ophthalmic exam including: evaluation by 1) slit-lamp of the anterior segment, 2) slit-lamp of the posterior segment, 3) visual acuity testing, 4) applanation tonometry, 5) gonioscopy, 6) evaluation of a relative afferent pupillary defect (RAPD), 7) indirect ophthalmoscopy, 8) evaluation of ocular movement, 9) use of Goldmann 3-mirror lens, 10) refraction, 11) color vision exam, 12) confrontational visual fields exam, 13) corneal scraping.In addition, they were asked to rank the contribution of each of the following factors to their decisions: 1) need for patient cooperation, 2) time required, 3) technical difficulty, 4)reliability, 5) patient discomfort, 6) requirement for special equipment, 7) fear of missed or wrong diagnosis, 8) need for acquired skill to perform correctly.Lastly, the residents were asked to select which subspecialties they considered for their future careers and whether they felt their choice correlated to their ranking of certain ophthalmic exam components.
Statistical AnalysisData were analyzed using IBM SPSS statistics (IBM SPSS for Windows, version 25).Significance was defined as an alpha error probability <0.05.The Chisquared test was used for comparison of categorical variables and Student’st-test and One-way ANOVA were used for comparison of continuous variables.Multivariate logistic regression analysis was applied as needed to detect interactions between variables and to exclude confounder effects.

Figure 1 Residents’ rankings of individual ophthalmic exam components.
RESULTS
Eighty residents (38 females, 42 males) responded to the questionnaire (over one-half of the residents in the country at the time).Their mean age was 33.6y [standard deviation (SD) 3.4].The respondents were in residency for a mean of 2.5y (SD 1.7).Figure 1 summarizes the responders’ perceptions of each component of the ophthalmic exam.Slit-lamp examination of the anterior segment received the highest score (i.e., the most liked component) followed by slit-lamp examination of the posterior segment and evaluation for RAPD.Gonioscopy and evaluation of extraocular muscles received the lowest scores(i.e., most disliked components) followed closely by visual acuity testing and use of the Goldmann 3-mirror lens.
No significant differences were observed between male and female responders, with the exception of refraction and gonioscopy which were more disliked by female responders(mean difference 0.6±0.26,P=0.024 and 1.1±0.24,P<0.001 respectively).A significant negative correlation was found between responders’ age and years in residency and ranking of gonioscopy, evaluation of extraocular muscles and refraction.Use of Goldman’s 3-mirror lens and indirect ophthalmoscopy correlated only with responders’ age.
Figure 2 depicts the average score given to each of the 8 factors contributing to the ranking of examination components.Need for patient cooperation was considered by the majority of responders as an important factor (63/80, 78.8%).Technical difficulty and time consumption were also considered important by over one-half of the responders (48/80, 60%).Conversely, the need for special equipment and the patient’s experience were considered important by the fewest number of responders (16/80, 20% and 21/80, 26.3% respectively).
Males gave a lower ranking to the need for skill proficiency and fear of wrong diagnosis than females (P<0.05).Responder’s age correlated significantly with a lower ranking assigned to the importance of examination time (Pearson’s correlation 0.273,P=0.017), technical difficulty (0.393,P<0.001), skill (0.351,P=0.002), and fear of wrong diagnosis(0.447,P<0.001).

Figure 2 Contribution of selected factors in the ranking of the individual ophthalmic examination components.
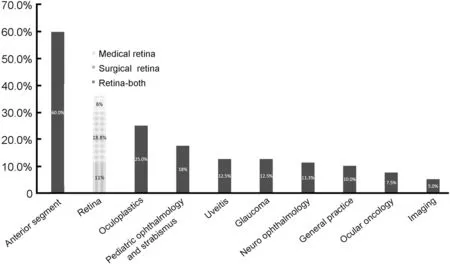
Figure 3 Distribution of future career preferences among the residents.
Effect on Future Career ChoicesPreferences regarding future career plans are presented in Figure 3.The most popular choices for subspecialty were anterior segment (48/80, 60%),retina (29/80, 36.25%, of which 15 considered a surgical fellowship, 5 considered a medical fellowship and 9 both)and oculoplastics (20/80, 25%).Twenty-seven (27/80, 33.2%)responders considered only one future career option, nearly one-half of whom chose an anterior segment fellowship(13/27, 48.1%).A very small overlap was noted between responders considering an anterior segment fellowship and those considering a pediatric-strabismus fellowship (P=0.030),as well as between responders considering a retina fellowship and an oculoplastics fellowship (P=0.031).
Overall, the majority of responders (49/80, 61.3%) stated that there was a direct correlation between the ranking of certain ophthalmic exam components and their future career choices.Responders who were considering a career in an anterior segment subspecialty gave a significantly higher ranking(liked) to the anterior segment examination in comparison to responders not considering that career path (P=0.006).A subset of responders who chose an anterior segment subspecialty as the only career option gave a significantly higher ranking to both gonioscopy and refraction (Figure 4A).Responders considering a career in retina (surgical or medical) gave a significantly higher ranking to posterior segment evaluation by slit-lamp or indirect ophthalmoscope, and a significantly lower ranking to aspects related to neurologic evaluations(Figure 4B).Responders considering a career in oculoplastics gave a significantly lower ranking to slit-lamp evaluation of the posterior segment and a significantly higher ranking to performing corneal scraping (Figure 4C).Responders considering a career in pediatric ophthalmology gave a significantly lower ranking to slit-lamp examination of the anterior segment (P=0.040).
Responders’ age, sex, and years in residency had no significant effect on the reported career preferences.The multivariate logistics regression model found that the ranking of the anterior segment aspect of slit-lamp examination was the only significant factor associated with responders’ choosing an anterior segment fellowship as their sole future career choice.The multivariate regression model for selecting a future career in retina found a positive association with posterior segment evaluation by both slit-lamp and indirect ophthalmoscope.Among the aspects in which a negative ranking was associated with a future career in retina in the univariate analysis, only evaluation of extraocular muscles was found to be statistically significant in the multivariate model.
DISCUSSION
In this study, we found that anterior and posterior segment slit-lamp examinations were the most likeable components of the ophthalmic exam, whereas gonioscopy, ocular motility evaluation and visual acuity assessment were least favored.There was a significant association between the perception of certain aspects of the ophthalmic exam and their related subspecialty fields.Forty-nine (61.3%) of the respondents noted a direct correlation between their perception of the ophthalmic exam components and their choice of subspecialty.Correspondingly, anterior segment and retina subspecialties were the most sought-after ones.The most significant factor contributing to a negative perception of an exam component was the need for patient cooperation, while special equipment and patient discomfort were ranked as least significant.
The findings from this study provide new insight into residents’ perceptions toward the ophthalmic examination.By gaining a deeper insight into the specific challenges that residents encounter during the ophthalmic exam, we were able to pinpoint areas in need of innovation and enhancement.While there has been prior research that focused on assessing residents’ clinical performance, to the best of our knowledge,this is the first investigation of residents’ perceptions of the clinical examination process.We also explored various implications of our findings in connection with earlier publications on this topic.

Figure 4 Ranking of ophthalmic examination components in a subset of residents considering pursuing a fellowship in anterior segment (A),retina (B) or oculoplastics (C) Indirect: Indirect ophthalmoscopy; RAPD: Relative afferent pupillary defect; CV: Color vision; CVF: Confrontational visual fields; EOM: Extraocular movement.
Perception of the Ophthalmic ExaminationPrevious reports support our findings of resident preferences towards certain components of the ophthalmic examination[3].The least likeable components in our study were gonioscopy, ocular motility testing and visual acuity testing.Mihlstinet al[4]found low compliance for performing gonioscopy.Quigleyet al[5]also observed that residents performed gonioscopy on only 50% of open angle glaucoma patients.In another study aimed to evaluate residents’ perception of gonioscopy, 20% of them stated they were not confident in performing the exam[6].These findings are consistent with gonioscopy having received the lowest overall ranking in our cohort.
Following gonioscopy, ocular motility testing and visual acuity assessment were the next least liked aspects of the ophthalmic examination.This might be due to the difficulty of performing pediatric evaluations or the residents’ perception of their training.Parija and Mahajan[2]reported that the ocular examination in children is commonly perceived as difficult and requiring a great deal of patience.In accordance, 63 (78.8%)of the residents in our study responded that the need for patient cooperation was the most significant factor contributing to a negative perception of an exam component.Gogateet al[7]found that a majority of young ophthalmologists felt they received poorer training in refraction, orthoptic evaluation and pediatric visual acuity testing compared to other ophthalmic exam components.Residents may not yet feel comfortable with certain examination techniques, particularly early in their training period, and as a result elect to abstain from performing them when given the choice.
In our study, most of the lower-ranking examination components were those less frequently performed.Unlike the slit-lamp examination, which is the mainstay of routine ophthalmic evaluation, gonioscopy, ocular motility testing and Goldman’s 3-mirror lens exams are performed only when indicated.Residents might rank gonioscopy low due to some degree of aversion, resulting from a lack of experience and a lower level of confidence.Conversely, residents may rank slit-lamp examination high due to increased comfort in performing, resulting from greater experience, improved skills and confidence.However, this relationship of performance frequency and likeability does not explain why visual acuity testing, a frequently performed examination component, was ranked third lowest.Furthermore, technical difficulty or skill were not considered particularly strong contributing factors in determining ranking.
In addition to reflecting the level of confidence in certain areas of the examination, the variability in rankings may indicate suboptimal elements and present opportunity for innovation.For example, several recent developments have been made to more easily evaluate ocular motility and visual acuity, both components of which were ranked low by our cohort.These include contemporary commercial software aiming at automatic strabismus assessment using eye tracking, near vision assessment using smartphones,and application of artificial intelligence in the diagnosis of anterior and posterior segment diseases[8-11].The introduction of these innovations may alter a resident’s perception of these exam aspects for the better, consequently enhancing the desire to pursue a fellowship in related subspecialties,such as pediatric ophthalmology and strabismus or neuroophthalmology.Additional developments under evaluation are gonio-photographic systems, which allow for qualitative assessment, similar to gonioscopy.More recently developed systems include learning algorithms that help classify angle findings, which could greatly aid residents in diagnosis[12-13].Gonioscopy ranked as the least popular component in our study, potentially due to its relative complexity and the high level of skill required for appropriate examination.Innovations in the field could therefore serve to increase the attractiveness of the ophthalmic exam components[12].
Choosing a Medical CareerChoosing a medical specialty and subspecialty is one of the most important decisions made by physicians throughout their professional career.Several motivating factors have been described in the pursuit of residency in ophthalmology[14-15].These include the ability to combine the practice of medicine and surgery, perceived intellectual stimulation, mentorship, teaching and research opportunities, and flexibility[16].Time spent with patients,physician teamwork, autonomy, and responsibility were also perceived advantages[17].In 1989, a controllable lifestyle was reported as a “new factor in career choice by medical students”, and lifestyle considerations, such as working hours and location, were found to be significant factors[18-19], as were degree of diagnostic uncertainty and peer interactions[20-21].
Subspecialty training is considered by some as the pinnacle of medical training[22].During this time, individuals move from a general training process to the start of their specialist careers.Factors influencing the decision whether to pursue a subspecialty and the choice of subspecialty include research and academic opportunities and delectation from subspecialty’s surgical procedures and/or clinic visits[2,23-24].In addition to pure professional interest and personal inclination, a subspecialty’s prestige, earning potential and job opportunities contribute to these decisions[25-26].Faculty role models and mentorship,adequate teaching and surgical exposure were found to be additional considerations[26-28].In cases where residents displayed lower levels of surgical competence, they were often advised to continue practicing as medical ophthalmologists, or to seek additional training in fellowship programs[29].
Anterior segment and retina subspecialties are commonly reported among the most popular, as supported by our current findings[1,16,30-31].This tendency may be attributed to the high ranking given to the anterior and posterior segment slit-lamp examinations, in addition to the multiple variables cited above.In further support, anterior segment slit-lamp examination was the only significant factor associated with choosing anterior segment fellowship as a sole future career choice.Interestingly,those considering a career in pediatric ophthalmology gave a significantly lower ranking to anterior slit-lamp examination,in agreement with the slight overlap between responders who were considering an anterior segment fellowship and those considering a pediatric-strabismus fellowship.The scarcity of residents mutually interested in both fields may also be attributed to differences in “time consumption”, ranked as being of high importance in our study: specifically, while an anterior segment examination tends to be relatively rapid,a pediatric examination can be time consuming.Residents interested in retina fellowships tended to favor ophthalmic exam aspects pertaining to visualization of the posterior segment (by either slit-lamp or indirect ophthalmoscopy)while also deterring from aspects related to neuro-ophthalmic evaluations.Although supportive literature is lacking, it is possible that the differing focus of the examinations contribute to this relationship, with a retinal examination being mainly intraocular with focus on structure and a neurological examination being mostly extraocular with focus upon function.A fellowship in pediatric ophthalmology and strabismus was sought after by 14 (18%) of the residents in our cohort, possibly attributed to the lower ranking given to ocular motility testing.Additionally, difficulties in handling children and stress were found to contribute to dissuading physicians from pursuing a career in pediatric ophthalmology[2].This finding further supports the influence the physician’s feeling during the ophthalmic exam has on attraction versus aversion toward the relevant subspecialty[2,32].A glaucoma fellowship was sought after by 10 (12.5%) residents, corresponding to the lowest likeability ranking given to gonioscopy.Residents interested in oculoplastics assigned a significantly lower ranking to posterior segment evaluations, coinciding with the paucity of residents interested in both oculoplastics and retina fellowships.Among the ophthalmology subspecialties,the techniques implemented in the operating room by oculoplasticians are closest to those used in classic surgery,thus the high ranking given to “scraping” by residents interested in oculoplastics might be related to their desire to perform surgery.
This study has several limitations, mainly the inherent drawbacks of questionnaire studies originating from variabilities in individuals’ interpretation of the questions.The survey may have been subject to recall bias since it relied upon self-reported data.Another limitation is the small sample size.Only one-half of the residents participated in this nationwide study, and different trends might have been observed among larger sample sizes.Furthermore, since this survey pertains to residents training in a number of institutions, they may have had varying levels of access to supplementary tests, such as optical coherence tomography and corneal topography,potentially influencing their perceptions.
Although our study suggests that residents’ perceptions of various aspects of the ophthalmic exam might affect their inclinations towards certain subspecialties, a reciprocal relationship might also coexist.The inclination toward certain subspecialties results in the resident’s attaining more experience in a certain part of the comprehensive exam,thereby creating a positive feedback loop of improvement of those skills and favoring of that particular aspect of the exam.Residents’ perceptions of various components of the ophthalmic exam correlated with their future practice choices.As the performance of many of the exam’s components will be performed in the future by technicians or automated devices, further technological advancement may make the ophthalmological examination more pleasant for both the patient and the physician.These advancements could alleviate many of the intrinsic difficulties and influence the rate and reliability of these examinations as performed by residents as well as senior physicians.Beyond greatly improving patient care, further investigation may reveal whether these innovations alter resident perceptions, and in turn, lead to a positive change in the current trends in subspecialty preferences among future physicians.
ACKNOWLEDGEMENTS
Conflicts of Interest: Leshno A,None;Shalev D,None;Landau Prat D,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Using choroidal thickness to detect myopic macular degeneration
- lmpact of multifocal gas-permeable lens designs on short-term choroidal response, axial length, and retinal defocus profile
- Baerveldt glaucoma implant with Supramid© ripcord stent in neovascular glaucoma: a case series
- Efficacy and safety of Usights UC100 illuminated microcatheter in microcatheter-assisted trabeculotomy
- Quantifying peripapillary vessel density and retinal nerve fibre layer in type 1 diabetic children without clinically detectable retinopathy using OCTA
- Nomogram to predict severe retinopathy of prematurity in Southeast China
