One-year results for myopia control of orthokeratology with different back optic zone diameters: a randomized trial using a novel multispectral-based topographer
2024-02-23WenTingTangXiangNingLuoWenJingZhaoJiaLiaoXinYueXuHuiDanZhangLiZhang
Wen-Ting Tang, Xiang-Ning Luo, Wen-Jing Zhao, Jia Liao, Xin-Yue Xu, Hui-Dan Zhang,Li Zhang
Department of Ophthalmology, the First Affiliated Hospital of Chengdu Medical College, Chengdu Medical College,Chengdu 610500, Sichuan Province, China
Abstract
● KEYWORDS: relative peripheral refraction; orthokeratology;myopia; back optic zone diameter; axial length; multispectral refractive topography
INTRODUCTION
The increasing prevalence and pathological complications of myopia have raised public concerns about control strategies.Orthokeratology (ortho-k) has been considered one of the most effective methods for myopia control in children.Previous studies confirmed that wearing ortho-k slowed down axial elongation by 40%-60%, compared with spectacles[1-2].But the mechanism remains unclear, and how to improve the efficacy of ortho-k attracts growing attention from practitioners and patients.
Overnight ortho-k produces reversible central cornea flattening(treatment zone) and surrounded mid-peripheral steepening(defocus ring), then may change the peripheral refraction towards myopic defocus which means that the off-axis focus falls anterior to the retina and thereby acts as a retardation signal for axial growth[3-4].Some scholars speculate that the area and degree of myopic defocus obtained on peripheral retina may be related to the myopia control effect[5-6].A series of retrospective studies have observed that children with smaller treatment zone tend to experience slower axial elongation from ortho-k[7-8].A few short-term (1-2wk) studies in adults have proposed that ortho-k with a smaller back optic zone diameter (5 mm BOZD) was developed to achieve a smaller treatment zone and inferred it could induce more peripheral myopic defocustocontrolmyopia progression[9-10].Concerning the potential impact on visual quality impairment[11], some practitioners suggest a 5.5 mm BOZD as a balance point in clinical practice.However, the previous studies only used a 5 mm BOZD ortho-k lens design and did not explore if it could consequently obtain a wider, deeper myopic defocus to achieve more effective myopia control.
On the other hand, it is imperative to measure relative peripheral refraction (RPR) to elucidate the mechanism of ortho-k lenses.The most commonly used method in scientific research is WAM-5500 (Grand Seiko, Hiroshima,Japan) or NVision-K 5001 (ShinNippon, Tokyo, Japan)autorefractor[12-13].However, its large-scale clinical application is restricted because of time-consuming, complex operations and a few specific spots only[14].Multispectral refractive topography (MRT) is a new approach based on multispectral imaging (MSI) technology[15-16]and in-depth computer algorithms.It can detect the topographic map and spherical equivalent (SE) of peripheral retina from 0° to 53° within 2-3s.A series of studies have confirmed its repeatability and accuracy[17-21].
Therefore, we originally designed a 2-year prospective,randomized study to evaluate the efficacy and safety of ortho-k with reduced BOZD (5 and 5.5 mm) compared with conventional BOZD (6 mm) in adolescent myopia control and explore its possible mechanism by MRT.In this report, the study design and lens performance are presented during the 1-year visit.
SUBJECTS AND METHODS
Ethical ApprovalThis double-blinded, randomized controlled trial adhered to the guidelines of the Helsinki Declaration and obtained approval from the Institutional Review Board of the First Affiliated Hospital of Chengdu Medical College(2020CYFYHEC-BA-32).All participants and their guardians signed a written consent after being fully informed of the study protocol, potential benefits, and complications.
SubjectsBetween Dec 2020 and Dec 2021, this study enrolled 88 participants in the First Affiliated Hospital of Chengdu Medical College.The inclusion criteria were: 8 to 14 years old, spherical power between -5.00 and -1.00 D, anisometropia no more than 1.00 D, best corrected visual acuity (BCVA,logMAR) no worse than 0.00, astigmatism less than 1.50 D,and normal pupil size (2.5-4 mm).The exclusion criteria were:an experience of myopia control, ocular or systemic disease,contraindications for ortho-k lens, poor compliance, and disagreement with randomization.
Allocations and TreatmentsAll the enrolled participants were trained in lens handling and care procedures.Then 72 participants who had successfully completed the training course were assigned into three groups at random:experimental group 1 (wore 5 mm BOZD ortho-k lenses,5-MM group), experimental group 2 (wore 5.5 mm BOZD ortho-k lenses, 5.5-MM group), and control group (wore 6 mm BOZD ortho-k lenses, 6-MM group).The random numbers were generated by Microsoft Excel and concealed in opaque envelopes by an external researcher.Patients and the examiner were blind to the group assignment.All subjects were fitted with the spherical and VST design Mouldway ortho-k (Autek China Inc.) and followed the manufacturer’s guidelines.
MeasurementsAll participants should attend 1d, 7d,1mo, 3mo, 6mo, 12mo, and any necessary unscheduled consultations.The aftercare visits were fulfilled within 2h after lens removal (between 8:00a.m.and 10:00a.m.).
Relative Peripheral RefractionMRT (MSI C2000, Thondar,China) was used to measure RPR after complete cycloplegia.The measuring method has been reported in prior research[17-20].RPR=SEa-SE0(a represents the peripheral retinal region,0 represents the central fovea).Total RPR (TRPR, the 53°circular retinal area centered on macular central fovea), RPR in the 15° (RPR 15), 15°-30° (RPR 15-30), and 30°-45°(RPR 30-45) areas were recorded.RPR was also divided into four quadrants: superior (RPR-S), inferior (RPR-I), temporal(RPR-T), and nasal (RPR-N) quadrant.According to the RPR data of each point on the retina, a direct color-coded image was obtained (Figure 1).
Contrast SensitivityContrast sensitivity (CS) which was used to evaluate the objective visual quality was assessed by CSV-1000E (VectorVision, USA) under photopic (85 cd/m2)condition at a 2.5 m distance.The logarithmic values for 3, 6,12, and 18 cycles/degree (c/d) were analyzed (https://www.vectorvision.com/csv1000-contrast-sensitivity/).
Higher-Order AberrationsCorneal higher-order aberration(HOAs) were measured by iTrace aberration analyzer (Tracey,USA) through the natural pupil in a dark room.The pupil diameter for analysis was 6 mm.The corneal HOAs were calculated by Zernike polynomial as the root mean square(RMS).
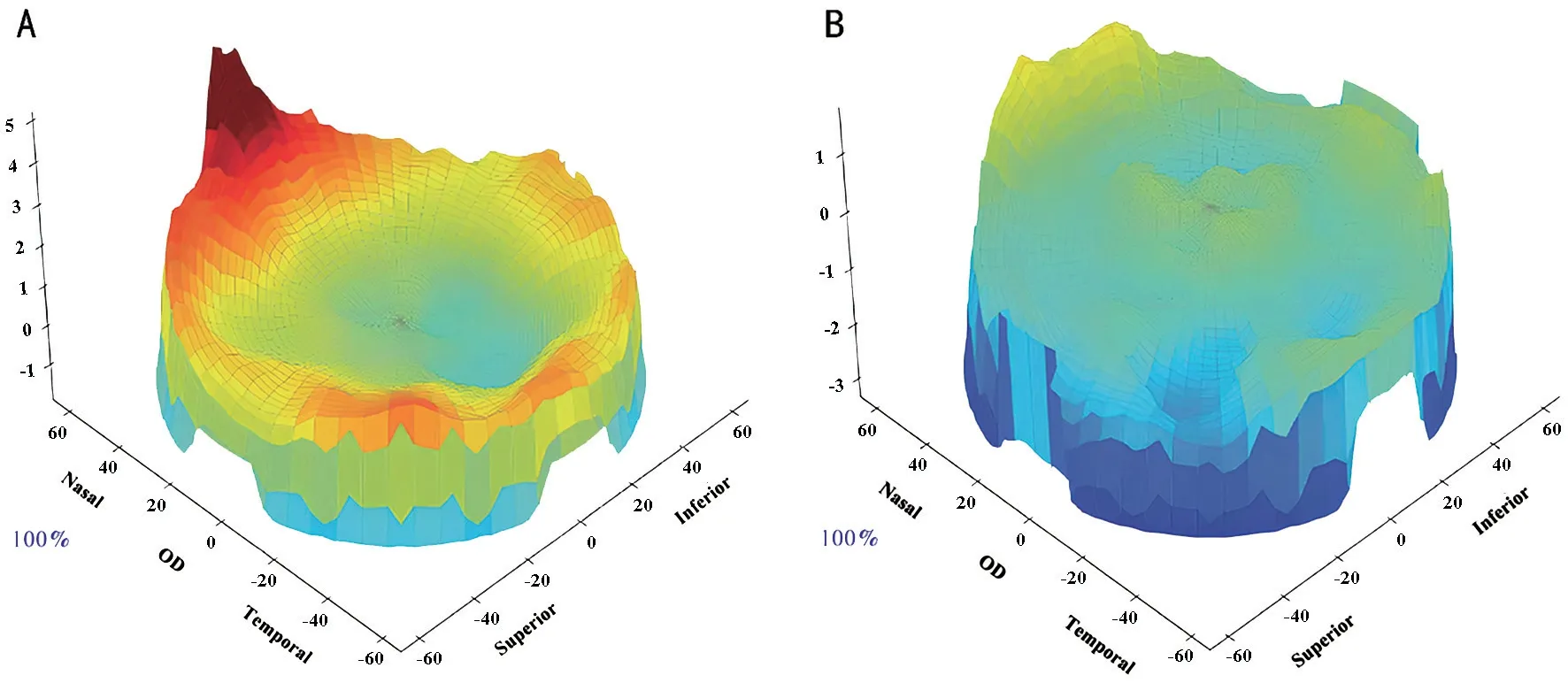
Figure 1 A typical three-dimensional MRT outcome at baseline (A) and 1-year visit (B) The hyperopic RPR is presented by a warm color(yellow-red), while the myopic RPR is presented by a cold color (blue-green).
Average keratometry (Kv), axial length (AL), SE, and BCVA were measured by SW-6000 corneal topography (Suoer, China),IOLMaster 500 (Carl Zeiss, Germany), RM8900 (Topcon,Japan), and ETDRS charts 2000 (Precision Vision, USA),respectively, following the manufacturer’s guidelines.The subjective visual performance was assessed by the National Eye Institute/Refractive Error Quality of Life Instrument-42 questionnaire (NEI-RQL-42)[22].A SL-1E slit lamp (Topcon,Japan) was used to examine the corneal staining that was graded by the Efron grading scales[23].
Sample SizeAccording to the generally accepted study[24], and based on the one-way ANOVA for three means (PASS 11.0), it would be detected as a statistical difference of 0.17 mm (AL)and 0.25 mm in standard deviation between the three groups in 2y.To achieve 10% inβerror and 0.05 inαerror, each group should contain a sample size of 15 participants.Assuming a dropout rate of 30% after allocation into three groups, a total of 66 participants were required to meet the minimum sample size.
Statistical AnalysisThe data from the right eyes were used for analysis.SPSS version 22.0 statistical software(IMB-SPSS Inc., USA) was conducted for data analysis.The correlation between the change in AL and RPR was calculated by Pearson’s correlation coefficient.Categorical data were analyzed by Chi-squared test (or Fisher exact test,as appropriate).Shapiro-Wilk test was applied to evaluate the normality of the data, and data with normal distribution were represented as mean±standard deviation.Levene’s test was used for evaluating the variance homogeneity of the data.Then one-way ANOVA was performed to assess the differences between the three groups.The difference was considered statistically significant when aPvalue was less than 0.05.Posthoc analysis [Least significant difference (LSD) or Tamhane test, as appropriate] was carried out, and the difference was considered to be statistically significant when aPvalue was less than 0.017 (0.05/3).

Figure 2 Study flowchart 5-MM, 5.5-MM, 6-MM: Wearing orthokeratology with back optic zone diameters of 5, 5.5, and 6 mm,respectively.
RESULTS
Subjects and Baseline BiometricsA total of 62 participants(20 in the 5-MM group, 21 in the 5.5-MM group, and 21 in the 6-MM group) finished the 1y follow-ups (Figure 2).There were no statistical differences in demographics or baseline data between the three groups (allP>0.05; Table 1).
Changes in Axial LengthThe AL elongation was statistically different between the three groups at 6mo and 12mo followups (allP<0.05).The AL elongation in the 5-MM group was slower than that in the 6-MM group by post-hoc analysis (6mo:P=0.01, 12mo:P=0.001); the 5-MM group was 61.11% slower in AL elongation than 6-MM group at the 12mo visit.But there were no statistical differences in the other two comparisons (5-MM groupvs5.5-MM group, 5.5-MM groupvs6-MM group,P>0.017; Table 2).

Figure 3 RPR at the 12-month visit 5-MM, 5.5-MM, 6-MM: Wearing ortho-k with back optic zone diameters of 5, 5.5, and 6 mm, respectively.Post-hoc test, aP<0.017, bP<0.01, cP<0.001.Error bars represent standard deviation.AL: Axial length; RPR: Relative peripheral refraction;Ortho-k: Orthokeratology; TRPR: Total relative peripheral refraction; S: Superior; I: Inferior; T: Temporal; N: Nasal.

Table 1 Baseline data mean±SD

Table 2 Axial length elongation mean±SD, mm
RPR in Different Retinal RegionsThere were statistical differences in TRPR (F=3.207,P=0.048), RPR 15-30(F=5.631,P=0.006), RPR 30-45 (F=4.795,P=0.012), RPR-T(F=4.233,P=0.019), and RPR-N (F=22.732,P<0.001)between three groups at the 12-month visit.Post-hoc analysis revealed that TRPR, RPR 15-30, RPR 30-45, RPR-T, and RPR-N in the 5-MM group were more myopic than those in the 6-MM group (P=0.014,P=0.015,P=0.011,P=0.008,P<0.001, respectively).RPR 15-30 in the 5.5-MM group was more myopic than that in the 6-MM group (P=0.002),and RPR-N in the 5-MM group was more myopic than that in the 5.5-MM group (P<0.001).However, RPR 15, RPR-S,and RPR-I between the three groups did not present statistical differences (allP>0.05; Figure 3).
Relationship Between the Change in AL and RPRThe Pearson correlation analysis indicated that the change in AL over 1y was not statistically correlated with the change in RPR 15, RPR-S, RPR-I, and RPR-T (allP>0.05).The change in AL was positively associated with the change in TRPR, RPR 15-30, RPR 30-45, and RPR-N (allP<0.05; Figure 4).

Figure 4 Scatterplot exhibits the correlation between the change in AL and RPR over 1y AL: Axial length; RPR: Relative peripheral refraction; TRPR: Total relative peripheral refraction; N: Nasal.
Visual Quality and Other ComplicationsThere were no serious adverse events (e.g., infiltrates, pannus, microbial keratitis,microcysts) occurred in the study period.The CS decreased at 3 c/d, and the corneal HOAs increased in the 5-MM group over 1y (allP<0.05).Other parameters did not show statistical differences between the three groups (allP>0.05; Table 3).

Table 3 Comparisons of visual quality and other complications over 1y
DISCUSSION
These first-year outcomes of the longitudinal trial demonstrated that ortho-k with 5 mm BOZD was more effective in slowing axial elongation, which might be related to greater myopic shifts in RPR.
In our study, the annual AL elongation was significantly less wearing 5 mm BOZD ortho-k than 6 mm BOZD ortho-k,with a mean reduction of 0.11 mm.This indicated 61.11%less AL growth wearing 5 mm BOZD ortho-k and was close to previous studies (0.08-0.17 mm/y AL decrease in absolute value and a control effect of 50%-76.47%)[25-28].We found that the annual AL growth in the 5-MM group was 0.07 mm, which was close to the physiological AL growth of emmetropic children in the Singapore Cohort Study of the Risk Factors for Myopia (SCORM study)[29].The annual AL growth in our study for the conventional BOZD (6 mm) group was 0.18 mm,which agreed with Guoet al[25], Paunéet al[26], and the overall consensus[30-31].However, the AL growth values investigated by Liet al[27]and Zhanget al[28]were greater than ours.One possible reason is that children in their study were younger and had lower SE values than our study.The different ortho-k types(5 mm BOZD: Double Reservoir, 6.2 mm BOZD: Euclid)used in their study may also partly explain the discrepancy.Furthermore, their study might have been affected by the COVID-19 lockdown, which could speed up AL elongation in young children[32].In our study, the annual AL elongation was 0.05 mm less wearing 5 mm BOZD ortho-k than 6 mm BOZD ortho-k.However, the results did not show a statistically significant difference.This implied that the 5.5 mm BOZD ortho-k lens might not steepen enough mid-peripheral cornea or increase enough HOAs to change the peripheral myopic defocus imposed on retina.Further large-scale investigations are needed to assess its long-term validity for myopia control.Regarding the 1-year change in RPR of smaller BOZD ortho-k,the available data is limited.Our results manifested that TRPR,RPR in the retinal region of 15°-45°, and RPR in the temporal and nasal areas were more myopic wearing 5 mm BOZD ortho-k than 6 mm BOZD ortho-k.This was close to the results drawn by Pegudaet al[33].The latter study manipulated scleral contact lenses to mimic the two ortho-k lens designs and found a myopic shift of RPR in the nasal horizontal meridian.However, Giffordet al[10]proposed a differing viewpoint, stating that there was no statistical difference in the change of RPR between the two lens designs.The cause might be that subjects in Giffordet al’s[34]study were adults, the sample size was too small (n=16), or the observation period was only 7d while RPR was stable between 6 and 18mo of ortho-k lens wear according to the previous studies[35].Pegudaet al[33]and Giffordet al[34]used Shin-Nippon NVision-K 5001 autorefractor to measure the RPR of some specific spots (0°,10°, 20°, 30°, 35°) in the horizontal or vertical meridian.This instrument relies on the alignment and patient’s cooperation a lot; the misalignment of the instrument may lead to considerable errors in RPR measurement (1 mm misalignment may cause 1.3-2.7 D errors at 30° field)[36].While the advent of MRT has enabled the effective and comprehensive measurement of peripheral refraction in different areas.
This study found a positive correlation between one-year AL elongation and TRPR (strong correlation), RPR 15°-45°(moderate correlation), and RPR-N (weak correlation), which was not observed in the previous study.Liet al[21]conducted a cross-sectional study that used MRT to measure the RPR of conventional BOZD (6 mm) ortho-k, and their results were approximately in accordance with ours.However, they did not measure the RPR before wearing ortho-k to evaluate the change in RPR, and their subjects wore ortho-k for 9mo.These findings indicate that different regions of the peripheral retina may play significant or minor roles in AL growth and myopia progression.Myopic defocus in 15°-45° suggests less AL growth, while RPR 15° seems irrelevant.The possible reason is that lights passing through the mid-peripheral cornea and causing myopic defocus mainly locate in the 15°-45° area of the retina.We infer that myopic defocus induced by ortho-k in this area may have a significant impact on the progression of myopia.However, the 15° area may mainly relate to the central correction region and just locate on the macular, so it did not show a significant impact on the axial elongation.We also discovered that, in contrast to the vertical field, the peripheral refraction of the horizontal field was more affected by ortho-k.
This conforms to the previous studies about the conventional BOZD (6 mm) ortho-k[6,34].In addition, RPR-N rather than RPR-T had a greater impact on AL growth, which suggested that light signals from the temporal side (wider than the vertical and nasal sides) may be associated with ocular growth.In the ortho-k mechanism, there may be an intricate regulatory between the RPR and the myopia control efficacy, which needs further investigation.
It should be noted that the CS decreased at the low spatial frequency (3 c/d), and the corneal HOAs showed a significant increase, indicating a decline in visual quality in the 5-MM group.However, there were no significant differences in subjective visual performance between the three groups.It is hypothesized that a blur adaptation or visual compensation may occur in children with smaller BOZD ortho-k.However, it is important to consider the potential benefits and risks of both visual quality and myopia control.
There were two main limitations in this study.First, the subjects have not stopped wearing ortho-k lenses for 4wk or more, so we cannot obtain accurate changes in SE, but we will provide the complete results after the end of our trial.Second, the current study was unable to define the cause-effect sequence between peripheral defocus and myopia control.Further research is needed to determine the mechanism by which peripheral defocus impacts AL growth.In conclusion, the current study assessed the three different ortho-k lens designs and used a unique MRT to analyze the change in RPR.Ortho-k with a 5 mm BOZD showed further substantial retardation of axial elongation compared with conventional ortho-k, and the possible mechanism is greater myopic shifts in RPR.This study may provide an optimized ortho-k lens design for myopia control.
ACKNOWLEDGEMENTS
Foundation:Supported by Education Department Foundation of Sichuan Province (No.15ZA0262).
Conflicts of Interest: Tang WT,None;Luo XN,None;Zhao WJ,None;Liao J,None;Xu XY,None;Zhang HD,None;Zhang L,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Using choroidal thickness to detect myopic macular degeneration
- lmpact of multifocal gas-permeable lens designs on short-term choroidal response, axial length, and retinal defocus profile
- Baerveldt glaucoma implant with Supramid© ripcord stent in neovascular glaucoma: a case series
- Efficacy and safety of Usights UC100 illuminated microcatheter in microcatheter-assisted trabeculotomy
- Quantifying peripapillary vessel density and retinal nerve fibre layer in type 1 diabetic children without clinically detectable retinopathy using OCTA
- Nomogram to predict severe retinopathy of prematurity in Southeast China
