Intravitreal injection of conbercept for diabetic macular edema complicated with diabetic nephropathy
2024-02-23YuanZhangZhuZhiZhiDouWenYingWangQingYueMaWenDanYiNingNingYaoYiChongLiuXiaoDiGaoQianZhangWenJuanLuo
Yuan-Zhang Zhu, Zhi-Zhi Dou, Wen-Ying Wang, Qing-Yue Ma, Wen-Dan Yi, Ning-Ning Yao,Yi-Chong Liu, Xiao-Di Gao, Qian Zhang, Wen-Juan Luo
Department of Ophthalmology, the Affiliated Hospital of Qingdao University, Qingdao 266000, Shandong Province, China
Abstract
● KEYWORDS: conbercept; diabetic nephropathy; diabetic macular edema; optical coherence tomography
INTRODUCTION
Diabetic retinopathy (DR) attracts attention because of vision threaten, and it was originally considered as a typical retinal microvascular disease, however, with research goes deeper DR was found to be the result of co-participation of multiple cell types (endothelial cells, microglia, astrocytes,and Müller neurons).Therefore, DR is not only a retinal microvascular disease, but also a chronic inflammation and a retinal nerve disease, which means DR could be affected by systemic metabolic and cardiovascular factors[1].
Diabetic macular edema (DME) can occur at any stage of DR, seriously threatening the vision of DR patients.The main treatment methods of DME include anti-vascular endothelial growth factor (VEGF) drugs, glucocorticoids and retinal laser photocoagulation[2].Due to the destructive nature of retinal laser photocoagulation and side effects of glucocorticoid, they are generally not the first choices for the treatment of DME.At present, anti-VEGF drugs are used as the first choice for DME because of rapid effect and high safety.
Conbercept is an anti-VEGF drug widely used in China.It is a fusion protein for VEGF receptor and Fc segment of human immunoglobulin.It can bind to VEGF-A, VEGF-B,and placental growth factor (PIGF), reduce the formation of neovascularization with a long half-life.At present, conbercept is widely used in clinical treatment, including retinal vein occlusion, secondary macular edema caused by DR, and choroidal neovascularization caused by pathological myopia.
In clinical application of conbercept to DME patients, we found that some patients appeared refractory DME, recurrent DME, best corrected visual acuity (BCVA) did not improve or even decreased, and most of these patients have chronic kidney disease or cardiovascular disease.Thus, we were wondering that the efficacy of anti-VEGF treatment in DME was closely related to the systemic condition of patients.However, there are few studies about the prognostic impact of conbercept on DME patients combined with chronic kidney disease.
In this retrospective study, we compared the treatment effect of conbercept between DME patients combined with and without diabetic nephropathy (DN), analyzed general situation,central macular thickness (CMT), BCVA, the number of hyperreflective foci (HF) and other characters, to explain the pathological mechanism.
SUBJECTS AND METHODS
Ethical ApprovalThis study was performed according to the Declaration of Helsinki.All patients signed informed consent before treatment.This study was submitted to the Ethics Committee of the Affiliated Hospital of Qingdao University for review, and the approval number was QYFYWZLL26980.
PatientsWe selected 54 DME patients visited the ophthalmology department of our hospital from January 2017 to October 2021, including 25 patients with DN and 29 patients without DN.
The inclusion criteria were: 1) more than 18 years old; 2) type 1 or type 2 diabetes; 3) non-proliferative DR; 4) clinically significant macular edema; 5) with or without DN.The exclusion criteria were: 1) combined with uveitis, retinal vascular obstruction, macular hole and other retinal diseases by fundus examination after mydriasis; 2) previous internal eye surgery; 3)previous retinal laser photocoagulation; 4) the refractive medium is unclear; 5) systolic blood pressure >160 mm Hg or diastolic blood pressure >100 mm Hg; 6) serious cardiovascular and cerebrovascular diseases.
Intraocular InjectionsIntravitreal injection of conbercept was applied in both groups.Levofloxacin eye drops used at the eye 3d before surgery, 4 times per day.Intravitreal drug injection procedure: the patient was required with supine position, then local anesthesia, aier iodine cleaned the conjunctival sac, and disinfected the eye.Vitreous injection was performed 3.5 mm posterior to the corneal limbal(perpendicular to the ocular surface), the vitreous cavity was injected with 0.5 mg conbercept.Levofloxacin eye drops was applied to postoperative eyes for 5d, 4 times per day.
Outcome MeasuresSlit lamp was used for routinely examination.Fundus examination was performed by the fundus photometer of Heidelberg Company.Biochemical indicators were collected by blood test and urine test that based on the results of 1d before injection.
BCVA Check UpComputer optometry and apparently optometry performed for BCVA.Using ETDRS visual acuity chart, at the 4 m distance, the patient recognized ETDRS letter,and if all letters could be identified, the corresponding visual acuity was 100 ETDRS letters.If the patient could not identify 4 letters at 4 m, the BCVA examination distance was changed to 1 m.Optometry operations are performed by a professional optometrist.The BCVA converts to the logarithm minimum angle of resolution (logMAR).
CMT MeasurementThe examination was performed using Heidelberg Spectralis SD-OCT.The inspection parameters of OCT were set as follows.The inspection adopted the horizontal mode, and the scanning area was 6 mm×6 mm; the transverse and longitudinal inspection resolutions were set as 14 μm and 7 μm, the inspection depth was 1.9 mm, and the inspection center was the macular fovea.The length of the hyperreflective band of the retinal pigment epithelium (RPE) in the fovea of the macula to the inner boundary membrane was considered as CMT value.
Statistical AnalysisThe database was established by Excel software, which used for data collation.Statistical analysis was performed by SPSS26.0 (USA).Quantitative data were presented as mean±standard deviation (mean±SD), BCVA was converted to logMAR.Normal distribution was checked by Shapiro-Wilk test, if normal distribution was met, ANOVA was used, otherwise Kruskal-Wallis rank sum test was used.Comparison of two groups at multiple time points was performed by ANOVA with repeated measures data and further group pairwise comparisons by LSDt-test.Qualitative data were presented as rate, andχ2test was used for comparison between groups.Test levelα=0.05,P<0.05 were statistical significance.
RESULTS
General Conditions and Laboratory Tests Between the Two GroupsAmong the 54 patients (54 eyes) of DME included in this study, 28 were male and 26 were female.Patients were divided into 2 groups based on whether combined with DN:DME combined with DN in 25 cases (DME+DN group), 29 cases with DME alone (DME group).No difference between sex, height and weight in the two groups (P>0.05), the differences were statistically significant in age and duration of diabetes (P<0.05).Laboratory test indicators in two groups:fasting blood glucose, glycated hemoglobin, serum creatinine,(eGFR), and urinary microalbumin/creatinine were compared,all these differences were statistically significant (P<0.05;Table 1).
Eye Parameters of Two Groups Before TreatmentAll the differences of eye parameters were statistically significant in two groups before treatment, including BCVA (logMAR),CMT, external limiting membrane (ELM) continuity, ellipsoidal zone (EZ) continuity, and HF number (allP<0.05; Table 2).

Table 1 General conditions and laboratory tests between the two groups
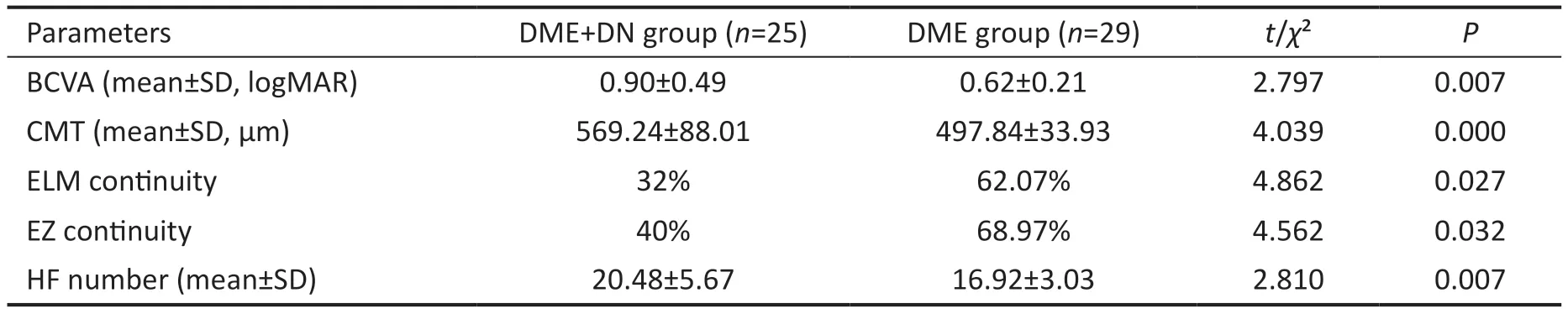
Table 2 Comparison of each index before treatment in the two groups
Changes of BCVA Before and After Treatment in Both GroupsBCVA (logMAR) before and after treatment improved significantly over time in both groups, the difference was statistically significant (Ftime=20.815,P<0.001), there were significant differences in the comparisons between the two groups (Fgroup=12.994,P<0.001) and no interaction effect between time and group (Ftime×group=2.898,P=0.058).Both groups showed a significant decrease of BCVA (logMAR; allP<0.05) at 3 time points after treatment than that in baseline.In the DME+DN group, BCVA (logMAR) decreased in the first and third month, but rebounded at the sixth month, the difference was not statistically significant (allP>0.05).While in the DME group, BCVA (logMAR) decreased statistically significant at first, third and sixth month after treatment(allP<0.05).BCVA (logMAR) of the DME group was significantly better than that of the DME+DN group at the same treatment time points (allP<0.05; Table 3, Figure 1).
Changes of CMT Before and After Treatment in Both GroupsCMT of the two groups decreased significantly over time, the difference was statistically significant (Ftime=215.042,P<0.001); there was significant CMT difference between the two groups (Fgroup=22.181,P<0.001), and there was no interaction effect between time and group (Ftime×group=2.537,P=0.083).CMT in both groups decreased significantly at 3 time points after treatment compare with before treatment (allP<0.05).CMT in the DME+DN group decreased significantly at 1mo and 3mo after treatment (bothP<0.05), but there wasno statistically significant difference between 6mo and 3mo(P>0.05).In DME group, CMT decreased significantly at 1,3, and 6mo after treatment (allP<0.05).CMT in the treatment group was significantly higher than that of the DME group at the same time points (Table 4, Figure 2).

Table 3 Changes of BCVA (logMAR) before and after treatment in both groups mean±SD, logMAR
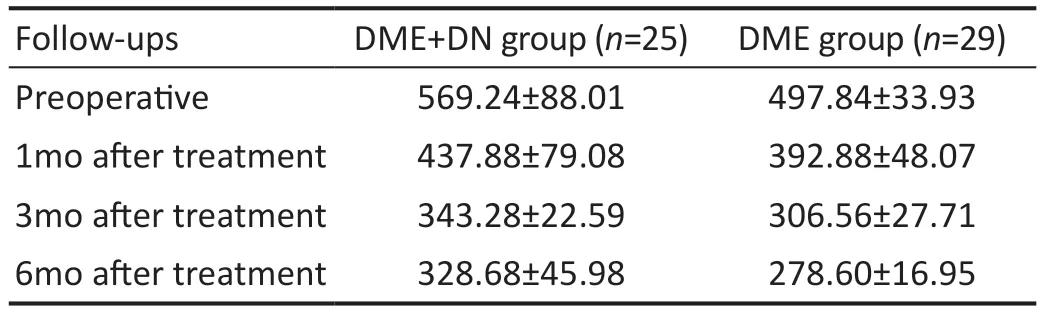
Table 4 Changes of CMT before and after treatment in both groups mean±SD, µm

Figure 1 Changes of BCVA (LogMAR) before and after treatment in both groups BCVA: Best corrected visual acuity; DME: Diabetic macular edema; DN: Diabetic nephropathy.

Figure 2 Changes of CMT before and after treatment in both groups CMT: Central macular thickness; DME: Diabetic macular edema; DN:Diabetic nephropathy.

Figure 3 Changes of HF amount before and after treatment in two groups HF: Hyperreflective foci; DME: Diabetic macular edema; DN:Diabetic nephropathy.
Changes of HF Amount Before and After Treatment in Two GroupsThe amount of HF in the two groups decreased significantly over time after treatment (Ftime=151.612,P<0.001); there was a significant difference in the comparisons between the two groups (Fgroup=11.696,P<0.001), and there was no interaction effect between time and group(Ftime×group=1.706,P=0.195).The amount of HF in both decreased significantly at 1, 3, and 6mo after treatment, and the difference in the two groups was statistically significant(allP<0.05).The amount of HF in the DME+DN group was significantly higher than that in the DME group at all time points (P<0.05; Table 5, Figure 3).OCT images of a patient in DME+DN group at different time were showed in Figure 4, HF existed between the outer plexiform layer and the outer nuclear layer before treatment (Figure 4A).With the extension of treatment time, CMT continuously decreased and HF gradually disappeared at 1, 3, and 6mo after treatment(Figure 4B-4D).

Figure 4 OCT images of a patient in DME+DN group at different time A: Before treatment, white arrow showed HF position.B, C, and D:1, 3, and 6mo after treatment, respectively.OCT: Optical coherence tomography, HF: Hyperreflective foci; DME: Diabetic macular edema;DN: Diabetic nephropathy.
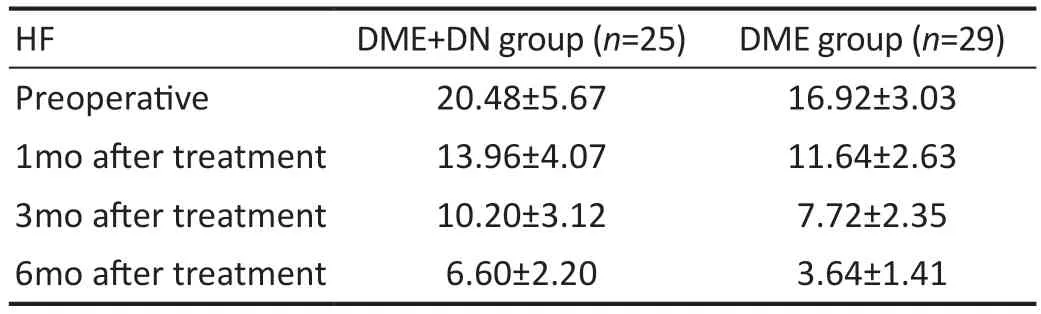
Table 5 Changes of HF amount before and after treatment in both groups mean±SD
Number of Injections Between the Two GroupsThe mean number of injections during the 6mo treatment in the DME+DN and DME group was 4.84±0.94 and 3.79±0.86,respectively, the difference between the two groups was statistically significant (t=4.262,P<0.001).
DISCUSSION
In this study, we found that conbercept has a significant effect in the short-term treatment of DME patients with DN and DME alone, and can significantly benefit BCVA, CMT and the number of HF.With the extension of treatment time, the therapeutic efficacy of conbercept in DME patients with DN was lower than that in DME alone, in which progression retinal dysfunction play an important role.Current views on the development of DME mainly focus on the breakdown of the retinal barrier mediated by VEGF and other inflammatory cytokines[3]and the obstruction of retinal interlayer fluid clearance[4].VEGF and PIGF factors play an important role in the occurrence and development of DME.The concentration of VEGF in vitreous was significantly higher in DME patients than that in diabetic patients without retinopathy[5].VEGF is produced by microvascular endothelial cells, pericytes and RPE cells during retinal hypoxia.In the VEGF factor family, VEGF-A and VEGF-B are mainly factors involved in DME.VEGF-A increases the number of endothelial cells and stromal cells through VEGF-2 receptor mediated cell signal transduction, thereby changing blood vessel morphology, damaging the inner retinal barrier and inducing neovascularization[6].VEGF-B can stabilize neovascularization by acting on vascular endothelial cells and pericytes[7].At present, anti-VEGF drugs are the first-line drugs in the treatment of DME.Conbercept is an anti-VEGF drug designed and widely applied in China.It is a recombinant fusion protein, which can specifically bind VEGF-A, VEGF-B and PIGF[8], block VEGF-mediated signal transduction, reduce microvascular leakage and endothelial cell proliferation, and alleviate macular edema.
Beyond the influence of the course and severity of diabetes on DME, the systemic influence caused by DN and its promoting effect on DME should also be considered.Previous studies reported that albuminuria, eGFR and DN grade were correlated with DME[9-12].In addition, without specific eye treatment for DME, hemodialysis could significantly decrease the central retinal thickness and increase the BCVA[13-14].Various different factors including hemodynamic, metabolic, inflammatory, and fibrotic processes contribute to DN progression[15].As two parts of a body, it is not surprising that changes from the kidney have influences on retina and DME.
In this study, there were significant differences in age, diabetes course and HbA1c between two groups.The incidence of DR and DN increases with the progression of diabetes, while DME could occur at any stage of DR[16], and DME could occur before or after DN.
The CMT of DME patients with DN was severer.The dysfunction of RPE and Müller cells under hyperglycemia condition could led to the obstruction of retinal interlayer fluid removal[17].Besides, creatinine and related toxins in the blood of DN may aggravate the dysfunction of RPE and Müller cells, thus exacerbating the abnormal distribution and excessive accumulation of fluid in macular area.Furthermore,the decrease of eGFR elevates CMT value.Previous study has shown that decreased eGFR was markedly related to the presence of subretinal fluid in macular area of DME before anti-VEGF treatment[18].Meanwhile, the presence of proteinuria may affect blood osmotic pressure and lead to fluid retention in the third space.
DME patients with DN had a higher proportion of EZ and ELM discontinuity, that could be related to the dysfunction and necrosis of Müller and RPE cells, in addition, diabetic choroidopathy should also be paid enough attention.ELM is a membrane-like structure formed by the complex of Müller cells and photoreceptor cells, necrosis of Müller promotes retinal fluid accumulation, pressed peripheral blood vessels and retina result in further damage[19].The outer layer of the retina and RPE cells are supplied by choroidal blood vessels,which could be used to evaluate eye diseases and potential inflammatory response[20].Interestingly, previous studies reported that decreased choroidal thickness was correlated with damaged urinary albumin excretion rate in type 2 diabetes mellitus under DR free condition, and becoming thinner when DR advancing[21-22].And existence of ischemia could also be used to predict DR and DME progression[23-24].Those data indicated that nephropathy could influence retinopathy by decrease choroid thickness, results in reduced blood supply to RPE cells and the outer layer of retina, promotes EZ and ELM damage.HF is considered to be a marker of inflammatory response.we speculate that retinal cell damage and destruction in DME patients with DN are severer than that in DME alone, resulting in a heavier inflammatory response presented with higher amount of HF.These results indicated that DME patients with DN had worse retinal functional and structural damage before treatment, which led to higher BCVA (logMAR)in DME patients with DN than DME alone.
In DME patients with DN, CMT decreased significantly at 1mo and 3mo after treatment, but there was no significant improvement at 6mo compared with 3mo, and in some patients CMT was rebounded.This could be related to the decreased eGFR.Studies have shown that the decrease of eGFR was related to the residual subretinal fluid after 3mo of anti-VEGF treatment in DME patients[18].
The decrease of CMT in DME patients with DN after conbercept injection was slower than that in DME alone.In DME patients, aqueous levels of VEGF were significantly higher than the plasma levels[25].Activation of reninangiotensin system (RAS) also contribution to high level of VEGF, which causes more extensive damage to microvascular endothelium, retinal cells, and vascular functions.
In this study, the number of HF in DME patients with DN was always higher than that in patients with DME alone.As a marker of inflammation, the amount of HF represents the severity of the disease, a lower amount of HF indicates less tissue damage and higher integrity, while a higher amount of HF indicates more severe DME[26], and the amount of HF is negatively correlated with the prognosis of BCVA(logMAR)[27].This indicated that inflammation participates in development of DME and has impact on prognosis of DME.The decreased number of HF in this study may be related to the blocking of protein kinase C involved signal transduction by anti-VEGF treatment, thus reduce the inflammatory response.However, HF did not disappear, on the one hand, it was considered that other inflammatory factors were involved, and anti-VEGF drugs could not block its signal transduction[28]; on the other hand, inflammation gradually played more important role in the development of macular edema than vascular dysfunction.
Under this speculation that early DME may be more driven by VEGF factors, while chronic DME may be more related to inflammatory factors, combined with the CMT changes of DME patients with DN in this study, it was speculated that with the extension of DME, the proportion of VEGF participation decreases, while the proportion of inflammatory factors increases, so DME patients with DN are becoming less sensitive to anti-VEGF drugs in the later stage of treatment.Therefore, in this study, DME patients with DN received more injections in 6mo of treatment.This may provide clues of how to optimize treatment for DME patients with DN.Furthermore,anti-VEGF therapy may aggravate renal kidney damage in DME patients[29-30], which may form a vicious cycle.The pathways of anti-VEGF and glucocorticoid to work on DME is different, studies have shown that glucocorticoid vitreous implants were more effective to some refractory DME[31-32].However, side effects could not be ignored[33].It is considerable to get a counterbalance between benefit and side effects for those special DME population.
BCVA (logMAR) was significantly improved after anti-VEGF treatment in both groups compared with baseline, but the improvement in DME patients with DN was not as good as DME alone.On the one hand, the sensitivity of patients to anti-VEGF drugs may decrease with the prolonging of diabetes course, especially in long-standing DME[34-35].However, the function of retinal cells also partially determines the prognosis of BCVA (logMAR).In DME patients with DN,more extensive retinal cell and blood vessel damage induced by higher VEGF content, blocked material transport caused by thinner choroidal thickness, severer retinal compression and ischemia caused by prolonged DME, more involvement of inflammatory factors, and retinal damage caused by toxic substances in the blood, these are possible factors that may lead to retinal dysfunction, which could partially explain that,in this study, although CMT decreased in DME patients with DN after anti-VEGF treatment at 3mo, BCVA (logMAR)increased.
Previous study showed security and effectiveness of conbercept on DME within two years[36], we further explored potential influencing role of DN, and analyzed the possible mechanism.This may provide clues for prediction of treatment prognosis and optimization of treatment modalities in this population in the future.
ACKNOWLEDGEMENTS
Conflicts of Interest:Zhu YZ, None;Dou ZZ, None;Wang WY, None;Ma QY, None;Yi WD, None;Yao NN, None;Liu YC, None;Gao XD, None;Zhang Q, None;Luo WJ,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Using choroidal thickness to detect myopic macular degeneration
- lmpact of multifocal gas-permeable lens designs on short-term choroidal response, axial length, and retinal defocus profile
- Baerveldt glaucoma implant with Supramid© ripcord stent in neovascular glaucoma: a case series
- Efficacy and safety of Usights UC100 illuminated microcatheter in microcatheter-assisted trabeculotomy
- Quantifying peripapillary vessel density and retinal nerve fibre layer in type 1 diabetic children without clinically detectable retinopathy using OCTA
- Nomogram to predict severe retinopathy of prematurity in Southeast China
