OCTA characteristics in non-arteritic central retinal artery occlusion and correlation with visual acuity
2024-02-23HongXiaGongBinWuShiYongXieWeiZhangSongChen
Hong-Xia Gong, Bin Wu, Shi-Yong Xie, Wei Zhang, Song Chen
1Tianjin Key Lab of Ophthalmology and Visual Science,Department of Ophthalmology for Integrated Traditional Chinese and Western Medicine, Tianjin Eye Hospital, Tianjin 300020, China
2Clinical College of Ophthalmology, Tianjin Medical University, Tianjin 300010, China
3Eye Hospital Affiliated to Nankai University, Tianjin 300020,China
Abstract
● KEYWORDS: non-arteritic central retinal artery occlusion; fundus fluorescence angiography; optical coherence tomography angiography; retinal vessel density;visual acuity
INTRODUCTION
Non-arteritic permanent central retinal artery occlusion(NA-CRAO) is a type of small vascular stroke[1-12]that typically results in severe vision loss.The gold standard for diagnosing retinal artery occlusion (RAO) is fluorescein fundus angiography (FFA)[13-14].
Optical coherence tomography angiography (OCTA) is an advanced technology that utilizes optical coherence tomography (OCT) to provide detailed information about the blood flow parameters in different retinal layers and the choroid’s blood flow characteristics, while avoiding mydriasis[15].Compared to conventional FFA, OCTA provides higher resolution 3-dimensional images of retinal vasculature,more accurate delineation of the foveal avascular zone, and depth-resolved images of both superficial and deep vascular plexus.In contrast to FFA which can be time-consuming,invasive, and may induce adverse reactions such as nausea,vomiting, and allergies, OCTA is a valuable alternative in the early stages of acute NA-CRAO.Although OCT can diagnose and assess ischemia in NA-CRAO, it cannot visualize specific blood vessels.Therefore, this study aims to determine the role of OCTA in NA-CRAO by evaluating and comparing the changes in retinal and choroidal blood flow in different types of NA-CRAO.Furthermore, this study aims to analyze the correlation between the OCTA findings and visual acuity to identify the OCTA characteristics that could potentially assist in determining the degree of visual loss in NA-CRAO.
SUBJECTS AND METHODS
Ethical ApprovalThis study was conducted at Tianjin Eye Hospital (Heping, China) and approved by the Ethics Committee of Tianjin Eye Hospital and adhered to the principles of the Helsinki Declaration (No.2022061).Informed consent was waived due to the retrospective study.
ParticipantsThis study was a retrospective case study focusing on patients with NA-CRAO.Between September 2019 and July 2022, and a total of 92 patients (92 eyes) with NA-CRAO within 7d of symptom onset were selected for analysis.The inclusion criteria for this study were previously established NA-CRAO diagnostic criteria[15-20]: 1) Sudden and severe visual impairment; 2) The fundus optic disc is normal or pale in color, with obvious edema in the posterior pole of the retina, thin arteries, some accompanied by cherry red macula,some accompanied by slight bleeding and retinal exudation; 3)FFA shows delayed arteriovenous filling.The exclusion criteria were as follows: 1) presence of an opticociliary artery (n=9),2) history of ocular trauma or surgery (n=1), 3) other retinal diseases that could affect the observations (n=3), 4) spherical equivalent refraction >6.00 D (n=2), 5) intraocular pressure(IOP) <10 mm Hg or >21 mm Hg (n=4), 6) blood pressure exceeding 90-150/60-90 mm Hg or allergy to contrast media that prevented participation in the FFA examination (n=8), 7)visual fixation failure and inability to obtain clear parameter images (n=3).Consequently, 62 patients with acute NACRAO, corresponding to 62 eyes, were included in this study(Figure 1).The corresponding 62 healthy contralateral eyes were used as the control group.
The patients underwent examinations including bestcorrected visual acuity (BCVA), slit lamp microscopy, indirect ophthalmoscopy, fundus color photography, and OCTA.The OCTA examinations utilized 6 mm×6 mm scans with RTVue-XR Avanti.However, eight patients were excluded from the FFA due to inappropriate blood pressure levels or allergy to contrast medium.As a result, only 84 patients underwent fundus FFA examinations using Heidelberg retinal tomography.The BCVA measurements were converted to the logarithm of the minimum angle of resolution (logMAR) for analysis[16].Fundus photography imaging were performed using the Daytona system (Optos, Britain).
All participants were examined by a skilled physician.The superficial vascular plexus (SVP) was defined as 10 µm above the inner limiting membrane-inner plexiform layer (ILM-IPL);the deep capillary plexus (DCP) was 10 µm above the IPL and 10 µm below the outer plexiform layer (OPL); the outer retinal layer was 10 µm below the OPL and 10 µm above Bruch’s membrane (BRM); and the choroidal capillary was 10 µm above BRM and 30 µm below BRM.The measurement circle has an area of 3.142 mm² and is centered on the central fovea of the macula.The 6 mm×6 mm area centered on the fovea macula is subdivided as follows.The fovea refers to a circle with a diameter of 1 mm, and the parafovea refers to the area outside the 1 mm diameter and inside 3 mm diameter.Perifovea refers to the area outside the 3 mm diameter and within 6 mm diameter.
Based on the CRAO classification in Ryan’s Retina 7thed[17]and the performance of FFA and optical OCTA, we classified NA-CRAO into A type (n=29), B type (n=27), and C type(n=6) NA-CRAO, based on the degree of visual loss, retinal edema, and arterial blood flow delay.In the A type NA-CRAO group, the optic disc was slightly edematous, with a slightly lighter color.There were scattered retinal cotton plaques,some hemorrhages, and no macular cherry red spots.FFA revealed slower filling of arteries and veins and leakage in the late stage.OCTA showed decreased vessel density (VD),and B-scan OCTA showed retinal edema with visible layers and accompanied by fovea hyperreflective.The B type NACRAO group exhibited edema in the optic disc with pale color.Significant edema was observed in the posterior pole of the retina, possibly accompanied by retinal cotton spot,hemorrhage, and macular cherry red.The delayed filling in arteries and veins was more obvious.OCTA showed a greater VD reduction.B-scan OCTA showed more significant fovea hyperreflective and blurred retinal layers.In the C type NACRAO group, retinal edema in the posterior pole was more obvious, possibly accompanied by cherry red spots and minimal retinal hemorrhage.FFA: Only the header of the peri disc artery was seen.Leakage or segmental blood vessels were seen in the late stage, while large areas of the macula and periphery lacked perfusion.OCTA showed the most significant decrease in VD, while B-scan OCTA showed significant retinal edema with fuzzy layers.Macular edema and subretinal fluid were also present (Figures 1 and 2).

Figure 2 Representative images of patients with different types of NA-CRAO A: Lefteye of a 72-year-old man with history of hypertension with A type NA-CRAO onset 76h.Visual acuity was 0.2 (decimal).A1: Fundus photography showed multiple cotton spots (arrows) around the optic disc and slight macular swelling; A2: OCTA showed decreased vessel density and absence of blood flow signal in capillaries (arrow); A3:B-scan OCTA image showed macular edema and fovea involvement; A4: Choroidal blood flow area is 1.898 mm2.B: Lefteye of a 66-year-old female with history of hypertension with B type NA-CRAO onset 54h.visual acuity was 0.01 (decimal).B1: Fundus photography showed optic disc edema, obvious macular and posterior polar retinal edema (blue arrow), and macular cherry-red spots (red arrow); B2: OCTA showed more vessel density decrease and absence of blood flow signal in branch vessels (arrow); B3: B-scan OCTA image showed retinal edema, fovea hyperreflective, and inability to detect the fovea; B4: Choroidal blood flow area is 1.591 mm2.C: Lefteye of a 64-year-old man with C-type NACRAO onset 17h.Visual acuity was hand motion.C1: Fundus photography showed mild optic disc edema, obvious macular edema, and macular cherry-red spots (arrow); C2: OCTA showed significantly lower vessel density and disconnected branches in the retinal blood vessels (arrows);C3: B-scan OCTA image showed obvious retinal edema, fuzzy hierarchy, and macular edema; C4: Choroidal blood flow area measured is 1.059 mm2.NA-CRAO: Non-arteritic permanent central retinal artery occlusion; OCTA: Optical coherence tomography angiography.
Statistical Analysis Data analysis was performed using SPSS 26.0.Normally distributed measurement data are expressed as mean±standard deviation (SD) and were compared using one-way ANOVA followed by the post hoc LSD method for pairwise comparisons.Measurement data that did not conform to normal distribution are expressed as median (quartile range)and were compared using the Kruskal-WallisHtest, followed by the Nemenyi method for pairwise comparisons.Theχ2test was used to compare groups of classification and counting data.Spearman’s correlation analysis was used to determine the correlations between each index and the logMAR BCVA.P<0.05 was considered statistically significant.
RESULTS
Basic Data Details regarding patients’ basic information are presented in Table 1.There were no statistically significant differences in age, gender, and intraocular pressure among the three types and the control group (P>0.05) except for BCVA(P<0.001).The logMAR BCVA of A type was significantly better than that of B type and C type (F=15.524,P<0.001).

Table 1 Comparison of basic data among the groups
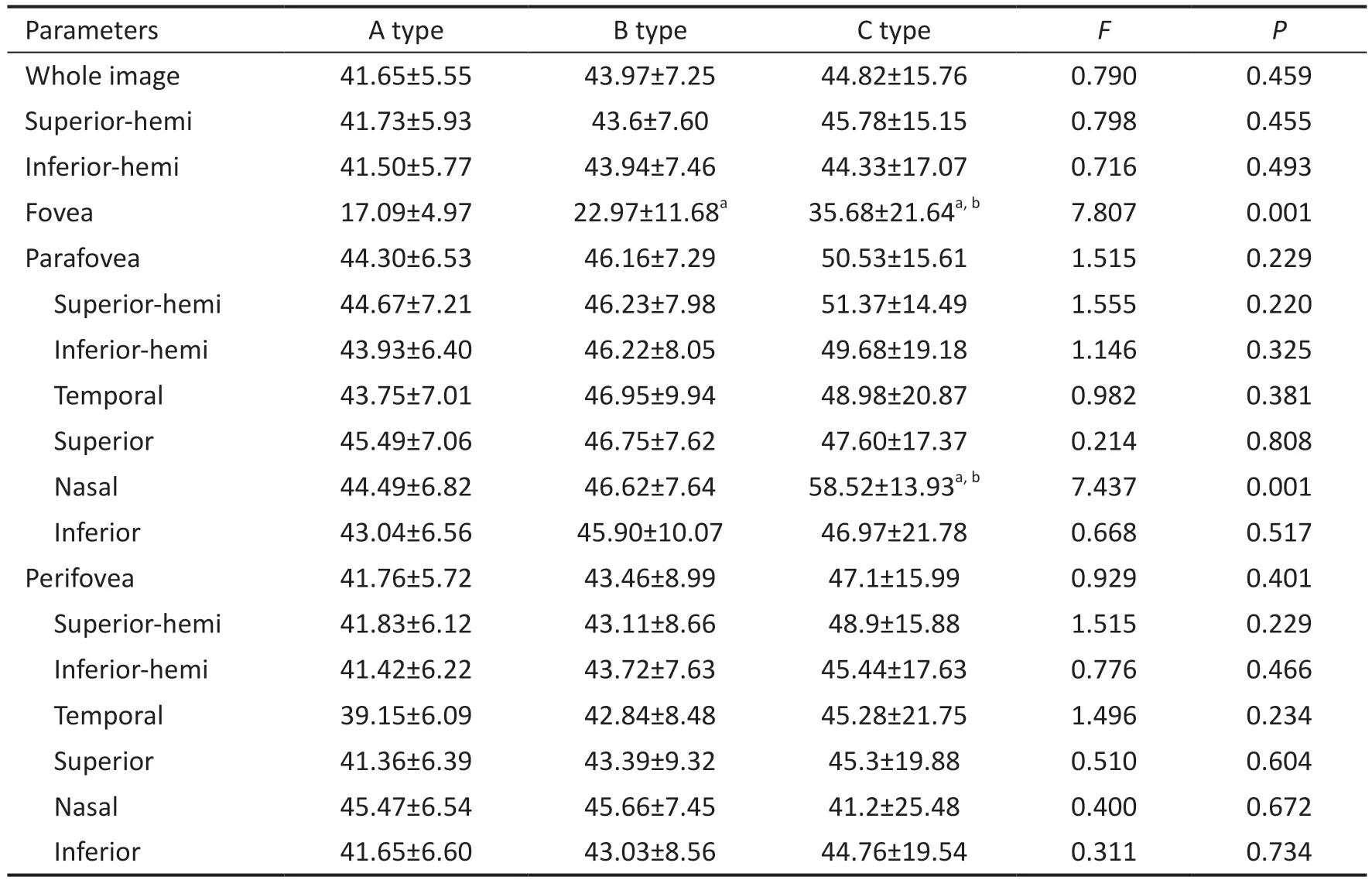
Table 2 Comparison of the SVP vessel density in the whole image and different regions mean±SD (%)
However, there was no significant difference in the logMAR BCVA between B and C type NA-CRAO.In type B, cherryred spots were in 12 eyes (44.4%); In type C, cherry-red spots were in 3 eyes (50%), macular cystoid edema in 4 eyes(66.7%), macular subretinal fluid in 2 eyes (33.3%).One eye had cystoid macular edema and subretinal fluid, and 2 eyes had cystoid macular edema and cherry-red macular edema.
The vessel density in superficial vascular plexus (VD-SVP)was the lowest in A type followed by B type, then C type at central fovea (F=7.807,P=0.001; Table 2) and nasal parafovea(F=7.437,P=0.001).There were no significant differences in the other regions among the three groups.
In addition to the fovea, OCTA showed that concerning DCP density, the C type group decreased the most.However, no significant differences were observed among the three groups(Table 3).Deep retinal vessels are the common damage targets of all types of NA-CRAO.Furthermore, the macular retinal thickness of the C type was significantly higher than that of the A and B types (Table 4), so an increase in macular retinal thickness may be associated with severe visual impairment.There was no significant difference in the outer retina flow area among the three groups (F=1.681,P=0.431; Table 5).Interestingly, the choroidal blood flow area of the A type NA-CRAO was significantly higher than that of the C type NA-CRAO (F=8.025,P=0.018; Table 5), so a decrease in choroidal blood flow area may be associated with severe visual impairment.
Spearman’s Correlation AnalysisThe logMAR BCVA was found to have a positive correlation with the vessel density of the superficial central fovea and the nasal vessel density in the parafoveal region (r=0.679, 0.826,P=0.031, 0.013),as depicted in Figures 3 and 4.However, no significant correlation was observed between the logMAR BCVA and the SVP, DCP densities in other regions, outer retinal blood flow area, and choroidal blood flow area.
Comparison with the Control GroupIn the whole-image analysis, the control group VD-SVP was 47.73%±5.98%,VD-DCP was 53.93%±6.47%, macular retinal thickness was279±10.85 μm, choriocapilaris flow area was 2.038±0.05 mm2,and outer retina flow area was 0.53±0.08 mm2.

Table 3 Comparison of the vessel density of the DCP in the whole image and different regions mean±SD (%)
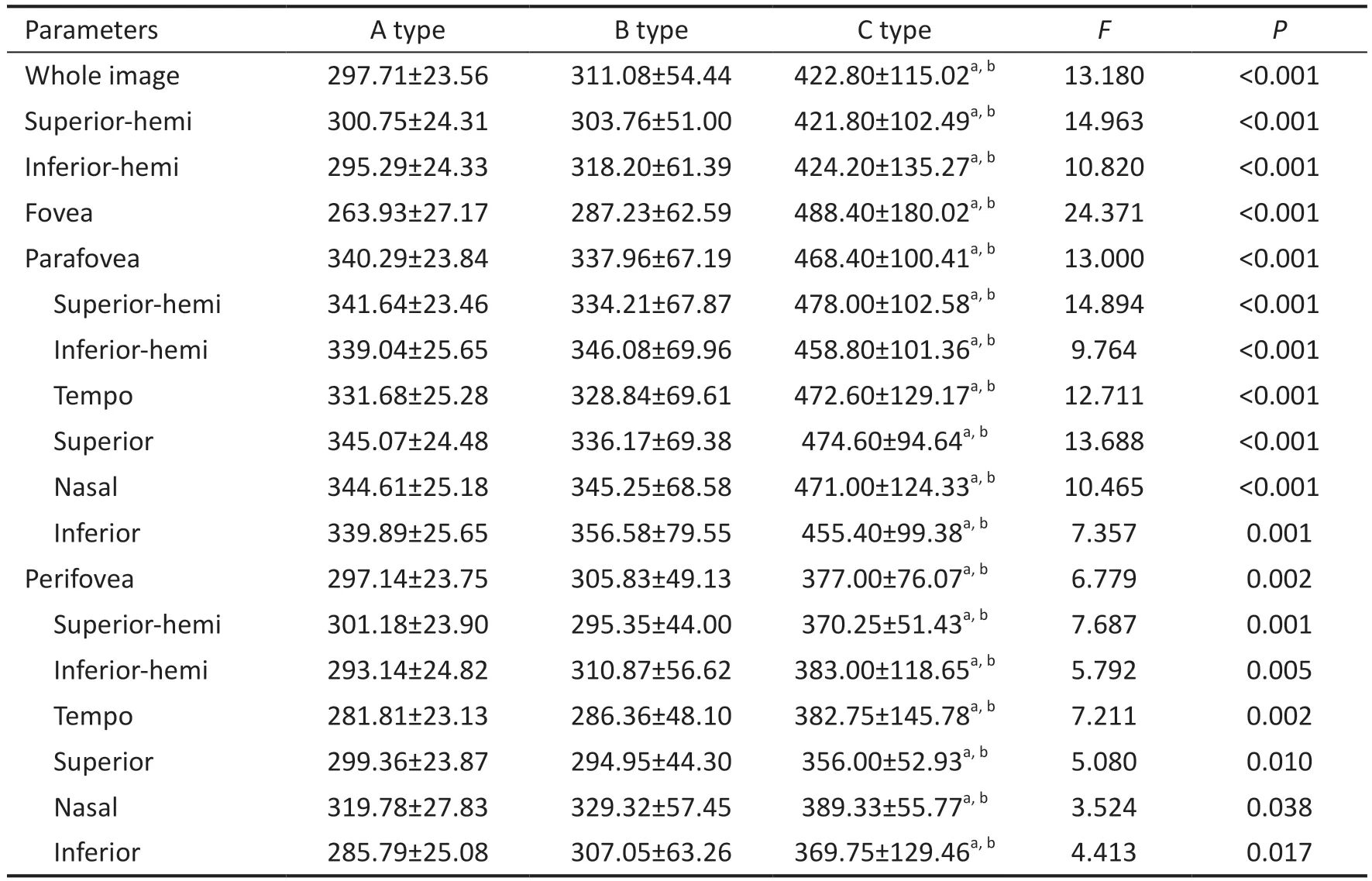
Table 4 Comparison of the thickness of the macular retina in the whole image and different regions mean±SD, µm

Table 5 Comparison of outer retina flow area and choriocapillaris flow area median (quartile range), mm2

Figure 3 Correlation between logMAR BCVA and vessel density in the superficial central fovea (r=0.679, P=0.031) BCVA: Best corrected visual acuity.
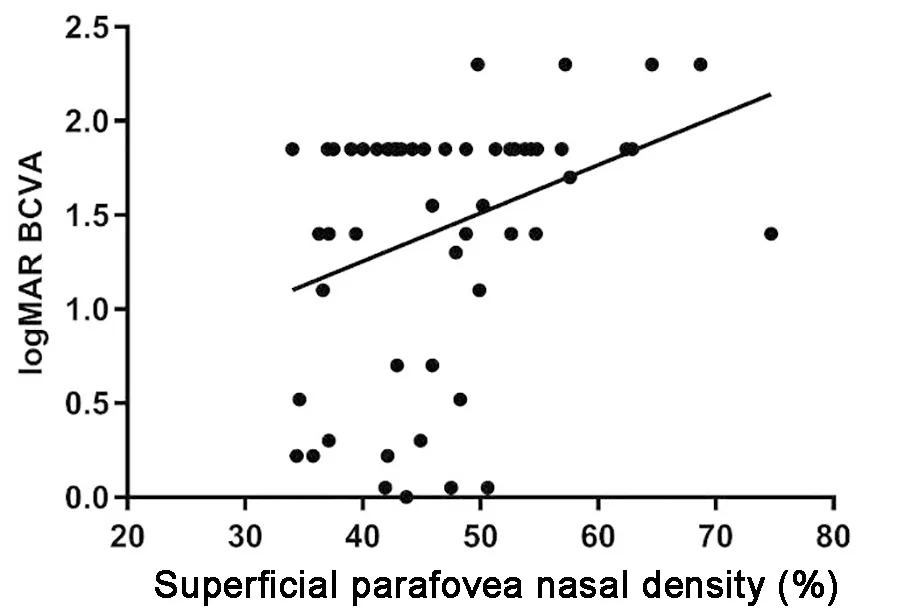
Figure 4 Correlation between logMAR BCVA and nasal vessel density near the superficial central fovea (r=0.826, P=0.013) BCVA:Best corrected visual acuity.
In the whole-image analysis, the A type group exhibited a significant decrease in VD-SVP (t=-0.028,P=0.014)compared to the corresponding control group, along with a significant decrease in VD-DCP density (t=0.058,P=0.000)and a significant increase in the outer retina flow area (t=2.42,P=0.031).There was no significant difference in choriocapilaris flow area and retinal thickness (t=0.315, 1.535,P=0.17, 0.136,respectively).Similarly, the B type group showed a significant decrease in the VD-DCP (t=0.098,P=0.031), particularly in parafovea and perifovea.Moreover, the choriocapillaris flow area was significantly decreased (t=-2.362,P=0.036)compared to the control group.There was no significant difference in VD-SVP density, retinal thickness, outer retina flow area compared to the control group (t=-0.427, 1.216,1.117,P=0.485, 0.244, 0.286, respectively).In comparison to the control group, the C type group had significantly lower VD-DCP (t=-5.618,P=0.005), especially in perifovea and parafovea-tempo, higher retinal thickness (t=27.06,P=0.000),lower outer retina flow area (t=4.68,P=0.018), and lower choriocapillaris flow area (t=-13.05,P=0.001).There was no significant difference in VD-SVP compared to the control group (t=-0.255,P=0.899).
DISCUSSION
This study aimed to investigate the changes in retinal blood vessels resulting from NA-CRAO, including a reduction in VD-SVP and VD-DCP and choroidal blood flow area in the acute stage.The decrease in VD and choroidal blood flow area in the superficial and deep retina varied according to the type of NA-CRAO.The VD in the superficial central fovea and nasal retina close to the superficial central fovea was significantly correlated with visual acuity in the acute stage.Therefore, OCTA examination in the acute phase may aid in evaluating retinal ischemia and visual function impairment in the affected eyes, with potential markers such as the VD in the superficial central fovea and nasal retina near the superficial central fovea[21-22].
In the acute stage, the A type NA-CRAO is mainly characterized by decreased VD-SVP and VD-DCP compared to a healthy eye.In contrast, the B type is mainly characterized by changes inVD-DCP and choroidal blood flow.In C type NACRAO, there were significant effects on the VD-DCP, outer retinal layer, and choroidal blood flow areas.Additionally,retinal thickness significantly increased in C type NA-CRAO,whereas VD-SVP did not change significantly.These findings indicate that NA-CRAO affects different vessels depending on the type and that changes in deeper and broader retinal layers result in poorer visual acuity.
Significant differences in superficial foveal VD, superficial parafoveal nasal VD, retinal thickness, and choroidal blood flow area among the different types of NA-CRAO, confirming their unique properties on OCTA.In the A type NA-CRAO,the VD of the superficial central fovea showed the greatest decrease, but the VD of the deep layer did not differ from the other two groups.Additionally, the vessels of the outer retina and choroid were well preserved, along with visual acuity.The VD of the superficial central fovea in B type NA-CRAO was intermediate compared to the other two groups.However,the VD in other parts of the SVP and DCP, the blood flow area of the outer retina and choroid, and the thickness of the retina were not as favorable as in A type NA-CRAO.The visual acuity was notably worse, but there were no significant differences between the B and the C types.In cases of C type NA-CRAO, the most striking feature was the marked visual impairment.The VD of the superficial central fovea and the degree of significant retinal edema were significantly higher than in the other two groups, while the choroidal blood flow area was significantly lower than in the A type.Compared with the other two groups, the C type group had extensive ischemic changes throughout the retina and choroid.Therefore, the OCTA’s retinal and choroidal blood flow parameters are useful for evaluating ischemia characteristics.
OCTA is a valuable tool for evaluating NA-CRAO as it allows for visualization of both superficial and deep blood vessels and acquisition of corresponding parameters in addition to retinal tomographyviascanning.Previously, research on NACRAO mainly relied on FFA and OCT findings[14,23].However,FFA is a lengthy and invasive examination that may not be necessary during the early stage of acute NA-CRAO due to potential side effects.While OCT has some diagnostic value, it cannot visualize vessels in detail, highlighting the importance of OCTA in identifying different types of NA-CRAO and providing information on choroidal blood flow.
NA-CRAO classification holds clinical significance as it provides insights into the degree of ischemia at different vessel levels and is associated with baseline visual acuity.In this study, visual acuity was negatively correlated with VD in the superficial central fovea and the nasal side near the superficial central fovea.This correlation may be due to central artery occlusion and distortion of the inner retinal tissue, leading to an increased VD in the fovea to compensate for the injury.Superficial retinal vessels directly connect large and small vascular networks of the retinal arteries and veins and supply all other vascular plexuses, including the deep retinal vascular layer[24].The compensatory response of superficial vessels in the nasal side of the fovea and paracentral fovea is more significant due to the presence of double capillaries around the optic disc and the macular area, containing 50% of the retinal ganglion cells[25].The correlation results show that this compensation may be a serious manifestation of visual impairment, consistent with the findings of Wanget al[26], who demonstrated compensatory effects between the optic disc and macula in a highly myopic low-oxygen environment.
No significant differences were observed in VD-DCP among the three groups.However, compared to the control group, the NA-CRAO groups exhibited significant vessel loss in the DCP.In the acute stage of NA-CRAO, the disease may directly affect the deep retinal vessels, with the extent and depth of retinal involvement varying based on the degree of ischemia.Additionally, the choroidal blood flow areas in both the B and C types were lower than in the control group.Specifically, the choroidal blood flow areas in the C type were significantly lower than those of the A type, suggesting the presence of choroidal dysperfusion in severely affected NA-CRAO cases.Mastropasquaet al[27]have suggested that choroidal capillary density is related to retinal ischemia in fluorescein angiography.Ahnet al[23]found that the choroidal thickness beneath the macular fossa was reduced in the acute stage of severe CRAO compared to the contralateral eye, indicating acute choroidal ischemia, which is consistent with our study findings.Choroidal ischemia can lead to thinning of the retinal outer layer and damage to photoreceptors, resulting in a permanent visual loss in CRAO-affected eyes[23,28].Therefore, a decrease in choroidal blood flow area may serve as a distinctive factor indicating severe visual function impairment in NA-CRAO.Although the outer retina mainly relies on choroidal blood flow, it can also be affected by inner ischemia.
This study has several limitations.First, it is a retrospective study, with inherent limitations in data collection and analysis.Second, some patients had difficulty fixating during OCTA image acquisition due to the extended collection time and difficult segmentation.Further research is needed to overcome these obstacles.Additionally, the time interval between the onset of symptoms and the first clinic visit varied from 1h to 7d among the patients analyzed, which could have influenced the baseline OCTA results.Nevertheless, this study provides important insights into the changes in retinal and choroidal blood flow in patients with NA-CRAO and evaluates the baseline factors affecting visual acuity using OCTA parameters.These findings provide valuable information on OCTA manifestations in eyes affected by NA-CRAO.Yilmazet al[29]used OCT to evaluate the degree of disorganization of the retinal inner layer (DRIL) and regarded it as a prognostic factor for patients with CRAO, and correlating it with final vision;They concluded that an increase in macular retinal thickness at baseline is associated with severe visual impairment, with changes in the nasal retina being closely related to visual function.This is consistent with our study.However, their study did not examine changes in blood flow in different retina and choroid layers, which our study compensates for.
NA-CRAO is currently a challenging and difficult disease to treat[3,30-31].We studied the changes in retinal and choroidal blood flow in patients with NA-CRAO using OCTA and observed the differences in different categories of NA-CRAO.Deep retinal vessels are the common damage targets of various types of NA-CRAO.In different types of NA-CRAO, the more outer the layer of retinal choroidal vessels, the wider the longitudinal range, and the worse the visual acuity.The VD of the superficial fovea and nasal retina near the superficial fovea may be reliable markers of visual impairment in NA-CRAO.Increased macular retinal thickness and choroidal ischemia may be associated with severe visual impairment.
ACKNOWLEDGEMENTS
Author’s contributions:Gong HX: Study design, data interpretation, manuscript preparation, funds collection; Wu B: Data collection, statistical analysis, manuscript preparation;Xie SY: Data collection, data interpretation, literature search;Zhang W and Chen S: Literature search.All authors read and approved the final manuscript.
Foundation:Supported by Tianjin Key Medical Discipline(Specialty) Construction Project (No.TJYXZDXK-016A).
Conflicts of Interest: Gong HX,None;Wu B,None;Xie SY,None;Zhang W,None;Chen S,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Using choroidal thickness to detect myopic macular degeneration
- lmpact of multifocal gas-permeable lens designs on short-term choroidal response, axial length, and retinal defocus profile
- Baerveldt glaucoma implant with Supramid© ripcord stent in neovascular glaucoma: a case series
- Efficacy and safety of Usights UC100 illuminated microcatheter in microcatheter-assisted trabeculotomy
- Quantifying peripapillary vessel density and retinal nerve fibre layer in type 1 diabetic children without clinically detectable retinopathy using OCTA
- Nomogram to predict severe retinopathy of prematurity in Southeast China
