Glaucoma drainage device implantation and cyclophotocoagulation in the management of refractory glaucoma after Descemet-stripping automated endothelial keratoplasty
2024-02-23MinShuWangXueChuanDongMiYunZhengXiangFanGeGeXiaoJingHongLingLingWu
Min-Shu Wang, Xue-Chuan Dong, Mi-Yun Zheng, Xiang Fan, Ge-Ge Xiao, Jing Hong,Ling-Ling Wu
1Department of Ophthalmology, Peking University Third Hospital, Beijing 100191, China
2Key Laboratory of Restoration of Damaged Ocular Nerve,Beijing 100191, China
3NIMO Ophthalmology Research Institute, Beijing 100176,China
4Department of Ophthalmology, the First Hospital of Putian,Teaching Hospital, Fujian Medical University, Putian 351100,Fujian Province, China
Abstract
● KEYWORDS: glaucoma drainage device implantation;cyclophotocoagulation; refractory glaucoma; Descemetstripping automated endothelial keratoplasty
INTRODUCTION
With remarkably reduced damage and enhanced prognosis, Descemet-stripping automated endothelial keratoplasty (DSAEK) has rapidly become the preferred surgical procedure replacing penetrating keratoplasty (PKP)for corneal endothelial disorders.Since significantly less tissue is transplanted in DSAEK surgery, allograft rejection has been reported to be less frequent and milder compared to PKP[1].DSAEK also induces fewer disturbances on the anterior chamber and less astigmatism[2].With the introduction of DSAEK and the elimination of some factors responsible for glaucoma escalation after PKP, there was optimism that the prevalence and severity of postoperative glaucoma would be reduced after this procedure[3].Unfortunately, recent studies showed that DSAEK is associated with a similar incidence of postoperative glaucoma[4-6].Mechanisms of post-DSAEK glaucoma included postoperative pupillary block intraocular pressure (IOP) elevation, steroid-induced glaucoma, and patients with pre-existing glaucoma, that worsening of the IOP control requiring additional medication or surgery[7].The IOP can be affected by the inflammation induced by DSAEK procedure, as well as the medications after the operation.Refractive glaucoma after DSAEK was reported to significantly lower the corneal graft survival and ruin the patients’ vision, while the treatment of which remains intractable due to the complicated ocular condition,particularly when medical treatment fails[8].The main surgical options include trabeculectomy, glaucoma drainage device implantation (GDI), and trans-scleral neodymium:YAG(Nd:YAG) cyclophotocoagulation (CPC).
Several studies have reported the factors influencing glaucoma management and graft survival in DSAEK patients with preexisting glaucoma or prior glaucoma surgery[9-10].However,studies evaluating the outcomes of glaucoma surgeries after DSAEK are limited.Some studies mentioned a few cases in which glaucoma surgeries were conducted after endothelial keratoplasty[3,11-13]with an extremely small sample size (less than 10 subjects).One study suggested trabeculectomy was effective for ocular hypertension in 20 patients after DSAEK[14].To date, no study has compared the effects of these various surgical procedures for the treatment of glaucoma in patients that had previously undergone DSAEK.Therefore, we carried out this study to present a number of peculiar cases of refractory glaucoma after DSAEK, and to compare the surgical outcomes between the two glaucoma procedures of GDI and Nd:YAG CPC.
SUBJECTS AND METHODS
Ethical ApprovalThe study was approved by the Peking University Third Hospital Ethics Committee on Research Involving Human Participants (IRB00006761-2008020).All patients read and signed an informed consent document for the DSAEK and glaucoma procedures.
This was a retrospective study that included consecutive cases of DSAEK and an anti-glaucoma surgery (either GDI or CPC) between October 2014 and September 2020 at the ophthalmology department of Peking University Third Hospital (Beijing, China).All patients represented intractable elevated IOP, which could not be controlled by medications.The glaucoma operation choices were made based on a number of factors, including the past history of glaucoma surgery,condition of the cornea, conjunctiva, anterior and posterior chamber, as well as the patient age and general health.Only patients with at least 6mo of follow-up after glaucoma surgery were included in the study.
The standard DSAEK suture pull-through technique has been described in detail in earlier publications[15].After DSAEK,all patients experienced uncontrollable IOP elevation with full anti-glaucoma medications and then accepted to have an antiglaucoma surgery.
The GDI of AhmedTMglaucoma valve (New World Medical Inc., CA, USA) implantation was performed in a standard fashion using intra-operative antimetabolites by a single surgeon[16].A cellulose sponge soaked in either 0.2 mg/mL of mitomycin C or 25 mg/mL of 5-fluorouracil was placed under the conjunctiva for 3min (in case of mitomycin C) or 5min (in case of 5-fluorouracil), followed by rinsing with phosphate buffer saline and fixation of the Ahmed valve onto the surface of sclera.As some patients had a history of different ocular diseases and surgery, they presented with wide iris anterior adherence or aniridia.To obtain patent drainage with the least influence on the endothelial graft, the drainage tubes of the valves were placed either in the anterior or posterior chamber/vitreous cavity of the eyes.All patients received topical steroid drops for 8 to 12wk postoperatively.
Contact trans-scleral Nd:YAG CPC was performed using a continuous-wave Nd:YAG laser with a hand-held fiberoptic G-probe (Oculight, IRIDEX Corporation, USA).The anterior edge of the laser probe was placed 0.5 to 1 mm posterior to the limbus with 25-30 applications of CPC at 1800-2800 mW for 2s in a 270° range, with energy level adjusted to hear the blast“pop” sound of the ciliary body.All patients received topical steroid drops for approximately 8wk postoperatively.
All patients underwent a comprehensive preoperative evaluation before and after the glaucoma surgery.Bestcorrected visual acuity (BCVA), IOP, corneal endothelium graft status, anterior and posterior segment examination results, and anti-glaucoma medications were recorded.The cup/disk ratio and Humphrey visual field were assessed in patients with clear media and at subsequent postoperative follow-up visits.IOP was usually measured using a Goldmann applanation tonometer (Hagg-Streit, Konig, Switzerland)and was occasionally measured using the Icare®tonometer(Model TAOli, Icare Finland Oy, Vantaa, Finland).Follow-up examinations were performed every 2-3mo postoperatively.The glaucoma surgery success rate was defined as an IOP value of 6-21 mm Hg without requiring an additional glaucoma procedure.Graft failure was defined as an irreversible loss of optical clarity owing to persistent corneal stromal edema.
Statistical AnalysisThe main outcome measures were postoperative IOP, glaucoma surgery success rate, number of glaucoma medications, DSAEK endothelial graft survival,and BCVA.Outcome proportions were compared using the Pearson Chi-square test with Yates’s continuity correction for small samples between the two glaucoma procedures or GDIsubgroups with different drainage tube positions.Student’st-test for paired data was used when the D’Agostino and Pearson normality test was successfully passed to compare preoperative and postoperative IOP, number of medications,and BCVA expressed in logarithm of the minimum angle of resolution (logMAR) units.When data failed to pass the normality test, the Wilcoxon paired-sample test was used.Data were expressed as mean±standard deviations, and two-tailed probability values lower than 0.05 were considered statistically significant.Data analysis was performed using IBM SPSS Statistics (release 23.0; SPSS Inc., Chicago, IL, USA).
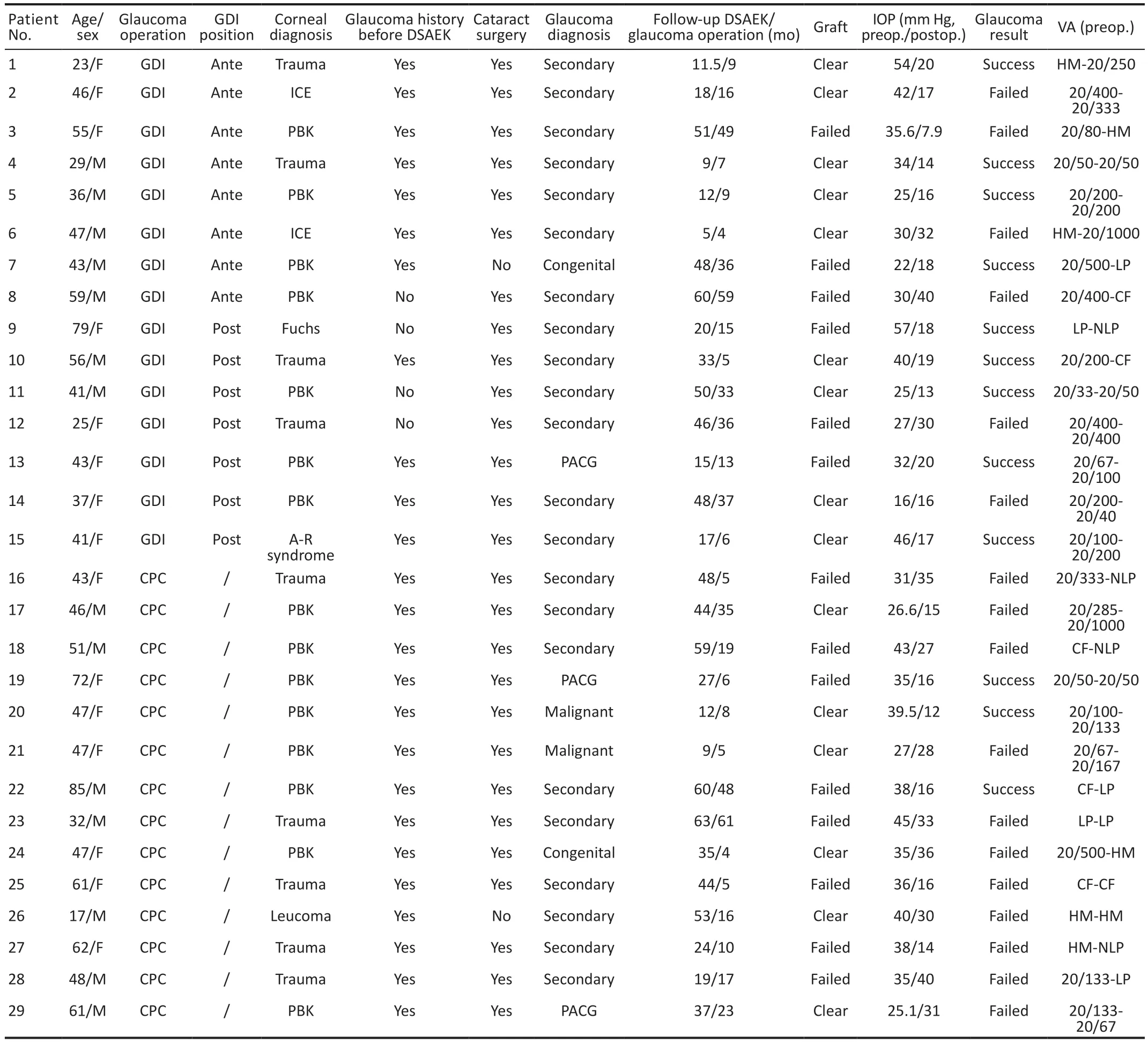
Table 1 Patient profile
RESULTS
Patient CharacteristicsA total of 29 patients were included in the study.Of these, 15 patients underwent GDI and 14 underwent Nd:YAG CPC.Table 1 summarizes the characteristics of the 29 enrolled patients.The mean age of the patients in the GDI and CPC groups was 44±14.4 (range, 23-79)y and 51±16.6 (range, 17-85)y, respectively (P=0.21,t-test).Neither preoperative IOP (P=0.79,t-test) nor BCVA (P=0.30,t-test) was significantly different between the two groups.

Figure 1 IOP status before and after glaucoma surgery Significantly reduced IOP was recorded after GDI procedure (A, P=0.006) and CPC surgery (B, P=0.003).The GDI group presented significantly better IOP control than the CPC group (C, P=0.03).IOP: Intraocular pressure; GDI:Glaucoma drainage device implantation; CPC: Cyclophotocoagulation.aP<0.05, bP<0.01.
Pseudophakic bullous keratopathy was the most common indication for initial DSAEK in both groups (n=15), and ocular trauma-related endothelial dysfunction was the second most common cause (n=9).DSAEK was performed in 2 patients with iridocorneal endothelial syndrome (ICE), and in 1 patient each of Fuchs dystrophy, Axenfeld-Rieger syndrome, and leucoma.Regarding DSAEK characteristics, 14 of the 29 patients had DSAEK alone, whereas the remaining 15 patients underwent other procedures combined with keratoplasty, such as lens phacoemulsification and posterior chamber intraocular lens implant, intraocular lens suspension or alignment, pupil formation, and anterior vitrectomy.Three of the 15 patients in the GDI group had previous keratoplasty before DSAEK but none in the CPC group underwent repeated keratoplasty.Other surgical procedures including corneal suture, cataract surgery,and vitrectomy were conducted in 11, 27, and 15 patients,respectively, among those 29 patients.
Eleven of the 15 patients in the GDI group and 14 of the 14 patients in the CPC group had glaucoma history before keratoplasty.The most common glaucoma diagnosis before DSAEK in both groups was secondary glaucoma (18 of 25 cases), while 3 patients had primary angle-closure glaucoma,2 patients had congenital glaucoma, and 2 had malignant glaucoma.Among the 25 patients with a past history of glaucoma before corneal surgery, 14 individuals had glaucoma surgery in previous to DSAEK, of which 7 were in the GDI group and 7 in the CPC group.Ten patients underwent glaucoma surgery once and 4 patients had repeated glaucoma procedures before DSAEK.The types of glaucoma procedures included trabeculectomy (10/14), CPC (4/14), GDI (3/14),and simple peripheral iridectomy during other intraocular procedures (2/14).All eyes with either past trabeculectomy or GDI had non-functional blebs and uncontrolled IOP with medications.
Follow-up periods ranged from 6mo to 5y after the glaucoma procedure.There was no significant difference in the mean follow-up after DSAEK or glaucoma procedures between the GDI and CPC groups.The interval between the latest keratoplasty and the glaucoma procedure ranged from 15d to 3.5y.
IOP MeasurementsThe IOP results before and at the last follow-up after GDI or CPC operation are shownin Table 2.There were no differences between the two different procedures in preoperative IOP (P=0.79,t-test) or postoperative IOP (P=0.41, Wilcoxon test).Both groups showed significant IOP reduction after glaucoma surgery(GDIP=0.003, CPCP=0.006, pairedt-test; Figure 1A, 1B).The percentage IOP reduction compared to baseline value was 35.4% in GDI and 26.8% in CPC group (P=0.49,t-test).The proportion of patients who developed postoperative IOP above 20 mm Hg for the GDI and the CPC groups was 33.3% and 57.1% (P=0.20, Pearson Chi-square test), respectively.None of the 29 patients developed hypotony during this study.

Table 2 IOP measurements and medications mean±SD
Figure 1C shows the significantly enhanced IOP control success rate after GDI than after CPC (P=0.03, Pearson Chisquare test).Six patients in the GDI group and 11 patients in the CPC group were considered as failure cases regarding IOP control, with a success rate of 60% (9/15) and 21.4% (3/14),respectively.Among the 15 GDI cases, 4 in 8 cases (50%)with drainage tubes placed in the anterior chamber and 5 in 7 cases (71.4%) in the posterior chamber or vitreous cavity(after vitrectomy) displayed successfully controlled IOP during the follow-up period (P=0.40, Pearson Chi-square test).For the CPC group, 5 in 11 cases (45.5%) with failed IOP control underwent repeated CPC procedure to obtain IOP below 21 mm Hg during the follow-up period.In the 6 cases with failed IOP control in the GDI group, two had needle revision of filtering blebs and 1 underwent CPC procedure.Patients in the two procedures groups received similar number of medications before and after glaucoma surgery (P=0.17 andP=0.59,t-test).Both the groups had significantly reduced medication numbers after glaucoma surgery (GDI,P=0.001 and CPC,P=0.03, pairedt-test; Table 2).

Figure 2 Comparison of endothelial graft survival and BCVA A: No significant difference was found in the proportion of patients who experienced graft failure between the two glaucoma procedures (P=0.36); B: No statistically significant differences were found in BCVA after GDI surgery; C: Significantly worse BCVA was recorded after CPC operation (P=0.006).BCVA: Best-corrected visual acuity; GDI: Glaucoma drainage device implantation; CPC: Cyclophotocoagulation.bP<0.01.
Corneal Endothelial Graft StatusThe most common etiology of graft failure was homograft rejection with anterior chamber inflammation accompanied by keratin precipitates or non-immunologic endothelial decompensation.In this study,endothelial grafts of 6 cases in the GDI group (40%) and 8 cases in the CPC group (57%) eventually failed (P=0.36,Pearson Chi-square test; Figure 2A).Among the 14 cases with graft failure, 6 cases had graft failure before the glaucoma procedure (2 in the GDI group, and 4 in the CPC group); the rest failures occurred after glaucoma operation (4 in the GDI group and 4 in the CPC group).
Before the DSAEK procedure, the average number of graft endothelial cells was 3496±709 and 3399±307 in the GDI and CPC groups, respectively, while the diameter of the endothelial graft ranged between 7.25 and 9 mm.Among the 15 patients with no remarkable corneal edema during the last follow-up, the number of endothelial cells varied from 553 to 2046, with no significant differences in the average number of endothelial cells between the two different operative groups.For the other 14 patients with graft failure, the number of endothelial cells could not be evaluated.Two patients in each group experienced early complications of endothelial graft(graft wrinkle or dislocation) and underwent further procedures after DSAEK, of which only 1 of 4 cases in the GDI group presented transparent corneal during the last follow-up.
Among the 15 GDI cases, 3 in 8 cases (37.5%) with drainage tubes placed in the anterior chamber and 3 in 7 cases (42.9%)with drainage tubes placed in the posterior chamber or vitreous cavity experienced graft failure (P=0.83, Pearson Chi-square test).
BCVAThe median BCVA for all 29 patients was 20/333 preoperatively and 20/1000 at the average 20-month followup postoperatively.For GDI surgery, BCVA improved in 4 patients, remained the same in 3 patients, and declined in 8 out of 15 patients (27%, 20%, and 53%, respectively).After the CPC procedure, BCVA increased in 1 patient, remained the same in 4 patients, and decreased in 9 out of 14 patients (7%,29%, and 64%).One patient in the GDI group and 3 cases in the CPC group were confirmed to have lost light perception during the last visit after the operation.The immediate causes for the loss of vision were not clear.
The mean preoperative and postoperative BCVA (logMAR)was 1.32 and 1.60 for the GDI group and 1.70 and 2.35 for the CPC group, respectively.The preoperative BCVA was not significantly different between the two groups (P=0.22,t-test).No statistically significant change in BCVA was found after GDI surgery, disregarding the GDI drainage tube placement(P=0.34, pairedt-test; Figure 2B).However, there was a significant worsening in BCVA of 0.65 logMAR after the CPC procedure (P=0.006, pairedt-test; Figure 2C).
DISCUSSION
The current study investigated surgical outcomes of GDI and CPC procedures on refractory glaucoma after DSAEK.All anti-glaucoma procedures were manipulated by a single surgeon.Among the large number of DSAEK cases carried out at the ophthalmology department of Peking University Third Hospital during the past 6y, only 29 patients with refractory postoperative glaucoma were recruited in this study.However,considering the small number of subjects and their rarity, this may be the largest sample size studied to date in this field.In this study, most cases had a history of preexisting glaucoma(25 of 29 cases) before DSAEK.Another notable characteristic of etiology was trauma history (9 of 29 cases).Previous studies mainly focused on the efficiency of the trabeculectomy procedure after DSAEK, as trabeculectomy might have the least influence on the endothelial graft[17].However, some glaucoma patients with DSAEK have more complicated conditions.As in this study, the average number of operations before the glaucoma procedure was >2.5.All cases presented refractory glaucoma, while not being eligible for traditional trabeculectomy.
This study demonstrated that both GDI and CPC procedures significantly decreased IOP in eyes with glaucoma after DSAEK, with a mean follow-up of 21.0mo.A similar mean IOP was observed between the GDI and CPC groups before and after glaucoma procedures.Both procedures significantly decreased the number of anti-glaucoma medications.A previous study showed that in the treatment of refractory glaucoma, Ahmed GDI and endoscopic CPC had similar success rates for IOP control (the definition of successful IOP control was similar to that used in this study)[18].However,in the current study on refractory glaucoma after DSAEK,the GDI group presented a significantly higher success rate of IOP control than the CPC group.Although with certain limitations, this study compared the efficiency of different antiglaucoma procedures in refractive glaucoma after DSAEK,similar to a previous study conducted in eyes that underwent PKP, which showed that CPC had a trend of lower success rate of IOP control than Ahmed GDI, although without statistical significance[19].Moreover, in a review describing different glaucoma procedures after PKP, GDI was proposed to be the most common and successful modality for IOP control when medications failed[20].Therefore, in terms of operative IOP control for eyes with refractory glaucoma after DSAEK, GDI seems to be more effective.
The current study found that Ahmed GDI had a 60% success rate of IOP control.The eyes with the tube position of the Ahmed valve in the anterior chamber and those in the posterior chamber or vitreous cavity presented a similar success rate for IOP control.The optimal location of the drainage tube remains controversial.Studies in PKP eyes demonstrated that vitreous cavity tube placement seemed to be more hospitable to corneal graft than anterior chamber tube placement, although a higher rate of posterior segment complications was expected as a result of vitrectomy[21-22].All cases in this study with vitreous cavity drainage tube position already had vitrectomy prior to GDI.Therefore, GDI could preferably be performed with tube placement in accordance with the patient’s anterior and posterior segment situations.
The CPC procedure had a 21% success rate for IOP control in eyes with DSAEK.A previous study in 11 eyes that underwent PKP showed that after a single application of CPC, the success rate of IOP control was 63% with an average follow-up of 23mo[19].CPC effectively reduced the IOP and the number of anti-glaucoma medications with few complications in glaucoma patients after either PKP or DSAEK[23].During the 12-month follow-up period, CPC significantly reduced the IOP of patients who underwent PKP, although with a total retreatment rate of 44%[24].In the current study involving patients undergoing DSAEK, CPC seemed to not be as effective as in patients undergoing PKP; moreover, nearly half of the failed IOP control cases underwent repeated CPC procedures during the follow-up periods.This might be attributable to the relatively low predictability of the nondirect-viewing CPC procedure.
The overall endothelial graft survival rate was 52% at 21.0mo follow-up in the current study, which was relatively lower than that reported in previous studies.A study reported a graft survival rate of 91% at 2y and 48% at 5y in 46 DSAEK cases with previous glaucoma surgeries[9].Another study suggested DSAEK is a viable alternative to PKP to restore visual function even in eyes with a GDI sited in the anterior chamber[25].However, no research on graft survival rate in patients with anti-glaucoma procedures posterior to endothelial keratoplasty,which seems to have more adverse effects on endothelial graft than surgeries prior to DSAEK, has been reported so far.The intricate ocular condition (with a previous history of trauma or multiple intraocular surgeries) could also attenuate the graft survival rate, while early complications might also account for final graft failure.GDI is considered a potent hazard to induce endothelial decompensation[26].A few studies reported that GDI was an effective method in glaucoma management but increased graft failure risk in PKP patients[16-17]and in endothelial keratoplasty patients[27-28].However, the current study found that cases with GDI after DSAEK presented an even enhanced success rate in the endothelial graft (60%)with a mean follow-up of 21.0mo compared with the CPC procedure (43%), although the difference was not statistically significant.Of note, in the GDI group, similar graft success rates were observed between eyes with anterior chamber drainage tube positions and those with posterior chamber or vitreous cavity position.This novel individual modification of the GDI drainage tube position according to different anterior segment situations during the surgical procedures could possibly explain the relatively high success rate of endothelial graft survival.Similarly, one study in patients undergoing PKP reported a trend that CPC had a higher incidence of graft failure than trabeculectomy and GDI, although without significant difference[19].
Neither of the two surgery groups displayed enhanced BCVA during follow-up, as glaucoma procedures were mainly not visual acuity-improving.Moreover, significantly worsening BCVA after surgery in the CPC group but not in the GDI group was observed.Previous studies showed that reduced vision was more prominent after CPC than after GDI in glaucomatous eyes after PKP, with various reports suggesting a vision loss between 6% and 33% after GDI surgery, but up to 56% after CPC[19].The current study provided similar results in patients with DSAEK.This might be attributable to the relatively lower success IOP control rate in the CPC group, which led to more anti-glaucoma surgeries or medications.CPC-induced inflammation in the anterior segment might also have an adverse effect on vision.
As a retrospective study and similarly to the weakness of a previous study in PKP patients[19], the two surgical groups in the current study may not be exactly comparable as the glaucoma procedure choice was not made randomly.It might be influenced by a few factors such as the past history of glaucoma surgery, condition of the cornea, conjunctiva,anterior and posterior chamber, as well as the patient age and general health.However, the preoperative characters of the two groups were relatively similar in terms of IOP and BCVA.In addition to the relatively small number of recruited patients,the follow-up time varied from 6mo to up to 5y, which might also impair the accuracy of the conclusions.Although these shortcomings limited the statistical power and were not suitable for multivariate analyses, this novel research could still provide references on the procedure selection to treat refractory glaucoma after DSAEK, especially when traditional trabeculectomy is not feasible.
In summary, this study showed that GDI manifested a significantly higher success rate for IOP control and similar endothelial graft failure rate compared with the CPC procedure for eyes with refractory glaucoma after undergoing DSAEK.
The creative individual modification of the glaucoma drainage tube position during GDI surgical procedures could possibly enhance the success rate of endothelial keratoplasty.A certain portion of patients experienced vision loss after one or repeated CPC operations, which was not observed posterior to GDI.Therefore, when trabeculectomy is not suitable,glaucoma drainage implant surgery may be preferable to CPC procedures in refractory glaucoma cases after DSAEK.Further prospective, randomized, and multicenter studies with larger sample sizes are required in the future.
ACKNOWLEDGEMENTS
Special thanks to colleagues from Department of Epidemiology, Peking University Third Hospital, for their professional advises on study design and statistics.
Authors’ contributions:Wang MS performed the clinical studies, data analysis and wrote the manuscript; Dong XC,Zheng MY, and Fan X performed the clinical studies and data recording; Xiao GG and Hong J performed DSAEK on those patients and helped with the patients’ screening; Wu LL designed the study and performed the review and modification of the manuscript.
Conflicts of Interest: Wang MS,None;Dong XC,None;Zheng MY,None;Fan X,None;Xiao GG,None;Hong J,None;Wu LL,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Using choroidal thickness to detect myopic macular degeneration
- lmpact of multifocal gas-permeable lens designs on short-term choroidal response, axial length, and retinal defocus profile
- Baerveldt glaucoma implant with Supramid© ripcord stent in neovascular glaucoma: a case series
- Efficacy and safety of Usights UC100 illuminated microcatheter in microcatheter-assisted trabeculotomy
- Quantifying peripapillary vessel density and retinal nerve fibre layer in type 1 diabetic children without clinically detectable retinopathy using OCTA
- Nomogram to predict severe retinopathy of prematurity in Southeast China
