Proposal of a modified classification for hilar cholangiocarcinoma
2024-01-13ShuaiXiangXiaoPingChen
Shuai Xiang,Xiao-Ping Chen
Abstract Hilar cholangiocarcinoma is a malignant tumor that originates from the left and right hepatic ducts and their confluence.It is highly malignant and associated with a poor prognosis.Surgical resection is the only available curative treatment option.A scientific classification system can aid in the preoperative assessment of resectability and guide the development of appropriate surgical strategies.Several classification systems are available,with the Bismuth-Corlette(BC)classification being the earliest and most widely used.Similar to many other classifications,the BC classification relies on the secondary branching of the bile ducts as an important anatomical landmark,making it unsuitable for cases with variations in the bile duct anatomy.With advances in understanding the hepatic plate and anatomical structures at the hilum,the secondary bile ducts are no longer considered important anatomical landmarks.Therefore,modifications to the BC classification are needed to align with modern anatomical improvements and advancements in surgical techniques.Herein,we propose a modification to the BC classification.In this new system,the boundary of the hilar plate is considered as limit of the proximal ductal margin and used as an anatomical landmark,rather than the concept of“secondary bile ducts”in the BC classification.
Keywords:Classification;Extent;Hepatectomy;Hilar cholangiocarcinoma
1.Introduction
In 1965,Klatskin[1]first described and popularized hilar cholangiocarcinoma as an extrahepatic malignancy originating from the left and right hepatic ducts and their confluences. The seventh edition of the American Joint Committee on Cancer(AJCC)staging system distinguishes hilar cholangiocarcinoma from distal extrahepatic cholangiocarcinoma by defining it as a tumor in the distal portion of the bile duct.Hilar cholangiocarcinoma is an invasive cancer that affects the intrahepatic bile ducts,liver parenchyma,and portal vessels. It can cause lymphatic metastasis and neural involvement.Therefore, treatment of hilar cholangiocarcinoma usually involves partial hepatectomy.[2]The core issue lies in determining appropriate liver resection strategy to remove the tumor while preserving an adequate functional liver parenchyma.Scientific staging or classification of hilar cholangiocarcinoma can help determine resectability,guide surgical planning,and predict prognosis.
2.Bismuth-Corlette classification
The Bismuth-Corlette (BC) classification of hilar cholangiocarcinoma was proposed by Bismuth and Corlette in 1975 and revised in 1988.[3]It is the most widely used classification system in clinical practice.This classification primarily divides the tumor based on its anatomical location and extent of bile duct involvement.Type I refers to tumors that invade only the common hepatic duct without involvement of the confluence of the left and right hepatic ducts.Type II involves the confluence of the left and right hepatic ducts.Type III involves the confluence of the left and right hepatic ducts and unilateral involvement of the secondary branch ducts.Type IV involves the confluence of the left and right hepatic ducts and bilateral involvement of the secondary branch ducts.Clinicians utilize this classification system for preoperative surgical planning because it is easy to understand.Type I hilar cholangiocarcinoma requires only extrahepatic bile duct resection or minor hepatectomy, whereas types II and III require combined partial liver resection. Treatment of types IIIb and IIIa hepatocellular carcinoma often involves left and right hemihepatectomies.However,type IV hilar cholangiocarcinoma cannot be radically resected.In the eighth edition of the AJCC staging system, BC type IV is no longer included in the T4 stage.[4]Nevertheless,properly selected patients with BC type IV can still undergo radical resection and achieve survival.[5]
The BC classification has certain limitations. First, the descriptions of each subtype in this system were not sufficiently precise or detailed.For example,it is uncertain whether tumors that invade beyond the confluence of the left and right hepatic ducts but do not reach the secondary branch ducts should be classified as type II or IV. It is also unclear whether unilateral secondary branch duct tumors that invade the contralateral ducts beyond the left and right hepatic ducts confluence but do not reach the secondary branch ducts are type III or IV. The BC classification mentions “secondorder bile duct branches,” but it does not emphasize their significance,confusing practical applications.
Furthermore, BC classification description and illustration may resemble a grading system.[6]“Classification” categorizes things with similar traits,whereas“grading”differentiates by quality,degree, or extent. Based on the descriptions and illustrations of the BC classification, it is assumed that the tumor cells originate from the common hepatic duct. The classification, ranging from type I to type IV,describes the extent of tumor spread from the common hepatic duct to the hilar bile ducts and subsequently to the intrahepatic ducts. Type I represents the early stage of the disease,with a small tumor that involves only the common hepatic duct and not the confluence of the left and right ducts.As the tumor progresses to the confluence of the ducts,it is classified as a type II tumor.If the tumor continued to invade the distal part of the unilateral duct,it is classified as type III.At this point,“grading”seems to reflect better the dynamic process and severity of bile duct cancer invasion along the biliary tree.However,cancer cells do not always originate from the common hepatic duct. They can occur anywhere within the biliary system, such as the left or right hepatic duct or their confluence.It is difficult to determine the specific origin of a tumor from preoperative imaging,intraoperative macroscopic observations,or postoperative histopathology.Therefore,accurate grading is challenging. Nevertheless, if the tumor progresses, it may spread to the entire hilar bile duct or even the intrahepatic ducts,making it reasonable to classify it as stage IV.
Moreover,practical applications of BC classification are limited.A key concept in the BC classification is the“second-order bile duct branches.”Type III involves the invasion of the unilateral secondary branch ducts,whereas type IV involves the invasion of the bilateral secondary branch ducts. Secondary branch ducts typically refer to bile ducts draining from different liver sectors,such as the right anterior,right posterior,left medial,and left lateral sectors.Most biliary anatomy is the formation of the right hepatic duct from the right anterior and posterior bile ducts,which subsequently join to form a common hepatic duct with the left hepatic duct(Figure 1A).This situation falls under the BC classification but may not apply to other variations of the biliary tree.When the right anterior or right posterior bile ducts join the left hepatic duct(Figures 1B,C)or merge to form the common hepatic duct (Figure 1D), the right secondary branch ducts directly join the confluence of the bile ducts.Tumor invasion of the confluence indicates right secondary branch duct involvement. However, it becomes difficult to determine whether it should be classified as type II or III using the BC classification.
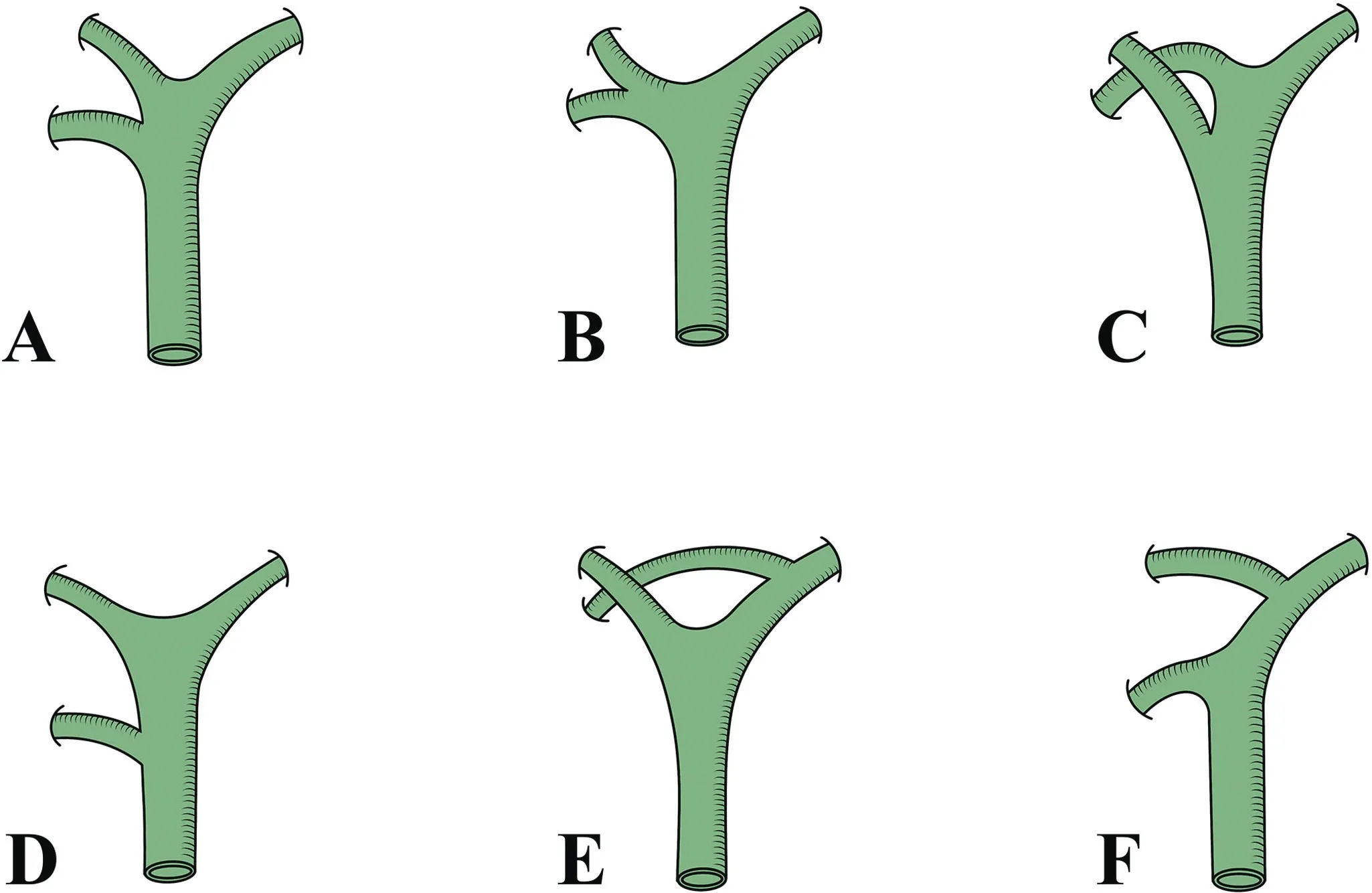
Figure 1. Common variations of hepatic ducts at the liver hilum.A,Trifurcation type. The left hepatic duct, right anterior sector duct,and right posterior sector duct converge to form the common hepatic duct. B, The most common anatomical variation is the“presence of a right hepatic duct” type. The right anterior sector duct and right posterior sector duct converge to form the right hepatic duct, which then joins the left hepatic duct to form the common hepatic duct. C, The convergence point of the right anterior sector duct shifts downward to the common hepatic duct.D, The convergence point of the right posterior sector duct shifts downward to the common hepatic duct. E, The right posterior sector duct converges with the left hepatic duct. F, The right anterior sector duct converges with the left hepatic duct.
3.Other staging systems for hilar cholangiocarcinoma
Other commonly used staging systems for hilar cholangiocarcinoma include the AJCC TNM staging system,which was updated in the eighth edition; the Blumgart-Jarnagin Memorial Sloan Kettering Cancer Center (MSKCC) T staging system proposed by Blumgart in 1997 and revised by Jarnagin in 2001[7,8];and the Clavien staging system proposed by the International Cholangiocarcinoma Collaborative Group in 2011.[9]
These 3 staging systems describe tumor invasion of the biliary anatomy and assess the tumor invasion of the surrounding tissues,such as the portal vein, hepatic artery, liver parenchyma, lymph nodes,and distant metastasis.The MSKCC T and Clavien staging systems also assess residual liver volume. T3 stage has essentially negligible resectability and involves unilateral secondary branch ducts and contralateral hepatic atrophy according to MSKCC T staging.The Clavien staging system describes the tumor size and macroscopic pathological subtypes(sclerosing,nodular,and papillary),making it the most comprehensive staging method available for evaluating and describing nearly all aspects of hilar cholangiocarcinoma.These staging systems complement and enhance the BC classification to varying degrees. By utilizing these staging systems, a more accurate assessment of the resectability,surgical approach selection,and prognosis can be achieved for hilar cholangiocarcinoma.
Despite these advancements, these staging systems still share a common characteristic with the BC classification when describing longitudinal tumor involvement along the bile ducts.They all considered the secondary branch ducts to be important anatomical landmarks for tumor invasion along the longitudinal axis of the bile ducts.Consequently,their applicability to all variations of the biliary tree is limited, similar to that of the BC classification, which restricts their clinical utility.An improved classification system is still needed.[6]
4.Anatomical variations and relationships between hilar bile ducts and portal vein
The hepatic artery, portal vein, and bile duct, forming the triad of Glisson,enter the liver parenchyma enveloped by Glisson capsule.Within the Glissonian system,the triad of structures is closely gathered and bundled; however, below the hepatic plate, these structures run separately,[10]exhibiting various anatomical variations. Anatomical variations in the portal vein and bile duct and their spatial relationships are significant in surgical procedures for hilar cholangiocarcinoma.
The most common anatomical type of right bile duct is the“presence of a right hepatic duct”type,where the right anterior sectoral and right posterior sectoral bile ducts merge to form the right hepatic duct,which then joins the left hepatic duct to form the common hepatic duct(Figure 1A).Other types include the“absence of the right hepatic duct” type, which comprises 3 situations: the downward migration of the confluence point of the right bile duct,the division of the bile duct into 3 branches,and the joining of the right bile duct with the left hepatic duct. Downward migration of the right bile duct confluence point means the duct directly joins the common bile duct from the right anterior or posterior sector(Figures 1E and F).The division of the bile duct into 3 branches refers to the common formation of the confluence points of the right anterior,right posterior,and left hepatic ducts to create the confluent portion of the common hepatic duct(Figure 1D).Joining of the right bile duct with the left hepatic duct can occur with the right posterior sectoral bile duct joining the left hepatic duct,accounting for approximately 20%,or with the right anterior sectoral branch joining the left hepatic duct,accounting for approximately 6%of cases(Figures 1B and C).[11,12]
Variations were more common in the left bile duct. The most common type involves the confluence of B2 and B3, which then joins B4 to form the left hepatic duct(Figure 2A).However,this type accounts for only 30%of the cases,with some studies reporting a variation as high as 69.1%.[13]The joining point of B4 can shift to the left or right of a typical position,resulting in different variations,depending on the location at which B4 joins the left bile duct.For example,the confluence portion of B2,B3,and B4 formed the B2,B3,and B4 duct confluence types(Figure 2B),and the leftward joining of B4 created the B3 and B4 duct confluence types(Figure 2C).
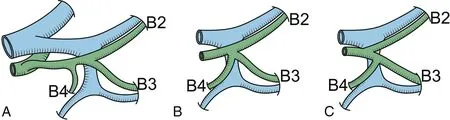
Figure 2. Common variations of the left hepatic duct (viewed from cranial to caudal). A, Type B2,3. B, Type B2,3,4. C, Type B3,4. The number indicates the segmental bile duct(B)according to Couinaud hepatic segment.
The portal vein develops from the early embryonic vitelline and umbilical veins and generally exhibits limited variation in its main branches. The most common anatomical type of portal vein is the bifurcation type, where the right anterior and posterior sectoral branches merge to form the right branch of the portal vein,accounting for 73.9%to 89%of the cases.The right branch of the portal vein is typically shorter, and its length depends on the location of the right anterior branch sprouting from the right posterior sectoral branch.In addition,6.1%to 7.7%of individuals have a trifurcation type,where the branching point is precisely located at the junction of the portal vein's left and right branches,and 4.7%to 17.4%have the right anterior branch joining the left portal vein.[11,14]Bile duct variations are often present when they occur in the portal vein.Variations in the bile duct are often present as well.[14]
In addition to understanding variations in the portal vein and bile ducts,it is important to analyze their anatomical positional relationships.The left side of the liver is relatively thin,and the bile duct usually runs on the cranial side of the portal vein.It is rare for individuals to exhibit a“southern loop”variant,where the bile duct is located on the caudal side of the portal vein.The right liver is thicker,and there are more variations in the positional relationship between the bile duct and portal vein.The most significant relationship was found between the right posterior branch of the bile duct and the right anterior branch of the portal vein.The right posterior branch of the bile duct commonly circum-passes the right anterior branch of the portal vein,moving from the cranial side to the dorsal and caudal sides, a phenomenon referred to as“northern looping”(Figure 3A).This anatomical relationship accounts for approximately 80% to 85% of the population. In another 15% to 20% of individuals, the right posterior branch of the bile duct runs on the ventral and caudal sides of the right anterior branch of the portal vein,a condition known as“southern looping”(Figure 3B).In patients with“southern looping,”the position of the right posterior branch of the bile duct is more superficial,making it easier to dissect the bile duct without obstruction from the right anterior branch of the portal vein after opening the Glisson sheath(Figures 3C and D).Higher rates of negative resection margins can typically be achieved compared with those with the northern looping.[15]In cases where the right posterior branch of the bile duct exhibits northern looping,resection of the right anterior branch of the portal vein may be necessary to obtain sufficient resection margins and expose the bile duct for biliary-enteric anastomosis,which may involve resection of the right anterior sector of the liver(Figures 3E and F).
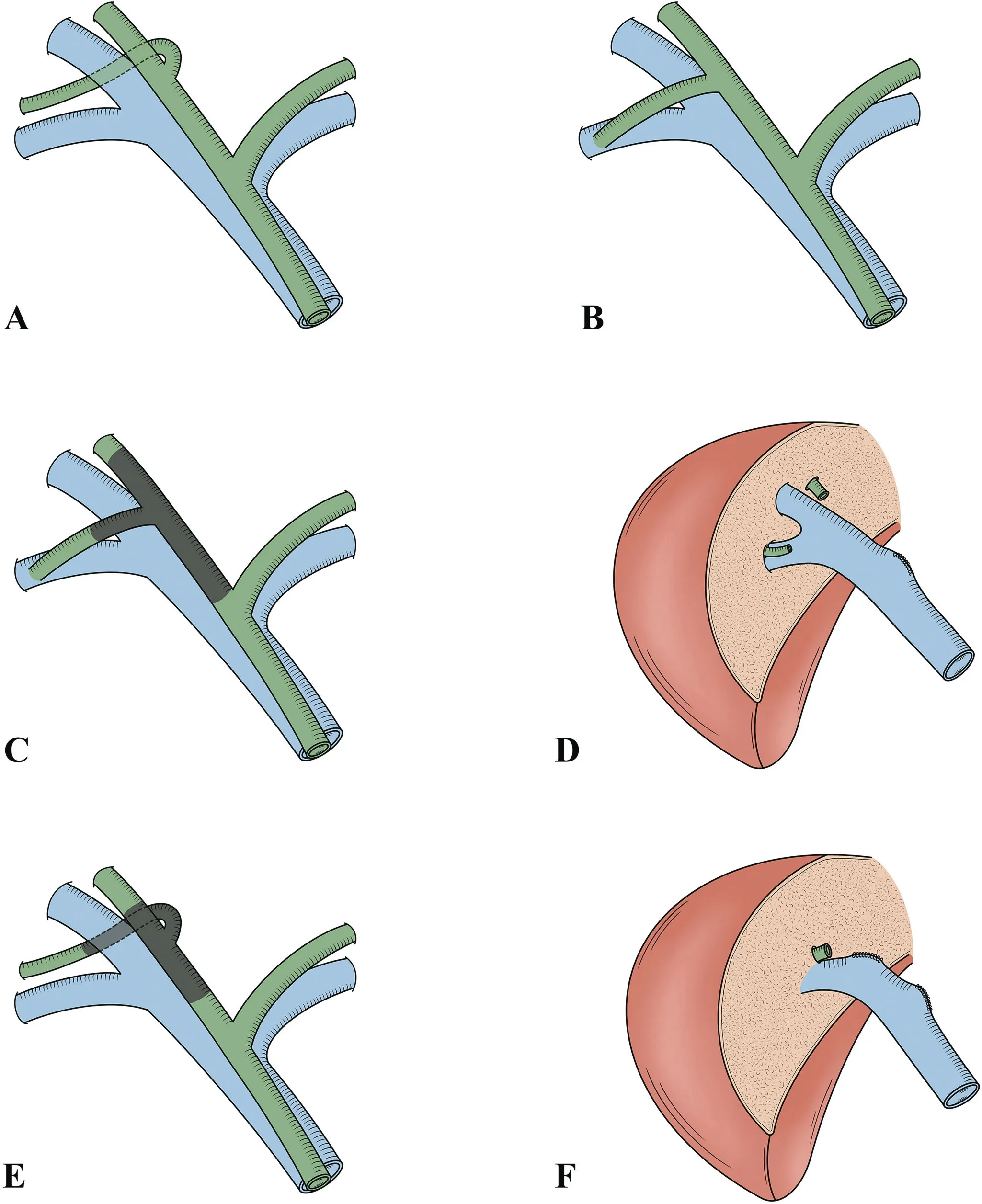
Figure 3. Variations in the relationship between the right posterior sector duct and the portal vein. A, Northern loop, where the right posterior sector duct runs on the cranial side of the right anterior branch of the portal vein. B, Southern loop, where the right posterior sector duct runs on the caudal side of the right anterior branch of the portal vein.
5.Modification of the BC classification for hilar cholangiocarcinoma
Surgery is the main treatment of hilar cholangiocarcinoma. Local tumor invasion, vascular invasion, lymph node metastasis, neural invasion,and distant metastasis affect postoperative survival.Assessing many of these factors preoperatively is difficult,and postoperative pathology is often needed for tumor staging and prognosis. Thus,preoperative classification is most useful for determining the appropriate hepatectomy technique and its extent.
The key aspect of curative resection for hilar cholangiocarcinoma is the complete tumor removal while ensuring an adequate blood supply to the residual liver. Therefore, the focus should be on whether the tumor or planned tumor-free resection line crosses the boundaries of important portal vein branches,rather than whether the tumor involves the secondary branches of the bile duct.
The left edge of the umbilical portion of the portal vein(umbilical portion of the left portal vein,U-point)and the right edge of the bifurcation of the anterior and posterior branch of the right portal vein(origin of the right posterior portal vein, P-point) (Figure 4A)have been proposed as anatomical landmarks to determine the proximal resection point of the bile duct during hepatectomy for trisegmentectomy.[16-18]These anatomical landmarks have been widely adopted. When the tumor was located between the U- and P-points,the liver resection range was the resection of segment 4/4b(Figure 4B). Segment 4/4b resection should be a routine step in the surgical treatment of hilar cholangiocarcinoma.There are 2 reasons for this. First, segment 4 is anatomically closest to the hilar region and is often affected by tumor invasion.Second,the surgical field is visualized from the ventral-caudal side to the dorsal-cranial side,and resection of segment 4/4b provides good exposure of the hilar structures,facilitating surgical maneuvering and gastrointestinal reconstruction. During the segment 4/4b resection, the left edge (U-point)corresponded to the resection line of the right trisegmentectomy,and the right edge corresponded to the left hepatectomy(P-point).When the tumor was located between the left edge of the U-point and the right edge of the P-point,the liver resection range included the resection of segments 4/4b,5,and 8(Figure 4C).In cases with a northern looping variant of the right posterior branch of the bile duct,which is obscured by the head side of the right anterior branch of the portal vein,it is usually necessary to resect the right anterior branch of the portal vein and the right anterior lobe of the liver to ensure that the resection margin of the right posterior branch of the bile duct reaches the right edge of the P-point.In this situation,additional segments 5 and 8 resection based on segment 4/4b resection is known as mesohepatectomy.The right resection margin during central hepatectomy corresponded to the left trisegmentectomy.Some authors argued that left trisectionectomy might not be needed to achieve curative resection in some cases with a“southern looping”variant, even if the tumor infiltrates the right secondary bile ducts(Figures 3C and D).[15]This approach allows the preservation of more residual liver tissue.For patients with localized tumor invasion,sufficient resection margins can be achieved with mesohepatectomy.The more extensive procedures of hemihepatectomy or even extended hemihepatectomy may not be necessary. This approach maximizes the preservation of the viable liver parenchyma and reduces the incidence of postoperative liver failure.
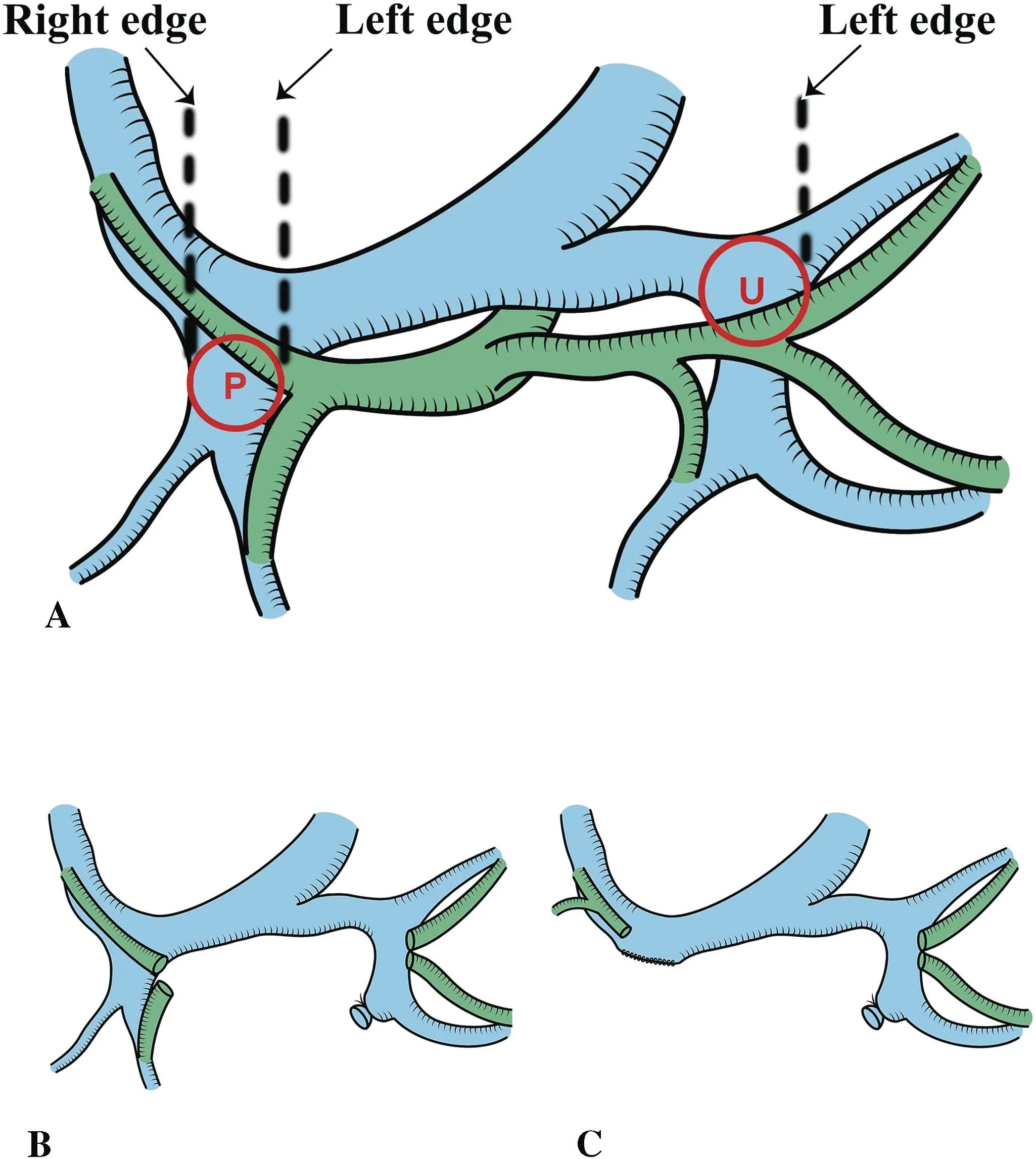
Figure 4. Important portal vein branches and corresponding liver resection extent(viewed from cranial to caudal).A,Diagram illustrating the locations of the U- and P-points, and their corresponding anatomical boundaries. The U-point is where the vertical part of the portal vein originates from the hilum. The left margin of the U-point represents the left margin of the vertical part of the portal vein.The P-point is where the right anterior branch originates from the right branch of the portal vein. B, Illustration after resection of segment 4/4b of the liver. C, Illustration after combined resection of segment 4/4b and segments 5 and 8 of the liver.
Recently,some authors have proposed a new classification of hilar cholangiocarcinoma using a combination of U-point and P-point anatomical landmarks based on 3-dimensional imaging techniques.They classified tumors limited to the bile duct without P- and U-point involvement,vascular invasion,or hepatic atrophy as type I and recommended minor liver resection as the surgical approach.Tumors that invaded either one of the anatomical landmarks (Uor P-point)or 1-sided vessels or resulted in unilateral liver atrophy while the contralateral side remained intact were classified as type II,and partial hepatectomy or trisegmentectomy was recommended.Tumor extension to both the P- and U-points, tumor extension to the P-point(U-point)with left(right)vascular invasion or left(right)hepatic atrophy,tumor involvement of the main PV or proper HA,and metastasis were all categorized as type III.In such cases,systematic treatment was recommended.They believe that this new classification predicts resectability effectively and demonstrates better efficacy in determining surgical prognosis.[19]This classification system effectively integrates the advantages of the existing staging systems.Its major improvement lies in replacing the concept of secondary bile ducts with portal vein anatomical landmarks,emphasizing the preservation of the portal vein as a crucial aspect of surgical resection,and overcoming the difficulties in classifying patients according to the BC classification caused by biliary anatomical variations.
As the bile ducts run separately from blood vessels within the plate system,the invaded bile duct can be resected without hepatic parenchymal resection when cancer cells affect the bile duct within the plate system.[10,20]Thus,the boundary of the hilar plate should be used as the anatomical landmark for evaluating resectability rather than the U-or P-point.Recently,researchers conducted studies on cadaveric liver specimens to investigate the practical boundary of the hilar plate(PBHP)and determine the limit of the proximal ductal margin.[21]They found that the proximal bile duct could be dissected further than conventional anatomical landmarks,with an average distance of 5 to 10 mm.[21]The median distance from the extreme separation point on the right side to the P-point was 6.9 mm,whereas that from the extreme separation point on the left side to the U-point was 8.9 mm.In some cases, the PBHP was almost identical to the anatomical landmarks,indicating that the vascular systems should not be separated beyond the anatomical landmarks.[21]
Based on current advancements in anatomy and a deeper understanding of the hilar plate,we propose the following modifications to the Bismuth classification for hilar cholangiocarcinoma and the corresponding extent of liver resection.Type I refers to tumors involving only the common hepatic duct without bifurcation of the bile duct,for which liver resection may not be necessary or may be limited to S4b.Type II refers to tumors in which the left margin does not reach the left PBHP, and the right margin does not invade the left margin of the P-point with a recommended S4 resection.Type II+refers to tumors in which the left margin does not reach the left PBHP, the right margin reaches the left margin of the P-point but does not involve the right PBHP,and the extent of liver resection includes S4,5,8 (ie, mesohepatectomy). Type IIIa includes tumors in which the left margin does not involve the left PBHP,and the right margin exceeds the right PBHP. The therapeutic strategy for such cases typically involves right hemihepatectomy with S4b or right trisegmentectomy.Type IIIb was defined as tumors in which the left margin exceeded the left PBHP,and the right margin did not reach the left margin of the P-point, with a recommendation for left hemihepatectomy. Type IIIb+ represents tumors in which the left margin exceeds the left PBHP,the right margin reaches the left margin of the P-point but does not involve the right PBHP,and the recommended liver resection range is a left trisegmentectomy.Type IV refers to tumors involving bilateral PBHPs with wide-ranging tumor involvement that cannot be resected in a 1-stage procedure and requires reevaluation after neoadjuvant treatment.
Similar to the BC classification,the modified classification does not include information on vascular invasion or liver atrophy. Instead,it focuses on whether the tumor involves important vascular anatomical landmarks and the PBHP. This approach maintains the simplicity of the BC classification.It no longer considers the secondary bile duct as a significant anatomical marker,thus overcoming limitations in the application of BC classification due to bile duct variations. The introduction of the PBHP as an anatomical landmark in this new classification is based on a comprehensive understanding of the hilar plate structure.This inclusion aims to maximize the R0 resection rate and surgical resectability while conserving a greater portion of the liver parenchyma. Accurate determination of PBHP is crucial in this classification. Preoperative techniques,such as multidetector computed tomography and 3-dimensional reconstruction, can help determine the relationship between the bile duct and blood vessels.The distance between the bile duct and the hepatic artery suddenly decreases to less than 1 mm and can be considered as approaching the PBHP.[21]It should be mentioned that achieving the PBHP during surgery also requires meticulous dissection to avoid injuring the hepatic artery(Figure 5).
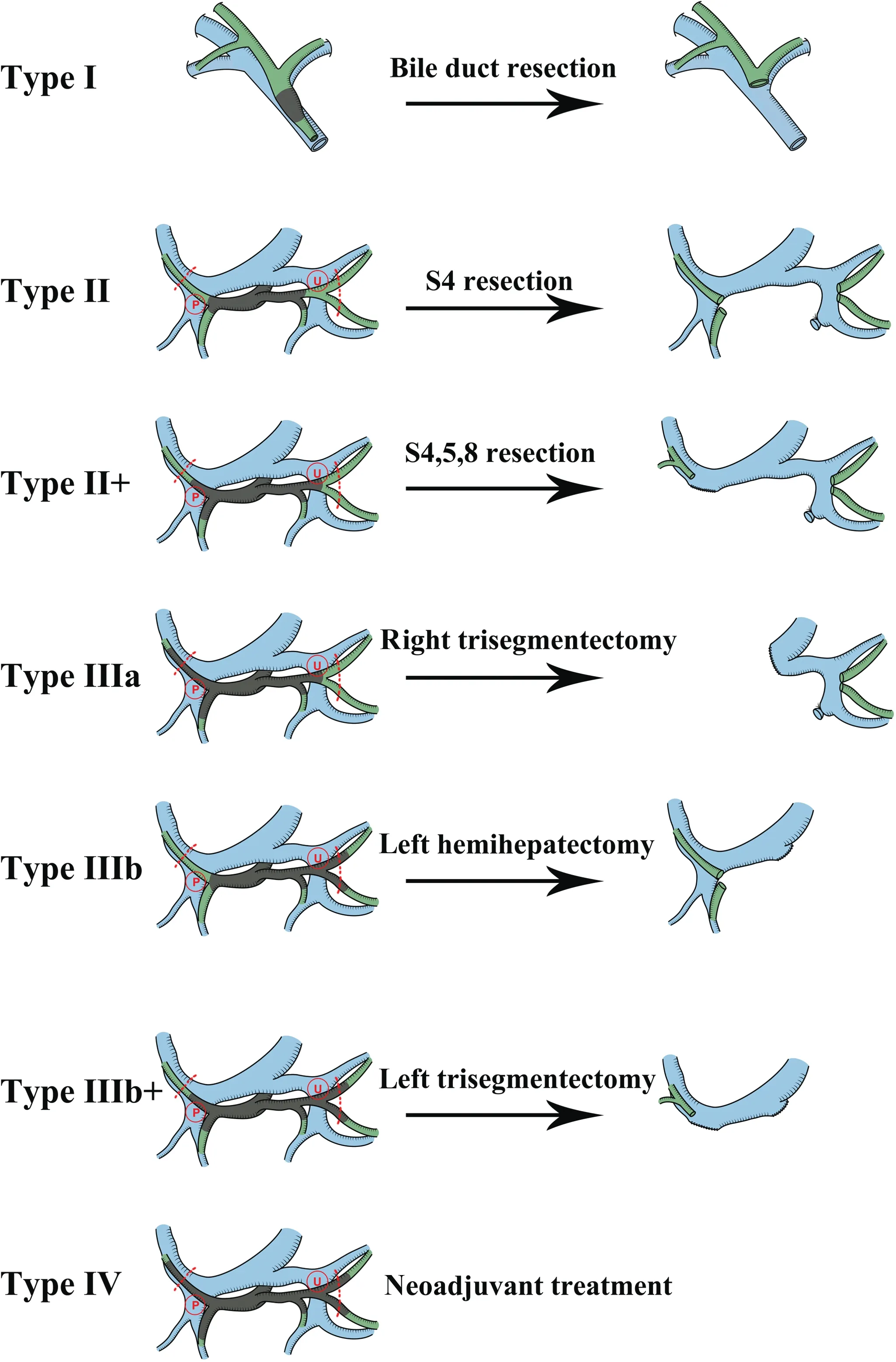
Figure 5. Modified classification of hilar cholangiocarcinoma and the corresponding resection extent (viewed from cranial to caudal). U,umbilical portion of the left portal vein,U-point;P,origin of the right posterior portal vein, P-point. Red dotted line: practical boundary of the hilar plate.
6.Conclusion
Hilar cholangiocarcinoma treatment requires radical resection with adequate residual liver volume.Although these tumors are generally small, their location in a particular anatomical region surrounded by important and complex neighboring ductal structures emphasizes the crucial importance of liver resection method and its extent.Bismuth-Corlette classification is the most widely used hilar cholangiocarcinoma classification.Understanding the anatomy of the hilar plate and improving hepatic surgery techniques have led to a shift in the criteria for irresectability.Involvement of the secondary bile duct is no longer the sole criterion for irresectability.We proposed modifying the BC classification for clinical application and better liver resection assessment.In this new system,PBHP is considered a limit of the proximal ductal margin and used as an anatomical landmark rather than“secondary bile duct”concept in BC classification.Further validation using additional clinical data is necessary to validate this modified classification.
Acknowledgments
We are very grateful to Ms. Mengli Gao,from the Department of Surgery, Tongji Medical College, Huazhong University of Science and Technology,for drawing the pictures for this article.
Financial support and sponsorship
This research was funded by the Department of Science and Technology of Hubei province, (Clinical Medical Research Center of Liver Surgery,CXPTZX005).
Conflicts of interest statement
X.-P.Chen is an editorial board member of Oncology and Translational Medicine.This article is subject to the journal's standard procedures, with peer review handled independently of the relevant editorial board member and his/her research groups.
Author contributions
Draft preparation,review and editing,Shuai Xiang;funding acquisition and supervision, Xiaoping Chen; All authors have read and agreed to the published version of the manuscript.
Data availability statement
Not applicable.
Ethical approval
Not applicable.
杂志排行
Oncology and Translational Medicine的其它文章
- Xiao-Ping Chen:the “Master of the Scalpel” who saves lives by entering the forbidden territory of hepatopancreatobiliary surgery
- Chinese expert consensus on laparoscopic hepatic segmentectomy and subsegmentectomy navigated by augmented-and mixed-reality technology combined with indocyanine green fluorescence imaging
- Immunotherapy for mucosal melanoma
- Development of therapeutic cancer vaccines using nanomicellar preparations
- Pancreatic cystic neoplasms:a comprehensive approach to diagnosis and management
- FGF2 promotes the chemotherapy resistance in colon cancer cells through activating PI3K/Akt signaling pathway
