Effects of intravenous infusion of esketamine on analgesia and postpartum antidepressant after cesarean section
2023-12-29SUNShansuXUZhixinSUNHu
SUN Shan-su, XU Zhi-xin, SUN Hu
The Second Affiliated Hospital of Hainan Medical University, Haikou 571000, China
Keywords:Esketamine Cesarean section Postpartum depression Pain
ABSTRACT
1.Introduction
Cesarean section is a common surgical procedure in obstetrics and gynaecology.Effective pain management for women is essential to reduce maternal stress and promote postoperative recovery.Postpartum depression (PPD) is a common type of perinatal psychiatric disorder that occurs during the first six months after delivery[1], and untreated PPD can cause extreme sadness and anxiety in the maternity, preventing the maternity from bonding with the baby or breastfeeding.Studies have shown[2] that the risk of postpartum depression increases by 63% after cesarean section, and acute pain after cesarean section may develop into persistent pain, leading to increased opioid use in pregnant women,delaying postoperative functional recovery, and increasing the risk of postpartum depression.The N-methyl-D-aspartate (NMDA)receptor antagonist ketamine provides analgesia while producing rapid-onset antidepressant effects as a novel antidepressant in antidepressant therapy[19-20].Esketamine, as the dextrosome body of ketamine, also has analgesic and antidepressant effects[21], and has fewer adverse effects than ketamine.However, Few studies on the use of esketamine in cesarean delivery have been reported..This study investigated the effects of different doses of esketamine given intravenously on analgesia and postpartum depression after cesarean section.
2.Materials and methods
2.1General information
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Hainan Medical College with the number LW2021020.From November 20 2020 to January 30 2022, 435 maternity who underwent cesarean section surgery under combined spinal and epidural anesthesia in the Second Affiliated Hospital of Hainan Medical College were selected, with ASA grade I-II,singleton full-term expecting for delivery, aged 20~41 years.Exclusion criteria: contraindications to combined spinal and epidural anesthesia, history of psychiatric illness and chronic pain, severe medical comorbidities, and difficulties in doctor-patient cooperation.Rejecting standard: local anesthetic allergy and anesthesia effect is not ideal, the blocking plane higher than T6, BMI40 kg/m2,changing the anesthesia method, and the late loss of follow-up.Evaluated by preoperative visits and the EPDS Score Scale, the EPDS Score Scale is one of the simplest and most reliable screening tools for postpartum depression, with a score of 9/10 indicating that the maternity has a depressive state, and women with a score higher than 12/13 are likely to have postpartum depression.The random number table method was used to divide into three groups: HE(0.4 mg/kg esketamine); LE(0.2 mg/kg esketamine); C (normal saline).There was no significant difference between the three groups of general data (P>0.05) and were comparable.
2.2 Research methods
Routine ECG monitoring is performed after the maternity enters the operating room.Routine placement, disinfection, clothing, L3-4 space puncture, subarachnoid retraction cerebrospinal fluid smooth injection of 0.5% ropivacaine 2.5 mL, epidural catheter to the head end of 5 cm, immediately after the completion of anesthesia to raise the right buttock of the mother to prevent supine hypotension syndrome.Control the plane of anesthesia not exceeding T6.Intraoperative systolic blood pressure < 90 mmHg or 20% lower than basal blood pressure, intravenous attention to norepinephrine tartrate injection 4~8 μg, heart rate less than 50 times/minute intravenous atropine 0.3-0.5 mg.5 min after the fetus is delivered, esketamine is dissolved in 40 mL of normal saline according to kg/body weight, and the test drug or normal saline is continuously pumped intravenously for 40 min at a speed of 60 mL/h.The control group was pumped with saline.After the operation, the maternal patient was given self-controlled analgesia, dose: sufentanil 2.5 μg/kg +ondansetron 8 mg + normal saline a total of 100 mL, background dose 2 mL/h, patient’s self-controlled analgesia 0.5 mL/time, lock time set to 15 min, and tell the patient how to use the analgesic pump correctly.
2.3 Study parameterss
The primary study parameters were VAS scores, Ramsay sedation scores and sufentanil consumption at T0’, T1’, T2’, T3’ and T4’over 24 h, and secondary study parameters were EPDS scores for all maternity were assessed using the Edinburgh Postnatal Depression Scale (EPDS) for scores one day preoperatively, one day postoperatively at follow-up, three days, one week (telephone follow-up) and six weeks (telephone follow-up) postoperatively.Intraoperative MAP and HR at entry (T0), skin incision (T1), start of drug pumping (T2), pumping for 10 min (T3), pumping for 20 min(T4), end of drug pumping (T5), end of surgery (T6) and adverse reactions at leaving the room were recorded.The occurrence of adverse reactions was observed and recorded at the postoperative follow-up.A score ofon the EPDS scale was diagnosed as as a positive screening indicator for postnatal depression in this study.
2.4 Statistical processing
SPSS 23.0 software was used for statistical analysis of the data.The measurement data were expressed as mean ± standard deviationor median (maximum and minimum), VAS score, sufentanil consumption and EPDS score were analyzed by multifactorial repeated measures ANOVA, and the count data were expressed as percentages using chi-square test, and P<0.05 was considered statistically significant difference.
3.Results
3.1 Comparison of MAP, HR in three groups
There was no statistically significant difference between the groups in the three groups for intraoperative MAP and HR at each time point (P>0.05).See Table 1 and Table 2.
Tab 1 Comparison of maternal MAP between the three groups(mmHg, )
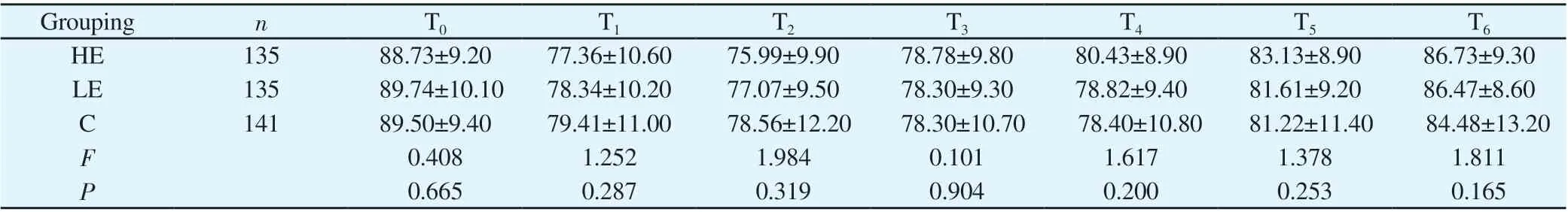
Tab 1 Comparison of maternal MAP between the three groups(mmHg, )
Grouping n T0 T1 T2 T3 T4 T5 T6 HE 135 88.73±9.20 77.36±10.60 75.99±9.90 78.78±9.80 80.43±8.90 83.13±8.90 86.73±9.30 LE 135 89.74±10.10 78.34±10.20 77.07±9.50 78.30±9.30 78.82±9.40 81.61±9.20 86.47±8.60 C 141 89.50±9.40 79.41±11.00 78.56±12.20 78.30±10.70 78.40±10.80 81.22±11.40 84.48±13.20 F 0.408 1.252 1.984 0.101 1.617 1.378 1.811 P 0.665 0.287 0.319 0.904 0.200 0.253 0.165
Tab2 Comparison of maternal HR in the three groups (times/min, )

Tab2 Comparison of maternal HR in the three groups (times/min, )
Grouping n T0 T1 T2 T3 T4 T5 T6 HE 135 89.52±11.00 80.33±14.10 83.10±11.50 85.02±10.30 85.73±10.20 84.10±9.10 82.90±9.40 LE 135 88.59±11.20 81.19±12.50 82.61±11.50 84.47±10.10 84.55±11.80 83.73±9.20 82.50±9.90 C 141 90.30±10.90 80.42±13.20 83.13±11.10 83.58±9.80 83.70±8.90 82.39±9.50 80.80±9.10 F 0.815 0.171 0.090 0.696 1.297 1.273 1.623 P 0.443 0.834 0.914 0.499 0.276 0.281 0.199
3.2 Comparison of VAS scores and sufentanil consumption between the three groups
The differences in VAS scores and sufentanil consumption were statistically significant (P < 0.05) in the HE and LE groups compared to group C.See Tables 3 and 4.
3.3 Comparison of EPDS scores between the three groups
Compared to C, the EPDS scores were lower in the HE versus LE at one day postoperatively (P<0.05) and in the HE versus LE group at three days postoperatively (P<0.05); the EPDS scores were not statistically significant in the three groups at one week and six weeks postoperatively (P>0.05).See Table 5.
3.4 Comparison of maternal adverse reactions in the three groups
There was no statistically significant difference in the incidence of nausea and vomiting when the three groups left the room (P>0.05);the incidence of dizziness and diplopia was higher in the HE and LE compared to C (P<0.05); the incidence of hallucinations was higher in the HE, but there was no statistically significant difference between the three groups (P>0.05).There were no adverse reactions of hallucinations, drowsiness or pruritus in the three groups at postoperative follow-up, and the differences in the incidence of dizziness, nausea and vomiting and diplopia were not statistically significant in the three groups (P>0.05).See Table 6.
Tab3 Comparison of maternal VAS scores in the three groups (scores,)
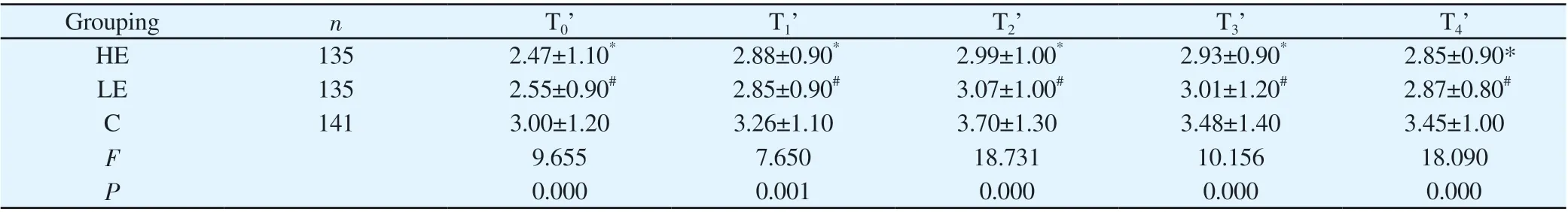
Tab3 Comparison of maternal VAS scores in the three groups (scores,)
Note: Comparison with Group C.* indicates P<0.05, # indicates P<0.05
Grouping n T0’ T1’ T2’ T3’ T4’HE 135 2.47±1.10* 2.88±0.90* 2.99±1.00* 2.93±0.90* 2.85±0.90*LE 135 2.55±0.90# 2.85±0.90# 3.07±1.00# 3.01±1.20# 2.87±0.80#C 141 3.00±1.20 3.26±1.10 3.70±1.30 3.48±1.40 3.45±1.00 F 9.655 7.650 18.731 10.156 18.090 P 0.000 0.001 0.000 0.000 0.000
Tab4 Comparison of maternal sufentanil consumption in the three groups (μg,)

Tab4 Comparison of maternal sufentanil consumption in the three groups (μg,)
Note: Comparison with Group C.* indicates P<0.05, # indicates P<0.05
Grouping n T0’ T1’ T2’ T3’ T4’HE 135 6.97±1.10* 14.18±2.30* 28.21±4.20* 42.36±6.40* 83.37±13.10*LE 135 7.18±1.20# 14.32±2.40# 28.34±4.90# 42.53±6.80# 83.97±13.50#C 141 7.81±1.60 15.60±3.10 30.56±5.10 45.58±7.40 88.93±13.90 F 14.742 11.969 10.316 9.113 6.857 P 0.000 0.000 0.000 0.000 0.001
Tab5 Comparison of EPDS scores between the three groups (points, )
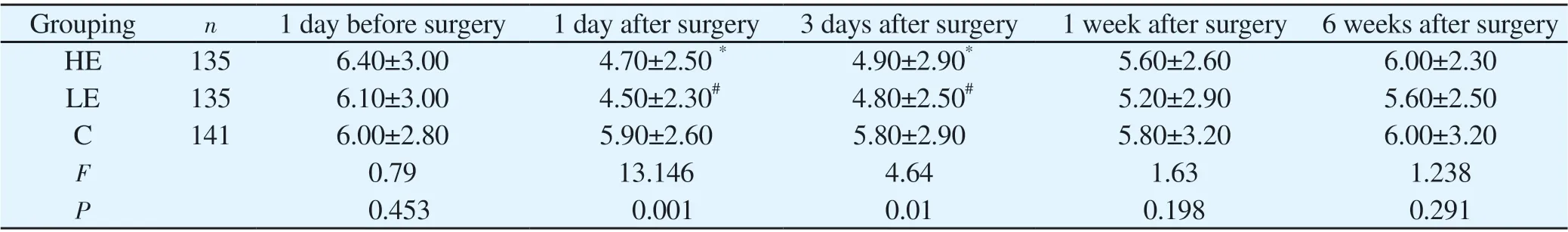
Tab5 Comparison of EPDS scores between the three groups (points, )
Note: Comparison with Group C.* indicates P<0.05, # indicates P<0.05
Grouping n 1 day before surgery 1 day after surgery 3 days after surgery 1 week after surgery 6 weeks after surgery HE 135 6.40±3.00 4.70±2.50 * 4.90±2.90* 5.60±2.60 6.00±2.30 LE 135 6.10±3.00 4.50±2.30# 4.80±2.50# 5.20±2.90 5.60±2.50 C 141 6.00±2.80 5.90±2.60 5.80±2.90 5.80±3.20 6.00±3.20 F 0.79 13.146 4.64 1.63 1.238 P 0.453 0.001 0.01 0.198 0.291
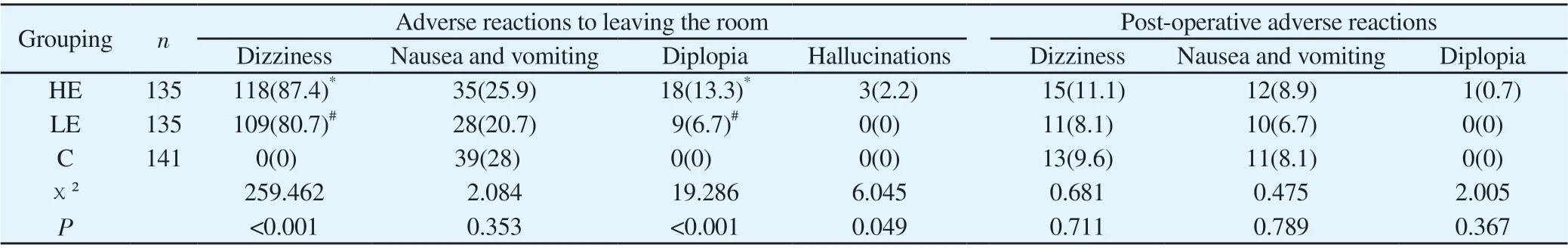
Tab6 Comparison of maternal adverse reactions in the three groups (%)
4.Discussion
Lack of analgesic means after caesarean section can lead to persistent pain and even a risk of developing chronic postoperative pain.With central sensitisation and nociceptive hypersensitivity due to injurious stimuli triggered by tissue injury, the body still perceives and amplifies pain after the injurious stimuli have ceased [3].The use of opioids in the perioperative period or in moderate doses in the postoperative period can help to relieve persistent pain caused by tissue damage.Pain after caesarean section is inextricably linked to postpartum depression[4].Most drugs can only relieve post-caesarean pain or reduce depressive symptoms alone; and few drugs can relieve both pain and PPD.Ketamine, as an NMDA receptor antagonist, can block and reverse central sensitization, reduce opioid tolerance, and have a rapid antidepressant effect at the same time[5].Esketamine is the right-hand side of ketamine and has an antidepressant mechanism similar to that of ketamine and has a higher affinity for NMDA receptors compared to ketamine, being approximately 2~4 times more potent[6] and 2~4 times more potent for theμ-andκ-receptors of opioids than R(-) ketamine[7].Thus, esketamine requires a lower dose to produce anesthesia and analgesia, is more effective, and has fewer side effects.Studies on the analgesic effects of esketamine have mainly focused on patients under general anaesthesia, and studies have shown[22-24] that the use of esketamine in general anaesthesia has a better postoperative pain effect and reduces the amount of morphine.But in comparison there are fewer studies on the use of esketamine in cesarean section at home and abroad.A recent study[25] showed that intranasal administration of 28, 56 or 84 mg dextroketamine to 67 patients with refractory depression(TRD) produced a potent and rapid antidepressant effect with a safety profile comparable to that of intravenous 0.5 mg/kg ketamine.It has also been shown[26] that patients with refractory depression receiving intravenous 0.20 mg/kg or 0.40 mg/kg esketamine (over 40 min) had rapid antidepressant effects over 24 hours, demonstrating the rapid antidepressant effect of continuous intravenous esketamine administered over a short period of time.In combination with the above, the intravenous infusion of esketamine (0.20 or 0.40 mg/kg) was chosen to assess and compare its effect on analgesia and postpartum antidepressant effect after cesarean section and to avoid direct fetal effects,.Our trial was designed to be pumped after delivery and umbilical weaning.
The results of our study showed that VAS scores and sufentanil consumption were reduced in the HE and LE compared to C, and were less in the HE, suggesting that intraoperative use of esketamine reduced post-caesarean pain within 24 h and that analgesia was better in the high-dose HE.The reduction of postoperative pain by esketamine is associated with the inhibition of visceral pain sensitization by ketamine[8],: (1) esketamine reduced direct or referred somatic pain caused by NMDA receptor-related injury [9],and activation of C-fiber injury receptors in spinal cord neurons caused a state of NMDA receptor-mediated central hyperexcitability producing injurious pain and nociceptive hyperalgesia.(2) esketamine may reduce peripheral and central visceral NMDA and non-NMDA receptor related injury perception and enhance pain inhibitory systems, such as the monoaminergic system[10].(3) esketamine can have a direct effect on brain areas with pain perception, pain memory or pain inhibition functions[11].As the immediate half-life of intravenous infusion of esketamine is less than 2 hours[12], this may be consistent with the antinociceptive allergic properties of the drug rather than a simple increase in analgesia.Antenatal depression is a risk factor for postnatal depression.Underwood[13] showed that approximately 39% of patients with antenatal depression develop postnatal depression.Therefore, we assessed the EPDS scores of all maternity tested one day before surgery and the results showed no statistically significant differences in EPDS scores between the HE, LE and C one day before surgery, ensuring that the three groups were comparable.EPDS scores were lower in the HE and LE one day and three days postoperatively compared to C.It is suggested that continuous intravenous infusion of esketamine during caesarean section has a rapid antidepressant effect in the short term.The antidepressant mechanism of esketamine is related to selective antagonism of the NMDA receptor subtype containing NMDA receptor subunit 2B (NR2B), which mediates phosphorylation of eukaryotic elongation factor 2 kinase and inhibition of brain-derived neurotrophic factor translation, increased expression of brain-derived neurotrophic factor, and its receptor pro-myosin receptor kinase B is associated with the antidepressant activity of esketamine[18].
The results of this study showed that MAP and HR were higher in the HE and LE compared to C.This was related to the central sympathomimetic effect of esketamine[14], which excites the sympathetic centre and increases endogenous catecholamine release, leading to increased blood pressure and increased heart rate.However, there were no significant differences in haemodynamics between the three groups, suggesting that maternal haemodynamics were less affected by intravenous infusion of 0.20 mg/kg or 0.40 mg/kg esketamine.Some maternity experienced dizziness, nausea and vomiting, diplopia and hallucinations after intraoperative use of esketamine.The incidence of these adverse reactions was higher in the HE and LE groups compared to the C group, but the duration of these adverse reactions was short and the women left the anaesthesia resuscitation unit (PACU) without significant adverse reactions.Ketamine usually causes significant psychiatric symptoms, such as dissociative symptoms and hallucinations, after intravenous administration[15].Compared to ketamine, esketamine has fewer psychiatric side effects and takes less time to disappear, which is consistent with the results we observed.Studies have shown that[16]esketamine has a lower incidence of psychiatric side effects than ketamine, and additional literature has shown that[17] esketamine does not reduce maternal ability to breastfeed or the duration of breastfeeding.Therefore esketamine is more suitable for csarean section than ketamine at the same dose or at a lower dose.
In conclusion, (1) intravenous infusion of esketamine during caesarean section enhances the postoperative intravenous analgesic effect of sufentanil and reduces the dose of opioids, and the analgesic effect of 0.4 mg/kg esketamine is better than that of the 0.2 mg/kg dose group; (2) Intravenous pumping of esketamine during cesarean section improved maternal EPDS scores at 1 day postoperative and 3 days postoperative and was less adverse and better tolerated in the 0.2 mg/kg esketamine dose group; (3) Further observations are needed regarding the effect of intravenous esketamine infusion during caesarean section on long-term postoperative maternal antidepressant.
杂志排行
Journal of Hainan Medical College的其它文章
- Systematic review and meta-analysis of endometrial thickening during endocrine therapy combined with Chinese herbal medicine intervention after breast cancer surgery
- Clinical observation on the efficacy and safety of different doses of alfentanil for painless gastroscopy
- Expression and significance of ADAM12 in bladder cancer
- The expression of TUSC3 in Preeclampsia and the function in trophoblast cell
- Effect of hepatocyte growth factor on inflammatory factors associated with CCL4-induced hepatocyte injury
- Inhibitory effect of water soluble propolis on oxidative damage in rats with ulcerative colitis
