Meta-analysis of the efficacy and safety of extended right liver transplantation versus whole liver transplantation
2023-11-20SUNJiangboPANShenghuiCHENWeijiaXUJian
SUN Jiang-bo, PAN Sheng-hui, CHEN Wei-jia, XU Jian✉
1.Department of Organ Transplantation, the Second Affiliated Hospital of Hainan Medical University, Haikou 570105, China
2.Hainan Organ Transplantion Institute, Haikou 570105, China
Keywords:
ABSTRACT Objective: To compare the differences in postoperative survival and complications between extended right liver transplantation(ERLT) and whole liver transplantation(WLT).Methods:The Chinese and English databases were searched for clinical studies on comparing ERLT with WLT for end-stage liver disease from the date of database construction to April 15,2022.The searched literature was de-duplicated and selected according to the order of title,abstract and content, after which NOS quality evaluation was performed for literature that matched the study.Postoperative complications and survival data were extracted from the eligible literature and subjected to Meta-analysis with Review Manager 5.3, and finally data sensitivity analysis and publication bias tests were performed.Results: The complication of ERLT such as biliary complications[OR=1.77, 95%CI=(1.39, 2.25), P<0.000 01], biliary leakage [OR=2.16, 95%CI=(1.64, 2.84), P<0.000 1], total vascular complications [OR=2.00,95%CI=(1.48, 2.70), P<0.000 1], hepatic arterial thrombosis [OR=2.06, 95%CI=(1.50, 2.83),P<0.000 01], re-Transplantation[OR=1.93, 95%CI=(1.53, 2.45), P<0.000 01] have a higher occurrence rate compared with WLT.While the biliary stenosis [OR=0.74, 95%CI=(0.48, 1.15),P=0.18], hepatic portal vein thrombosis [OR=1.72, 95%CI=(0.84, 3.49), P=0.14] , primary non-function[OR=1.27, 95%CI=(0.80, 2.02), P=0.32] had no statistically difference in the incidence of complications after liver transplantation.In terms of survival, ERLT had lower 1-year graft survival rate [OR=0.64, 95%CI=(0.54, 0.76), P<0.000 01] and patient survival rate[OR=0.75, 95%CI=(0.62, 0.91), P=0.003] than WLT.Fortunately, there was no statistically difference in 5-year graft survival rate[OR=0.97, 95%CI=(0.76, 1.23), P=0.78] and 5-year patient survival rate[OR=0.94, 95%CI=(0.78, 1.14), P=0.54].Conclusion: ERLT is a safe and effective treatment for adult end-stage liver disease.As a surgical method with postoperative complications and survival similar to that of WLT, ERLT can increase the source of donor liver.
1.Introduction
ERLT was originally written by Pichylmayr et al.[1] in 1988, ERLT is widely used in liver transplantation in different countries[2].Whether enlargement of the right hemi-liver can be performed well in adults is still controversial[3].Early studies have shown that ERLT has a higher incidence of postoperative complications and early mortality.However, with the improvement of surgical techniques,some research centers believe that ERLT can achieve the same transplantation effect as Whole liver transplantation[4].
At present, the safety and efficacy of ERLT have not been unanimously recognized.countries widely recommending ERLT,such as Italy and Germany, believe that the benefits far outweigh the disadvantages.the “forced separation” policy in these countries has reduced the mortality rate of children with end-stage liver disease to 0 in recent years[5].On the contrary, countries such as the United States, where the pressure of the donor liver is relatively small compared with other countries, believe that ERLT is a marginal donor liver graft, and it is prone to postoperative complications such as biliary complications (BCs), vascular complications, and re-transplantation (RE-LT), etc.[6].Japan, South Korea and others believe that ERLT is technically as complicated as Living Donor Liver Transplantation, (LDLT) and requires the use of an ideal liver donor from the best donor, and its final prognosis may only be comparable to that of other types of marginal grafts.[7], a more waitand-see attitude towards ERLT or significantly increased criteria for splitting the donated liver.
There are a large number of liver transplants in China.Although the number of ERLs increases year by year, the proportion of ERLs abroad is significantly lower, and the related literature and experience are few[8].Therefore, we conducted a meta-analysis and systematic review of the relevant literature both in China and abroad to assess the safety and effectiveness of the expanded right hemiliver transplantation.
2.Data and methods
2.1 PICOS principles
P(Participant/patient): An adult patient requiring liver transplantation for end-stage liver disease confirmed by CT,pathology, liver function, and clinical signs;
I(Intervention): Extended right hemi-liver transplantation (braindead donor, recipient with extended right hemi-liver);
C(Comparison): Total liver transplantation (brain dead donor,recipient undergoing total liver transplantation);
O(Outcome): To compare the safety and effectiveness of ERLT and WLT in the treatment of end-stage liver disease, such as BCs,vascular complications, and survival rate;
S(Study): Retrospective cohort study, prospective randomized controlled study;
2.2 Inclusion and exclusion criteria
2.2.1Inclusion criteria
(1) The research object is a comparative study on postoperative efficacy and prognosis of ERLT and WLT in patients with end-stage liver failure, with the main focus on adults.
(2)Cases in a single study ≥5;
(3)WLT was used as the control group.
(4)Studies may involve liver transplantation in children, but data must be available for separate analysis in adults with enlarged right hemi-liver.
(5)One of the following outcome measures were included in the study.Outcome measures included: ① 1-year Graft survival, GS)rate and overall survival, OS) rate of patients, and 5-year OS and GS rates.② The incidence of primary non-function, PNF) and re-LT in the transplanted liver; ③BCs (including biliary fistula and biliary stricture); ④ Vascular complications, including Hepatic artery thrombosis (HAT) and PVT (Heptic Venous Thrombus, HVT);
2.2.2Exclusions
(1)The original text was not available in the literature, or Meta required for the meta-analysis could not be extracted;
(2)Non-Chinese and English literature;
(3)Articles with duplicate data were analyzed according to the latest articles;
(4)Case reports or case series studies;
(5)One-arm studies involving ERLT:
2.3 Literature Retrieval
2.3.1 Retrieval strategy
According to the standards for evidence-based medical literature retrieval and Cochrane Handbook system evaluation, prospective randomized controlled or retrospective cohort studies comparing ERLT with WLT in the treatment of end-stage liver disease from database establishment to April 15, 2022 were retrieved according to the pre-established Chinese and English retrieval strategies.The English retrieval databases were PubMed, Web of Science, Cochrane Library, and Embase.The databases retrieved in Chinese were China Biomedical Literature Database, Wanfang, HowNet and VIP.
2.3.2 Literature retrieval words
The English retrieval database mainly uses “translation”,“translation”, “liver”, “hepative”, “split”, “extended right-split”,“right lober grades”, “right extended lobe”, “right extended grave”and “full right” as the search terms.The Chinese search term was“expanded right half liver transplantation, total liver transplantation,brain death donation, split liver transplantation, liver malignant tumor, liver cancer, randomized controlled trial, retrospective case analysis, biliary complications, vascular complications, and patient survival rate”, and the like.The search was performed according to different combinations, and the language was limited to Chinese and English.Meanwhile, relevant references of obtained articles were searched to avoid omissions.
2.4 Evaluation methods
2.4.1 Evaluation indicators
Literature screening and data extraction were conducted independently by two reviewers in the study.In case of disagreement,the third reviewer resolved the disagreement through discussion and negotiation.If studies lacking relevant information were identified,the authors were contacted for raw data, including by e-mail and telephone.Data were extracted using a pre-established data extraction table, including: (1) General information of the included studies, including the name of the author, year of publication,country, and study time; (2) Basic data included in the study: mean age of donor and recipient, gender, sample size, body weight, MELD score, Graft to recipient weight ratio (GRWR), Cold ischemia time (CIT), and cleavage type (in vivo and in vitro) (3) Outcome indicators: main outcome indicators (OS rate at 1 and 5 years, GS rate at 1 and 5 years); Secondary outcome measures: PNF incidence,re-LT incidence, vascular complications (HAT, PVT, hepatic vein),BCs (biliary stricture, biliary fistula).
In statistical analysis, the quantitative analysis results between the ERLT group and the WLT group were expressed by Odds Ratio (OR)and 95% Confidence intervals (CI).Heterogeneity I According to the criteria for quality evaluation of Cochrane Cooperative Network, if P > 0.1 and I<30%, there was mild heterogeneity in the analysis of this index.When P>0.1, And 30%I2<60%, the data had moderate heterogeneity.The fixed-effect model was used for statistical analysis in the cases of the above two items.When P0.1, and I260%, the data had significant heterogeneity.The random effect model was used for statistical analysis in the study, and subgroup analysis was conducted for this indicator to determine the source of heterogeneity.Review Manager 5.3 was used for Meta-data analysis.
Sensitivity analysis and publication bias: Each index in the literature was excluded and included one by one.The change of OR value was observed to determine the stability of the study results and the sensitivity of each individual data.The funnel plot symmetry was used to visually analyze the publication bias.
2.4.2 Literature quality evaluation criteria
The quality of observational studies was assessed using the NOS(Newcastle-Ottawa Scale (NOS) literature quality rating scale).The scale was divided into three parts in total and nine specific rules,including the selection of study subjects, whether the groups were comparable, and the quality of result evaluation (there were detailed evaluation indicators and standards in this study, which the author could provide according to need).The full score was 9, with ≥8 being high quality, ≥6 being medium quality and < 6 being failure.
3.Results
3.1 Search results
3.1.1 Retrieval process and literature data
Through PubMed, Web of Science, Cochrane Library, Embase and other databases, 3,937 English articles that might meet the conditions and 218 Chinese articles that met the topics were retrieved.At the same time, nine articles that met the conditions of the study were obtained through the references of relevant articles, and a total of 4,164 articles were obtained preliminarily through literature retrieval.A total of 1,437 articles were obtained after the repetitive articles were excluded by Endnote 9.0.Then, by reading the titles and abstracts, a total of 245 articles were obtained, including 671 articles that were not related to ERLT due to death donation, 149 reviews, 32 systematic reviews, 266 living donor liver transplants,and 74 articles that did not conform to the format or were incomplete in content, such as letters and SMS.After further reading the full text of the remaining 245 articles, 16 articles with data reuse excluded,25 articles with incomplete original literature information or unable to obtain original materials, and 38 articles with research orientation that was not completely consistent with the theme of this research orientation or did not involve the data indicators required for this study, mainly involving left and right hemi-liver dissection, or the research theme that focused on left lateral lobe liver transplantation,or the research control that focused on the comparative study between adults and children.Finally, among the remaining 21 articles, one article was found to be unqualified in literature quality evaluation during the analysis and was discarded.Finally, all the obtained articles were in English, and the relevant Chinese articles only covered related series of case reports or single-arm studies.No Chinese articles meeting the research criteria were found, and a total of 20 articles were finally obtained.
3.1.2.Literature quality evaluation results

Fig 1 Literature retrieval process diagram
As shown in the figure for literature quality evaluation of included subjects, there were nine articles with high quality evaluation,including three articles with 9 points, six articles with 8 points and the rest 11 articles with medium quality evaluation, including six articles with 7 points and five articles with 6 points.All included literature studies were fully designed and reported follow-up time was sufficient to meet the criteria for evaluating the endpoints of the Meta-analysis.Goals and endpoints were defined in some detail in all relevant included studies.

Tab 1 Literature quality evaluation
3.2 Basic features of literature
All included studies were retrospective cohort studies and all were English articles (no Chinese articles meeting the inclusion criteria).A total of 1304 patients with ERLT and 9070 patients with WLT were included in this Meta-analysis, and the follow-up time was 1–240 months (Table 2).Qualitative analysis of the effect of ERLT on vascular complications and BCs, as well as GS and OS rates at 1 and 5 years, and re-LT and PNF in 20 studies.
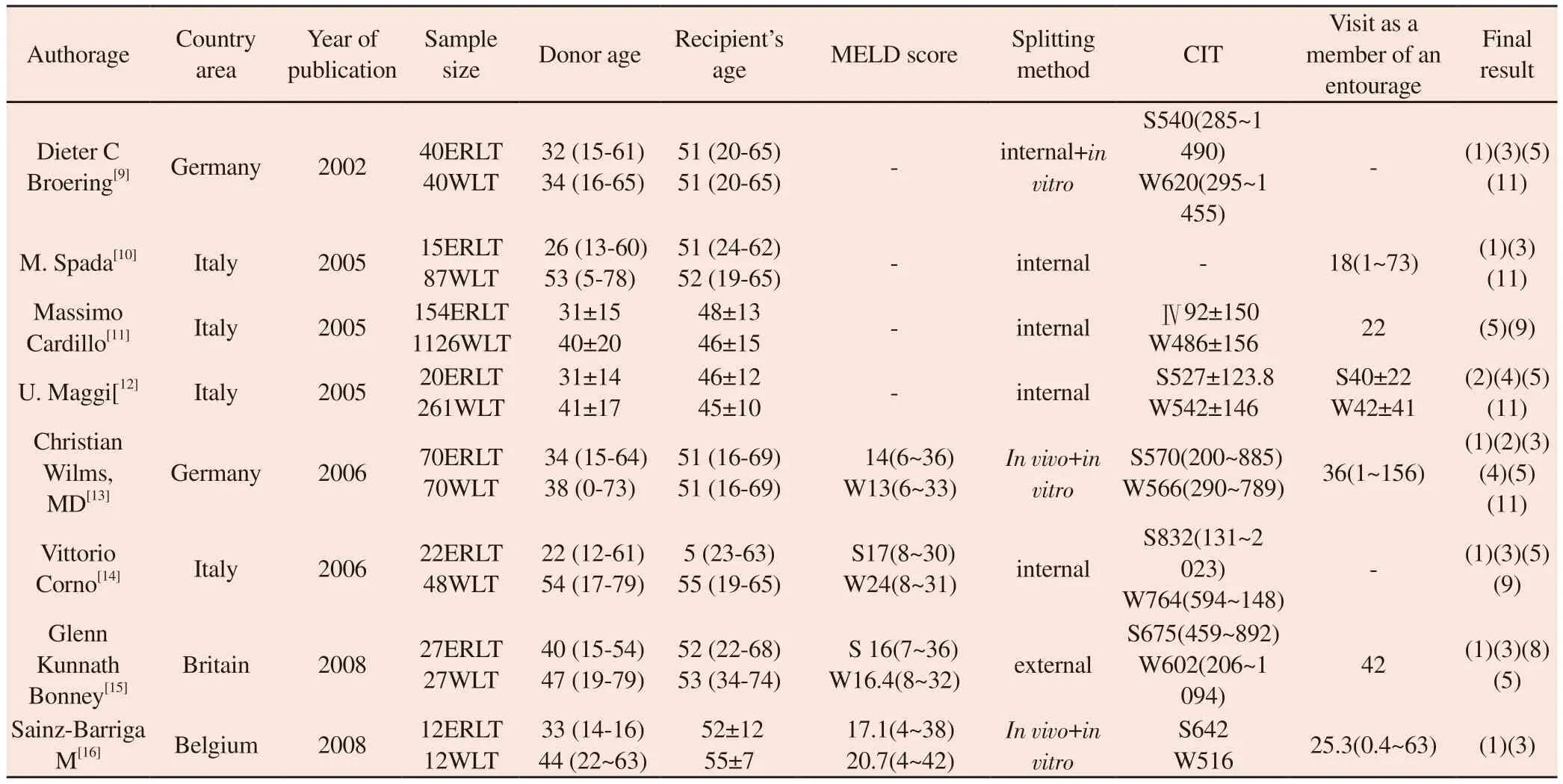
Tab 2 Basic features of literature
Note: * Outcome measures: (1) GS rate in 1 year (2) GS rate in 5 years (3) OS rate in 1 year (4) OS rate in 5 years (5) BCs (6) bile leakage (7) biliary stricture(8) total vascular complications (9)HAT formation (10) PNF (11) RE-LT
3.3 Quantitative analysis of Meta-analysis results
A total of 20 articles were included in this study, 10 studies reported PNF after liver transplantation, and 11 studies reported re-LT after ERLT.Seventeen studies covered the GS rate in one year, 15 studies covered the OS rate in one year after surgery, 10 studies covered the GS rate in five years, and nine studies covered the OS rate in patients after liver transplantation in five years.Twelve studies reported total vascular complications, 13 articles reported postoperative HAT, 6 articles reported PVT, 13 studies reported total BCs incidence, 11 studies reported bile leakage, and 9 studies reported biliary stricture.The following is a detailed analysis of each index.
2.3.1.Biliary Biles complications, (BCs)
According to the search results of a total of 13 articles describing BCs, the fixed-effect model in the meta-analysis for BCs after liver transplantation showed significant difference between the two groups[0R = 1.77; 95% CI=(1.39, 2.25); P < 0.000 01), 702 patients with ERLT, a total of 137 patients with BCs, the incidence of BCs was 19.5%, while the total number of cases with WLT was 2648, 347 patients with BCs, accounting for 13.1%.The incidence of biliary BCs was higher in the ERLT group than in the WLT group.There was no significant heterogeneity between the two groups of articles and no publication bias [(P = 0.57); I² = 0%].
3.3.2 Biliary leakage
According to the search results of a total of 11 articles describing bile leakage after liver transplantation, the fixed-effect model analysis in the meta-analysis showed that there was a significant difference between the two groups in bile leakage after liver transplantation [OR=2.16; 95%CI=(1.64, 2.84); P <0.000 1], and the incidence rate of bile leakage was 20.5% (106/516) in ERLT (Note:the articles reporting bile leakage here are not completely consistent with the total complication of biliary tract, so it is possible that the incidence rate of bile leakage is greater than the total complication rate of biliary tract).In contrast, 249 cases (11%) of WLT 2258 patients have bile leakage, and there is no significant heterogeneity in the data of various articles [P = 0.65; I2= 0%], the incidence of bile leakage in the ERLT group was higher than that in the WLT group.

Fig 2 Forest map of biliary complications

Fig 3 Forest map of bile leakage incidence
3.3.3 Biliary tract stenosis
According to the search results reported in nine articles concerning biliary stricture, the fixed-effect model in meta-analysis was used to analyze the postoperative biliary stricture of ERLT and WLT, and no significant difference was found between the two [OR = 0.74;95% CI=(0.48, 1.15); P=0.18], of which, 428 cases were reported in ERLT regarding biliary stricture, of which 28 cases (6.5%) occurred stenosis, while 2084 cases (9.3%) were reported in WLT regarding biliary stricture, and 193 cases (9.3%) developed biliary stricture.There was no significant heterogeneity between the two groups [P =0.65; I² = 0%].There was no significant difference in the incidence of biliary strictures between the ERLT group and the WLT group.
3.3.4 Vascular complications
According to the search results, a total of 12 articles reported the vascular complications in both groups after operation.The fixedeffect model analysis according to the meta-analysis showed that there was a significant difference in vascular complications between the ERLT and WLT groups [OR = 2.00; 95% CI=(1.48, 2.70); P <0.000 1), a total of 646 subjects were included in this study, while 80 subjects (12.4%) experienced vascular complications from ERLT,2,446 subjects (WLT), and 216 subjects (8.8%) experienced vascular complications, with no significant heterogeneity between the two groups of data (P = 0.88; I2= 0%), and a higher incidence of total vascular complications in ERLT than in WLT.
3.3.5 Arterial thrombosis (HAT)
Postoperative HAT was reported in a total of 13 articles according to the search results.The fixed-effect model was used to compare the HAT status, and the result showed that there was a significant difference between the two groups [OR = 2.06; 95%CI=(1.50,2.83); P < 0.000 01), the total number of cases of ERLT was 890,and HAT formation was 7.8%, while the number of cases of WLT was 3,591, including 169 cases of hepatic artery formation, and the incidence rate of complications was 4.7%.There was no significant heterogeneity between the two groups [(P = 0.85); I2= 0%], the incidence of HAT in ERLT was higher than that of WLT.
3.3.6 Portal vein thrombosis (PVT)
PVT after liver transplantation was reported in a total of six articles according to the retrieved results, and fixed-effect model analysis showed that there was no significant difference in PVT between the two groups [OR = 1.72; 95% CI=(0.84, 3.49); P=0.14], and the number of patients with ERLT was 410, including 10 cases of PVT,with the incidence rate of 2.4%, while the number of subjects with WLT in the literature was 2078, including a total of 30 cases of portal vein thrombosis, with the incidence rate of 1.4%, and there was no significant heterogeneity in the data of each literature [P= 0.52; I2= 0%], and there was no significant difference in PVT incidence between ERLT and WLT.

Fig 4 Forest map of biliary stricture

Fig 5 Forest map of vascular complications

Fig 6 Forest map of arterial thrombosis
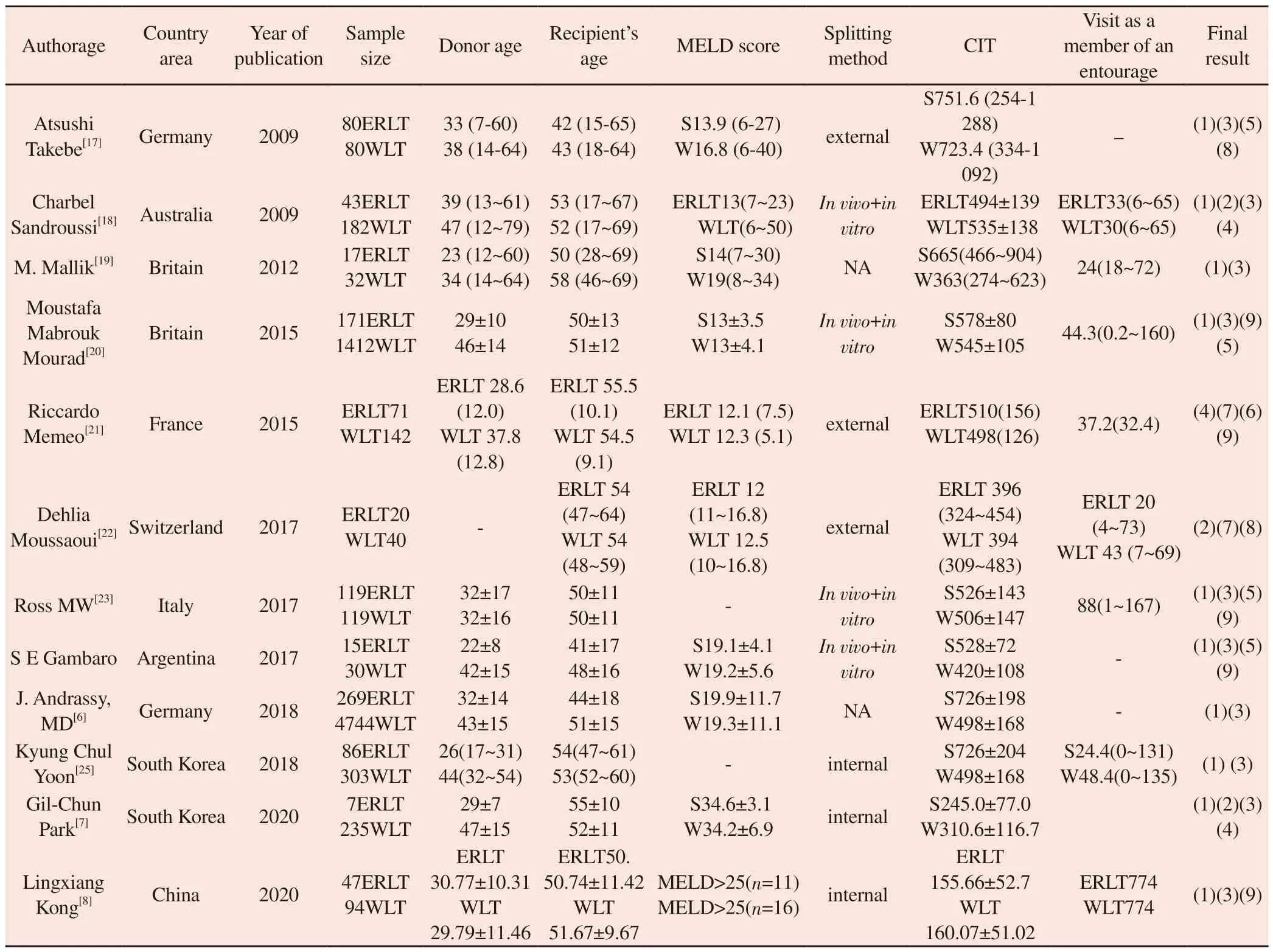
3.3.7 Primary nonfunction of transplanted liver (PNF)
According to the search results, there were 10 literature studies covering the PNF after liver transplantation, and the fixed-effect model analysis of the results of 10 studies showed that there was no significant difference in the incidence of PNF after liver transplantation between ERLT and WLT [OR=1.27; 95% CI=(0.80,2.02); P=0.32], a total of 722 cases in the ERLT group and 2,168 cases in the WLT group were involved in this study.Among them,the incidence rate of PNF in ERLT is 4%, while that in WLT is 3.8%,and no significant heterogeneity is observed in the heterogeneity test(P = 0.57; I² = 0%).The incidence of PNF was higher in the ERLT group than in the WLT group.

Fig 7 Forest map of portal vein thrombosis
3.3.8 Re-transplantation (Re-LT)
According to the search results of a total of 10 articles covering the re-LT after liver transplantation in the two groups, a fixed-effect model was used to compare the occurrence of re-LT of ERLT and WLT, and there was a significant difference in the incidence of re-LT between the two groups after liver transplantation [OR = 1.93; 95%CI=(1.53, 2.45); P < 0.000 01), the total number of cases of ERLT studied involving indicators of re-LT was 884, the number of cases of re-LT was 117, and the incidence rate of re-LT was 13.2%, while the total number of cases of WLT was 7049, the number of cases of re-LT was 619, and the incidence rate of re-LT was 8.8%.The incidence rate of re-LT after ERLT was higher than that of WLT, and the degree of heterogeneity was (P= 0.19; I2= 27%), heterogeneity< 30%, was mild heterogeneity, and the incidence of re-LT postsurgery was higher in the ERLT group than in the WLT group.
3.3.9 GS and OS rates 1 year after liver transplantation
According to the search results, a total of 17 literature studies have reported the GS rate in one year after liver transplantation, and the fixed-effect model in the meta-analysis showed significant difference between the two groups [OR = 0.64; 95%CI=(0.54, 0.76); P < 0.000 01), with a 1-year GS rate of 76.9% in ERLT and 81.9% in WLT (P= 0.351; I2= 9%), and GS rates in subjects with ERLT were lower than those with WLT 1 year after surgery.Among the retrieved results, 15 literature studies reported the OS rate in one year after liver transplantation, and the fixed-effect model in the meta-analysis was used to analyze the Meta.The results showed that there was a significant difference between the OS rate in one year after ERLT and that after WLT [OR = 0.75; 95%CI=(0.62, 0.91); P=0.003], with little heterogeneity between articles (P= 0.43; I2= 2%), in which the one-year OS rate of ERLT was 81.4%, while the OS rate of WLT was 83.1%, and the GS rate and OS rate in the ERLT group at one year after surgery were higher than those in the WLT group.
3.3.10 GS and OS rates 5 years after liver transplantation
A total of 10 articles covered the GS rate in 5 years after ERLT and the fixed-effect model analysis in the meta-analysis showed no significant difference in GS rate in 5 years between the two groups[OR = 0.97; 95% CI=(0.76, 1.23); P=0.78], literature heterogeneity is small (P = 0.23; I2= 24%), in which the GS rate was 71.3% in the 5-year post-ERLT group and 72.5% in the 5-year post-WLT group,and there was no significant difference between the GS rate and WLT group in the 5-year post-ERLT group.Among the nine articles reporting the OS rate in five years after liver transplantation, the meta-analysis fixed-effect model showed no significant difference in OS rate in five years between the two groups [OR = 0.94;95%CI=(0.78, 1.14); P=0.54], while there was mild heterogeneity between the literature data (P= 0.23; I2= 24%), with a 5-year OS rate of 76.3% for ERLT and 74.7% for WLT.In summary, there were no significant differences in OS and GS rates between ERLT and WLT at 5 years.
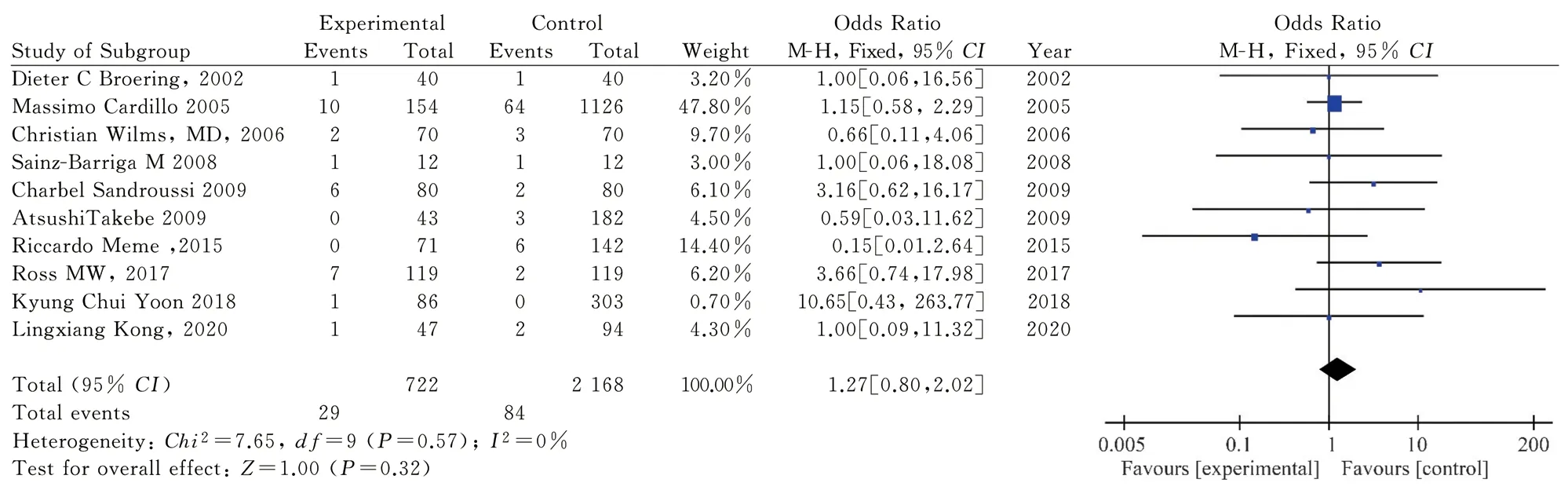
Fig 8 Primary nonfunctioning forest map of transplanted liver

Fig 9 Forest map of incidence rate of liver retransplantation

Fig 10 Forest map of GS rate and OS rate at 1 year after liver transplantation
3.4 Sensitivity analysis and publication bias of literature study
All literature results included in this study were subjected to sensitivity analysis and publication bias test.Among them, except for the incidence of re-LT and OS in 5 years, one study showed higher sensitivity compared with other studies, but it did not significantly affect the stability and reliability of the overall data.All literature data were subjected to publication bias test and no significant publication bias was found (as shown in Fig.12 in the funnel plot, P> 0.05 in all analyses).

Fig 11 Forest map of GS rate and OS rate 5 years after liver transplantation

Fig 12 Publication bias funnel plot
4.Discussion
The results of this meta-analysis show that the incidence rate of BCs after ERLT is significantly different from that of WLT.The results of this meta-analysis show that the incidence rate of bile leakage after ERLT is higher than that of WLT.The incidence rate of BCs after ERLT is as high as 19.5%, which is significantly higher than that of BCs13.1% of WLT.In addition, the incidence rate of BCs has been reported in the early literature to be higher.In recent years, with the improvement of surgical technology, more and more transplantation centers tend to split apart in the body, and the incidence rate of BCs after surgery is all obviously lower than before[16, 24].With the improvement of surgical techniques and the development of endoscopic techniques, the cross-sectional BCs of the recipient and complications such as biliary leakage at the biliary anastomosis gradually decrease the impact on the recipient of ERLT[26].
The obvious increase of BCs in ERLT can be attributed to the following three reasons: 1.The different diameters during ERLT insertion make the anastomosis more technically demanding(especially when the main artery and biliary tract are left to the left lateral lobe); 2.The microvascular damage supplying the biliary tract is more serious due to the process of cleaving and liver repair.[17]; 3.Patients with ERLT are prone to bile leakage in cross section[20].Although there are certain risk factors for biliary stricture in ERLT, the incidence of biliary stricture did not increase significantly between the two groups, which may be related to the higher proportion of biliary-enteric anastomosis in ERLT than in WLT[27], Roux-en-Y can protect the biliary tract by providing more blood supply, thus significantly reducing the occurrence of biliary ischemia[28].ERLT injures more blood vessels during separation, so special care should be taken to protect the tissue in the right area of hepatic hilus during cleaving and transplantation, which may greatly reduce the occurrence of biliary ischemic stenosis.The placement of a T-tube can significantly reduce cross-sectional biliary leakage in ERLT, a study that has been confirmed by many transplant centers[29].Research shows that preventive biliary stent implantation can not only reduce the occurrence of bile leakage, but also reduce the occurrence of biliary stricture, and at the same time reduce the inconvenience caused by T tube after surgery for patients[7].
The total vascular complication rate in ERLT is slightly higher than that in WLT, which may be related to arterial reconstruction.Reconstruction of the right hepatic artery increased the risk of thrombosis.In ERLT, the right hepatic artery of the donor and the caliber of the common hepatic artery of the recipient needed to be anastomosed, and the application of bridging vessels for grafting between the two was more frequent.When the right liver supplied multiple hepatic arteries, the incidence of early HAT increased by 20% compared with other arterial reconstruction groups.[20].Therefore, the allocation of the main vascular trunk to the enlarged right hemi-liver should be determined based on the arterial anatomy of the donor and recipient, the number of branches, the size of the branches, the origin of the S4 segment artery, and so on[5].Vascular complications may be closely related to other complications.Vascular complications may lead to worse early survival rate.Acute HAT leads to early graft liver failure and is a key factor for reducing GS rate and OS rate.Vascular complications can interact with BCs.HAT may further increase the occurrence of BCs by causing ischemic biliary lesions.For example, a study by Mabrouk Mourad et al.in the UK found that when arterial reconstruction involved the right hepatic artery (type Ⅱ and Ⅲ) and combined with end-to-end biliary anastomosis, the incidence of BCs was significantly higher in the WLT group (P= 0.04 and P=0.01).[20].The portal vein is assigned to adult subjects and generally does not require reconstruction, so there is no difference in PVT between ERLT and WLT.
Our results show that there were no significant differences in our patient’s postoperative PNF between the two groups, but there was a higher incidence of re-LT in the ERLT group.Currently, the screening criteria for ERLT are relatively strict.The donors of ERLT are younger and more hemodynamic stable.Most of the donors are in the 20-40 years old age group[3].The inconsistent definitions of PNF among different articles are also an important reason for this result.A higher incidence of PNF and re-LT does not necessarily imply a worse patient survival, and in the case of ERLT, subjects tend to have better systemic conditions and a relatively lower MELD score and are therefore better placed to accept re-LT[30].In a recent European transplant analysis of 5013 transplant cases, donor and recipient matches were best matched, and there was no difference in OS rates and the incidence of re-LT between the ERLT and WLT groups[31].Studies have found that the one-year survival rate and the incidence of re-LT are different between the two groups.an indepth study of the literature has revealed that the early recurrence rate of primary diseases (hepatitis c and hepatocellular carcinoma)after ERLT is higher[28], better basic conditions of the subjects, and a higher proportion of liver disease types such as liver cancer may be the main reason for the high incidence of re-LT[32].Therefore,optimal donor-recipient matching is a key issue in maximizing the value of SLT.
GS rate and OS rate in the first year after ERLT are significantly different from those of WLT.The OS rate and GS rate in the first year after ERLT are higher than those of WLT, while there is no significant difference in GS and OS between ERLT and WLT in the fifth year after surgery.Studies have found that the early postoperative survival rate of ERLT is lower than that of WLT.Studies have shown that the re-LT rate of ERLT at three months after surgery may be more significantly different from that of WLT[8].However, as there were few reports regarding early survival such as GS and OS at 3 months after surgery, no further Meta-analysis was conducted for earlier survival in this meta-analysis.At present, it is considered that the main factors affecting re-LT after ERLT surgery are vascular reconstruction, ischemic biliary stricture, formation of HAT, and prolongation of CIT due to primary recurrence.CIT affected the transplanted liver and the patient’s survival only in the first year after ERLT and even earlier, after which ischemiareperfusion injury and CIT had no further effect on the transplanted liver[3], which may be an important reason for the increased 1-year survival rate after WLT compared with that of ERLT.Although that early prognosi of ERLT is slightly worse than WLT[33]However,the survival rate can reach the same level as that of WLT after technical optimization such as late learning curve, allocation policy,improvement of application to hepatic artery reconstruction and mechanical perfusion[31,34].
In recent years, ERLT has made significant progress in technology.Judging from the results of the Meta-analysis, the prognosis of ERLT is not only related to the quality of the donor liver, but the optimal donor-receptor matching is also crucial[35].Therefore, to play the role of SLT in patients with end-stage liver disease requires the targeted use of ERLT, which not only sets donor criteria, but also strengthens research on organ allocation and donor selection in ERLT[21], and establish a postoperative risk prediction model of ERLT that includes liver donation (such as donor age, CIT, fatty liver disease and other factors) as much as possible, in order to better exert the potential of SLT.
At present, the splitting criteria and allocation principles do not form the same standard.It is better to formulate specific policies in this regard to further regulate the application of SLT.For countries in China that rely on body donation for liver transplantation, ERLT may have greater potential[36].In conclusion, SLT effectively expands the donor source, which is of great significance for pediatric subjects, while the remaining enlarged right lobe may provide a good prognosis for patients with cirrhosis or hepatocellular carcinoma with low MELD scores[28].Therefore, we should further improve the use of ERLT while ensuring the safety of the subjects.
Limitations and shortcomings of this study: 1.The liver diseases among the subjects were not of the same type, and there were differences in results between the two types of liver cancer and liver cirrhosis.The two types of liver diseases were not classified in the current literature, which affected the heterogeneity of the Meta-analysis.2.The postoperative survival rate in this metaanalysis study is different from the officially reported GS rate 1 year after liver transplantation, and more randomized controlled or larger sample size literature Meta should be further included for comparative analysis.3.although more stringent screening criteria have been adopted in this study, factors affecting the prognosis of ERLT include the quality of transplanted liver, the condition of the recipient, allocation strategy, and vascular reconstruction.currently, most of the studies are hybrid in vivo and in vitro cleavage studies[37], this study was unable to analyze the effects of different cleavage types and CIT on ERLT.
Author’s contribution
First author: SUN Jiang-bo (collecting relevant literature and writing papers); Author of communication: XU Jian (in charge of article conception and review); The rest of the authors participated in article retouching and format correction.
There is no conflict of interest.
杂志排行
Journal of Hainan Medical College的其它文章
- Advances in cellular and molecular mechanisms of oral submucosal fibrosis
- Research progress of natural products in treating polycystic ovary syndrome
- Research progress of related signal pathways in the prevention and treatment of heart failure with traditional Chinese medicine
- Network pharmacology and preliminary cell screening studies on the anti-liver cancer activity of Nauclea Officinalis
- Quality of life of hospitalized patients after lung cancer operation and analysis of influencing factors
- Clinical study of different modes of repetitive transcranial magnetic stimulation in the treatment of post‑stroke executive dysfunction
