Neutrophilic Panniculitis Associated With Myelodysplastic Syndrome/Myeloproliferative Neoplasm: A Case Report and Literature Review
2023-10-20AlexaCohenLauraGleasonSafiyyahBhattiNedaNikbakht
Alexa J.Cohen, Laura K.Gleason, Safiyyah A.Bhatti,2, Neda Nikbakht,*
1 Department of Dermatology and Cutaneous Biology, Thomas Jefferson University, Philadelphia, PA 19107, USA; 2 Department of Hematology & Oncology, Thomas Jefferson University, Philadelphia, PA 19107, USA.
Abstract
Keywords: neutrophilic panniculitis, myelodysplastic syndrome, neutrophilic dermatoses
Introduction
Neutrophilic dermatoses (NDs) are a class of inflammatory skin disorders characterized by neutrophil-predominant infiltrative skin lesions without evidence of an infectious etiology or vasculitis.1Examples of NDs include Sweet syndrome (acute febrile ND), pyoderma gangrenosum, subcorneal pustular dermatosis (Sneddon-Wilkinson disease), and neutrophilic panniculitis (NP).NP is a rare subtype of ND that is defined by the presence of a neutrophilic infiltrate in the fat lobules of the subcutis.2Furthermore, NP has been found to be associated with myelodysplastic syndrome (MDS).2-7We herein report a case of NP associated with MDS/myeloproliferative neoplasm overlap syndrome (MDS/MPN) and provide a review of the literature focused on the diagnosis and treatment of NP associated with MDS and MDS/MPN.
Case report
A 65-year-old African-American woman presented with a 1-week history of painful, pruritic nodules on the upper and lower extremities refractory to doxycycline.Her medical history was significant for newly diagnosed MDS/MPN established 3 months priorviabone marrow biopsy after her admission to the hospital with fatigue, exercise intolerance, weight loss, night sweats, and leukocytosis.Bone marrow biopsy was notable for a hypercellular bone marrow with myeloid proliferation, megakaryocytic atypia,4% to 5% increase in blasts, and mild diffuse reticulin fibrosis with pathogenic mutations inBCOR1,PPM1D,andDNMT3A.Fluorescencein situhybridization of the bone marrow revealed trisomy 8; the results were negative forBCR/ABL1translocation and for 5q/5, 7q7, 13q,and 20q deletions.The karyotype of the bone marrow also revealed trisomy 8.These findings were consistent with the diagnosis of MDS/MPN, the unclassified subtype, based on the World Health Organization criteria.8At the time of presentation to the dermatology clinic, the patient had not yet started a chemotherapy regimen.Other than fatigue and exercise intolerance on presentation, she denied any other systemic symptoms including fever or chills.
On examination, the patient had multiple subcutaneous 2- to 3-cm skin-colored nodules on the bilateral lower extremities and the right upper and lower arm (Fig.1A).The lesions were tender on palpation.A complete blood count revealed normocytic anemia (hemoglobin, 7.0 g/dL; mean corpuscular volume, 98 fL), polymorphonuclear leukocytosis (white blood cell count of 17.2 billion/liter [B/L]; differential count of 84% neutrophils, 4%metamyelocytes, and 2% myelocytes; and absolute neutrophil count of 27%), and thrombocytopenia (platelet count, 142 B/L).The peripheral blood smear revealed neutrophilic leukocytosis with a mild left shift (<10%),occasional blasts, and granulocytic dysplasia.In addition,inflammatory markers were elevated for lactate dehydrogenase (272 IU/L; reference range, 125-240 IU/L), fibrinogen (562 mg/dL; reference range, 200-393 mg/dL), ferritin(2,588 ng/mL; reference range, 30-400 ng/mL), C-reactive protein (19.82 mg/dL; reference range, ≤0.80 mg/dL), and the erythrocyte sedimentation rate (35 mm/h; reference range, 0-30 mm/h).Based on these findings, the patient had a high score of 5.5 using the Revised International Prognostic Scoring System for Myelodysplastic Syndromes Risk Assessment Calculation, which is a scale system from 1.5-6.0, and a high score of 5.5 indicates that the MDS is likely to progress more quickly or become AML more quickly without treatment and that it may cause more symptoms and health complications in a short amount of time, thus requiring more intensive treatment.9
Punch biopsy of a representative lesion was obtained and sent for tissue culture and histologic examination.Histopathologic examination revealed a mild perivascular inflammatory infiltrate in the dermis and a predominantly lobular infiltrate of polymorphonuclear cells with sparse histiocytes in the subcutaneous fat, fat necrosis, and fragmentation of the fat lobules with no evidence of vasculitis(Fig.1B-1D).Myeloperoxidase was highly expressed in neutrophils in the subcutaneous fat (Fig.1E and 1F).Acid-fast bacilli and Gram stains were negative for bacteria, and tissue culture grew no organisms.The final diagnosis was NP.
After establishment of the diagnosis, the patient was treated with oral prednisone starting at 40 mg/d with reduction by 10 mg every 4 days for a total of 16 days.The patient’s lesions dramatically improved within the following week.At the 1-month follow-up, the initial lesions on her lower extremities and right arm were resolved.However, the patient reported an eruption of small nodules on her left thigh and arm with no systemic symptoms.Prednisone therapy was reinitiated (20 mg/d× 4 days, followed by 10 mg/d × 2 months), leading to resolution of the lesions.

Figure 1.Clinical presentation and histopathological results of the patient with neutrophilic panniculitis associated with myelodysplastic syndrome/myeloproliferative neoplasm.(A) Skin-colored nodule on the left lower extremity.(B-D) Images show a lobular distribution (H&E, B: ×10;C: × 40) and intense neutrophilic infiltration (H&E, B: ×10; D: ×100).(E and F) Myeloperoxidase was highly expressed in neutrophils in the subcutaneous fat (E: × 10; F: × 40).
The patient eventually underwent treatment for MDS/MPN with decitabine, which led to stable peripheral blasts at 4% to 5%.Following this treatment, her clinical course was complicated by severe thrombocytopenia(platelet count of 12 B/L).Unfortunately, she developed multicompartmental and intraventricular hemorrhage extending into the third and fourth ventricles, ultimately leading to death.
在我们看来,弗雷格的做法是让语言上的特征“不定”以一种相对间接的形式在起作用,即通过概念的中介关联至不确定的对象。但是日常语言的表达意向总是意图直接与最终的对象发生关系。因此对问题的解答仍然必须回到对象之上。如果说“四足动物”或“一个四足动物”这些表达尚可以被看作命名不确定之四足动物的通名,但带有空位的表达“( )是一个四足动物”,即严格的概念词,却绝无法被用来命名,只能说,这个表达适用于不确定的四足动物,可以用来谈论任意一个不确定的四足动物。概念词的本质功能不在于“命名”或“代表”一个确定概念,而在于“述谓”一类对象中的任意一个。
Patient consent declaration
Written informed consent of this case publication was obtained from the patients next of kin, which was her daughter, considering patients premortem preferences.
Discussion
NDs are a diverse group of disorders characterized by an abundant infiltrate of neutrophils within the skin in the absence of infection or true vasculitis.NP is an uncommon type of ND that usually presents as deep inflammatory nodules and/or plaques located predominantly on the lower extremities and can be associated with recurrent fevers,arthralgia, and myalgia.1Skin biopsy often reveals a predominantly neutrophilic infiltrate in the hypodermis and fat lobules highlighted by myeloperoxidase expression.1In our patient, the predominant pathology was infiltration of neutrophils in the fat lobules, causing panniculitis; this differs from the dermal infiltrate of neutrophils seen in Sweet syndrome, another ND subtype.1It is important to rule out an infectious etiology in patients with any neutrophilic inflammatory infiltrates to avoid corticosteroid treatment in patients with infection.An infectious etiology was ruled out in our patient because of the absence of organisms in tissue culture and Gram staining.NP can also be caused by certain drugs, including vemurafenib, BRAF inhibitors,and other kinase inhibitors such as dasatinib10; however,our patient had not received any of these agents prior to the diagnosis of NP.
Although rare, NP can occur in conjunction with MDS.Some studies have suggested that NP can be the result of aggravation of MDS and treatment of MDS.2-3A thorough patient history should be taken to elicit details that may raise suspicion for consequences or complications of malignancy, including constitutional symptoms such as fever, weight loss, lymphadenopathy, and fatigue.In addition, laboratory examinations should be conducted to identify elevations in any markers of inflammation, including the erythrocyte sedimentation rate, C-reactive protein,and acute phase reactants.Other laboratory studies should include a complete blood count, anti-nuclear antibody titer,and measurement of the rheumatoid factor concentration to exclude hematological malignancies and vasculitis.
Only 8 cases of NP associated with MDS, including our patient, have been described in the literature to date(Table 1).The patients’ ages ranged from 13 to 74 years(median, 58 years).Most patients were male (6/8), and most received a diagnosis of MDS before a diagnosis of NP (6/8).The clinical presentation was variable but typically involved multiple widespread erythematous nodules on the extremities.Multiple types of medications were used for treatment, including anti-inflammatory medications such as colchicine and dapsone, a variety of antibiotics, and systemic steroids.Most patients had no improvement with anti-inflammatory medications and antibiotics but achieved resolution with systemic steroids.These data suggest that once a diagnosis of NP is established and infection is ruled out, anti-inflammatory medication and antibiotics may be discontinued because they are ineffective in the treatment of NP.All patients treated with steroids achieved resolution of their cutaneous lesions, including our patient.This supports the use of systemic steroids as first-line therapy for NP.
The limitation of our case is that the pathogenesis of NP in association with MDS is rare and not well understood.The present case further supports NP as an ND associated with MDS.In a patient diagnosed with MDS who develops lobular NP, NP must be considered after infection is ruled out.In rare instances when NP is diagnosed first, a thorough examination for a hematological disorder needs to be completed because a skin manifestation may be the first sign of a malignancy.Once diagnosed, NP is easily treated and has an excellent response to systemic corticosteroids.In addition, because NP can be a manifestation of myeloid neoplasms, treatment of the primary myeloid disorder might also result in improvement or resolution of the NP.Overall, dermatologists can benefit from implementing a bidirectional approach when encountering patients with NP or MDS.If NP is diagnosed, MDS with or without MPN must be considered,whereas in a patient with MDS, NP should be a differential diagnosis of clinically suspicious skin lesions.
Source of funding
This work was supported by a grant from the National Cancer Institute (R03CA252818 to NN).
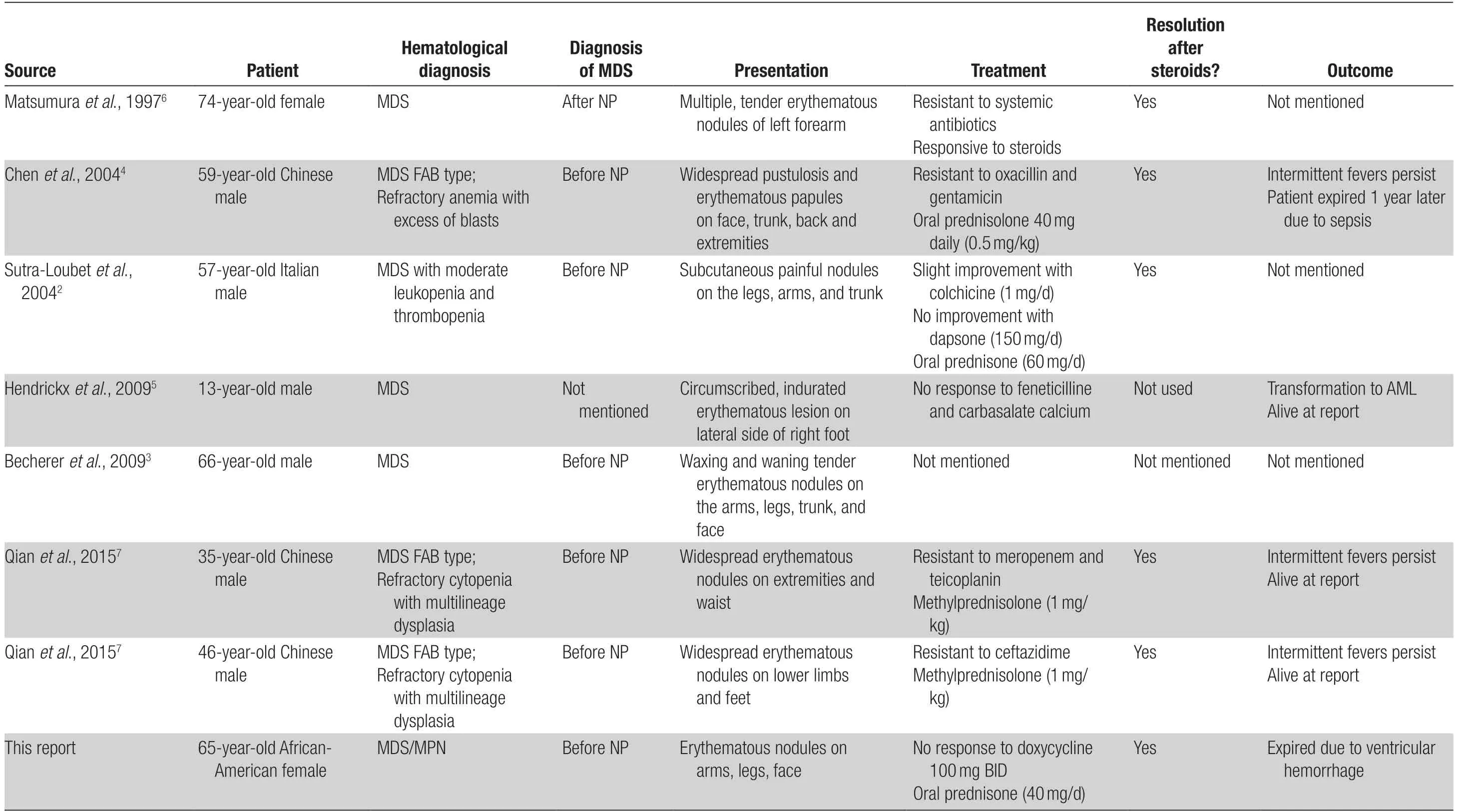
Table 1 Cases of neutrophilic panniculitis associated with myelodysplastic syndrome reported in the literature.
猜你喜欢
杂志排行
国际皮肤性病学杂志的其它文章
- Transcription and Secretion of lnterleukin-1β and HMGB1 in Keratinocytes Exposed to Stimulations Mimicking Common lnflammatory Damages
- Dermoscopic Assessment of Pityriasis Versicolor: A Cross-Sectional Observational Study
- Evaluation of Serum Vitamin D Concentration and Blood Eosinophil and Basophil Counts in Patients With Vitiligo: A Cross-sectional Study From Rafsanjan and Zarand, Iran
- Teledermatology During the COVID-19 Pandemic in a Developing Country: Could This Be the Answer to Improving the Reach of Dermatology Care?
- Basal Cell Carcinoma Excision Guided by Dermoscopy: A Retrospective Study in Macau
- The Role of Endoplasmic Reticulum Stress in Melanoma
