Teledermatology During the COVID-19 Pandemic in a Developing Country: Could This Be the Answer to Improving the Reach of Dermatology Care?
2023-10-20ShakiratGoldOlufadiDamilolaJesuyajoluOlufolakemiColeAdeifeDidiEmokpareOmololuEnigbokan
Shakirat Gold-Olufadi*, Damilola Jesuyajolu, Olufolakemi Cole-Adeife, Didi Emokpare,Omololu Enigbokan
1 Department of Medicine, University College Hospital, Ibadan, Oyo state 200212, Nigeria; 2 Salford Royal NHS Foundation Trust,Northern Care Alliance NHS Foundation Trust, Manchester M68HD, United Kingdom; 3 Lagos State University Teaching Hospital,Lagos State 100271, Nigeria; 4 Outpost Healthcare, Saskatchewan S4P 0J3, Canada.
Abstract
Keywords: teledermatology, COVID-19, telehealth, acne, black skin
Introduction
Telemedicine refers to the process by which healthcare consumers are provided healthcare services by their providers using information and communication technology as a means of communication without a physical meeting.1This service is frequently employed for healthcare provision in developed countries, especially for highly communicable diseases and for specialties where healthcare providers are limited.2However, the COVID-19 pandemic has changed the face of telemedicine even in developing countries.3The pandemic was accompanied by lockdowns and curfews worldwide, with restrictions on physical consultation and increased adoption of virtual consultation in both developed and developing countries.4Dermatology, being a visual specialty, is one in which telehealth has been of great benefit in developed countries,5and it may be even more important in developing countries where the ratio of dermatologists to patients is extremely low.6
In Nigeria, the number of fully trained dermatologists is less than 250 in a population of more than 170 million people, resulting in a ratio of 1 dermatologist to 850,000 Nigerians.Most dermatologists are in urban areas, and many patients must travel interstate to see a dermatologist.The adoption and use of telemedicine was low in previous studies because of factors such as poor Internet availability, unwillingness to pay for the service,low data safety, and an inadequate number of healthcare providers using the services, among other factors.6The COVID-19 pandemic and technological improvements have resulted in the availability of several platforms with inbuilt electronic medical records and video units.Healthcare providers and consumers can sign up, pay for consultation, and receive prescribed treatment.About 15 such platforms are currently available in Nigeria, allowing patients to book both physical and virtual consultations.The methods employed in consultations include store-and-forward, real-time, or hybrid consultations.7Although concerns have been expressed regarding the use of WhatsApp for store-and-forward consultations,8the data are usually encrypted to ensure safety.This article highlights the use of teledermatology (TD) by 2 dermatologists in Nigeria on 2 of these platforms and factors that influenced the use of TD services during a 1-year period during the pandemic.
Materials and methods
Subjects
This retrospective study involved all patients that had booked an appointment (whether virtual or physical)with dermatologists on 2 telemedicine platforms during a period of 1 year (April 2021 to March 2022).Inclusion criteria for this study was patients who booked appointments physically or virtually over the one-year period and consented to participate, and exclusion criteria was patients who did not turn up for appointments.The dermatologists were primarily based in Ibadan, Oyo state (the largest city in West Africa) and Lagos state (the commercial hub of Nigeria).The platforms used had an inbuilt video app and electronic medical record that could be used for virtual consultation and allowed patients to fill out a form containing their history and pictures, which could be sent ahead of the consultation.Both platforms ensured data security and protection.The teleconsultation was performed either through a store-and-forward method using WhatsApp or a real-time video consultation.Healthcare providers could set up their calendars for consultation at the beginning of each month, and a personalized link was generated on the platform and could be sent to patients who wanted to book an appointment with the healthcare provider.The appointment was usually confirmed after the patient had paid for the consultation through the platform.For video consultations, because the dermatologists were usually aware of the booking, we ensured that we had a fast Internet connection before the consultation and that we were in the office while seeing the patients to give the feel of a physical consultation and to ensure confidentiality.The patients were also encouraged to secure good Internet service prior to the consultation and be in a location where they could adequately expose the affected areas of the skin.The 2 platforms also had options allowing them to upload their pictures and history ahead of the consultation,which helped in cases of poor network connections.When Internet issues were unavoidable, the patients were taught how to take pictures in natural light, and they sent pictures to the dermatologists’ email address after the consultation for further correspondence with the dermatologists.
An online questionnaire was emailed to all patients who had been seen by the dermatologists during the study period after informed consent was obtained via email and a follow-up call.The questionnaire followed the guidelines specified in the report on standards and guidelines in telemedicine.9
Ethical approval was granted by the Oyo State ethics reviewboard (Approval ID: AD/13/479/4425A) and was performed in adherence to the Helsinki declaration.The written informed consent was provided by all of the subjects.
Data collection methods
The questionnaire was prepared by the authors of this paper who are all medical doctors of which two are dermatologists.The questionnaire was made using Google forms and was on a single page which was sent as a link to the respondents.The respondents filled out the forms and the data was automatically entered into a secure Microsoft excel sheet.
Instrument
The questionnaire had 34 questions which were single-answer options and in nine of the questions, multiple choices could be selected.Participation was voluntary and no incentives were given.Informed consent was gotten verbally and via email after the dermatologists explained the study in detail.
The rationale/basis
The study was conceived because of the gap in knowledge about the utilization of telemedicine in Nigeria.With the COVID-19 pandemic, there were more innovations,especially with telemedicine.Dermatology being a visual speciality was one of the fields where it was deployed,and it was important to report the experience with the application in practice.
Validation of questionnaire
The usability and functionality were pretested and validated prior to being sent out on 10 patients each by the two dermatologists in this article.
Modes of questionnaire administration, type, number of contacts, time frame and location.
The survey was a closed survey as it was sent out only to patients who booked outpatient appointments with the dermatologist over the one-year period that was reported.The patients were contacted by email and a follow-up call simultaneously and all those that agreed to participate were sent the questionnaire.The collection period was over a month and reminders were sent via email and text message to the respondents.
Participation and response
The collection period was over a month and reminders were sent via email and text message to the respondents.Participation was voluntary and no incentives were given.Informed consent was gotten verbally and via email after the dermatologists explained the study in detail.The response rate for those that booked a physical consultation was 50% while it was 68.4% for those that booked a virtual consultation.The questionnaire was completed fully by all the respondents which are likely due to the small sample of participants and the follow-up call where it was explained that all the questions should be answered.There was a non-response option of “not applicable” provided with questions that had a need for non-response.All the respondents filled out the questionnaire only once.
Statistical analysis
The obtained data were entered into an Excel spreadsheet and analyzed with SPSS version 22.0 (IBM Corp., Armonk,NY, USA).Continuous variables are expressed as mean and standard deviation, and categorical variables are expressed as percentage.Thettest was used to compare means,and the chi-square test was used to compare percentages.Statistical significance was set at aPvalue of < 0.05.
Results

Figure 1.Distribution of responses regarding how patients became aware that they could book a dermatologist appointment online.
A total of 60 patients booked an appointment on the platforms from April 2021 to March 2022, with 38 (63.3%) of them being virtual consultations and 22 (37.7%) of them physical consultations.The response rate for patients who booked a physical consultation was 50.0% (11 patients),while that of patients who booked a virtual consultation was 68.4% (26 patients).There was no significant difference in age between patients who booked virtual and physical consultations (33.8 ± 9.7vs.31.8 ± 8.3 years, respectively;P= 0.42).Twenty-four (92.3%) of the respondents who booked a virtual consultation were seen via real-time video consultation, while only 2 (7.7%) consulted using the storeand-forward method.Nineteen (73.1%) of the respondents who booked a virtual consultation were women,while 7 (63.6%) of those who booked a physical consultation were women (P= 0.32).All patients who booked both virtual and physical consultations were educated to college level, with more than half of the patients who booked a virtual consultation having a postgraduate degree after college compared with 18% of those who booked a physical consultation (P= 0.07).Five of the patients who booked a virtual consultation were from outside Nigeria (2 from Canada, 2 from the United Kingdom, and 1 from Ireland).Among the patients living in Nigeria who booked a virtual consultation, 14 (53.8%) were in the same state as the dermatologists, whereas all but 1 patient who booked a physical consultation were in the same location as the dermatologists (P= 0.01).All patients who booked virtual consultations knew there were dermatologists in Nigeria prior to booking the appointment, while only one of the patients who booked a physical appointment was unaware that there were dermatologists in Nigeria.The patients became aware that they could book an appointment with a dermatologist online through different means, as highlighted in Fig.1.
The median duration of symptoms among patients who booked a virtual consultation was 16 (interquartile range,43.5) weeks, while the duration of symptoms among those who booked a physical consultation was 99.9 ± 154.09 weeks.A total of 63.6% of the patients who booked a physical consultation had more than 1 presenting symptom, while 34.6% of those who booked a virtual consultation had more than 1 presenting symptom.The most common presenting symptoms in patients who booked a virtual consultation were bumps on the face (50.0%),followed closely by hyperpigmentation (46.2%) and pruritus (34.6%).The most common presenting symptom in patients who booked a physical consultation was hyperpigmentation (81.8%), followed by pruritus (63.6%) and bumps on the skin (27.2%).The benign tumors were dermatosis papulosa nigra and syringoma.
The most commonly affected area in patients who booked both virtual and physical consultations was the face (61.5% [n= 16] and 54.5% [n= 6], respectively).The skin lesions affected multiple areas in 54.5% (n= 6) and 38.4% (n= 10) of those who booked physical and virtual consultations, respectively.A total of 80.7% (n= 21)and 63.6% (n= 7) of patients who booked a virtual and physical consultation respectively sought treatment prior to booking a dermatologist appointment, with several patients using multiple treatments as shown in Fig.2.
The skin condition did not improve in any of the patients who booked a physical consultation after the preliminary treatment, and the skin condition worsened in 2 (28.5%)of them.Mild improvement was noted in 3 (14.3%) of the patients who booked a virtual consultation after the preliminary treatment, whereas the skin condition worsened in 3 (14.3%) and showed no improvement in 15(71.4%) (Table 1).
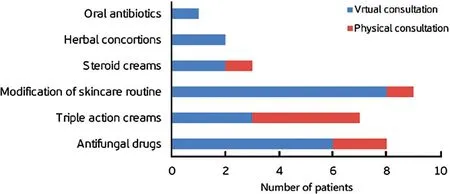
Figure 2.Treatments used prior to seeing a dermatologist.
Seventeen (65.4%) of the patients who booked a virtual consultation and 9 (81.8%) of those who booked a physical consultation did not have an idea what their diagnosis was prior to seeing the dermatologist.Acne was the most common final diagnosis made in patients who booked a virtual consultation.The distribution of the diagnoses made by the dermatologists is shown in Fig.3.
A total of 61.5% (n= 16) and 81.8% (n= 9) of patients who booked virtual and physical consultations, respectively, found it very easy to access the platform used.In total, 30.8% (n= 8) and 27.2% (n= 3) of patients who booked virtual and physical consultations, respectively,had reservations prior to booking the appointment.A total of 63.6% (n= 7) of patients who booked a physical appointment chose physical over virtual because they preferred the feel of a physical consultation, while 53.8%(n= 14) of patients who opted for a virtual consultation did so because of the convenience.Only 11.5% (n= 3)of patients who booked a virtual consultation booked it because of the COVID-19 pandemic.In total, 65.4% (n=17) of patients who booked a virtual consultation opined that they would still have booked a virtual consultation even without the COVID-19 pandemic, whereas 38.5%(n= 10) agreed that they now preferred a virtual consultation over a physical consultation.A total of 36.4%(n= 4) of patients who booked a physical consultation responded that they would likely book a virtual consultation in the future.All patients agreed that the consultation afterward met their expectations; however, 2 (7.1%)of those who consulted virtually and 1 (9%) of those who consulted physically experienced no resolution of symptoms after the consultation (P= 0.89).None of the patients underwent a biopsy.A total of 30.8% (n= 8),57.6% (n= 15), 7.7% (n= 2), and 1 (n= 3.8%) of the patients who booked a virtual consultation stated that the network during the consultation was excellent, very good,good, and poor, respectively.
A total of 81.8% (n= 9) and 76.9% (n= 20) of patients who booked physical and virtual consultations,respectively, found it very easy to pay for the consultation on the platform using their debit card.The price of a physical consultation at 25,000 naira ($42 USD) was considered fair by 81.8% (n= 9) and expensive by 19.2%(n= 2) of the patients who booked a physical consultation, while the cost of a virtual consultation at 20,000 naira ($35 USD) was considered fair by 76.9% (n= 20)and expensive by 23.1% (n= 6) of those who booked a virtual consultation.

Table 1 Channels through which patients sought treatment prior to booking an appointment, n (%).
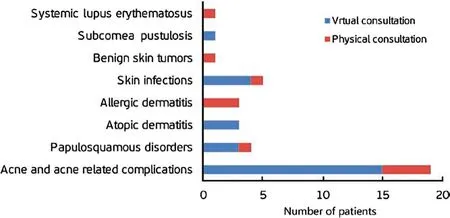
Figure 3.Final diagnosis made by the dermatologists.
Discussion
TD has become widely used in most developed countries,10-13and its use is gradually increasing in developing countries.3The benefits of adopting TD are especially important in countries with a limited number of dermatologists, such as Nigeria.In 2021, a review of a TD platform by Okoro and Shittu6revealed that patients had high interest in but low usage of the platform.The platform, which made use of the store-and-forward method,had only 3 patients who paid for consultation within 2 years (2016-2018).That review was the first to examine TD practice in Nigeria.Several telemedicine platforms have recently become officially established in Nigeria,especially because of the COVID-19 pandemic.7Several of these platforms are now widely known and utilized,particularly by people in urban areas.For the currently available platforms, both the dermatologists and the patients register on the platform before the patient book a consultation.The patient can view the dermatologist’s profile, picture, and qualifications prior to booking the appointment.
In the present review, the number of patients who booked an appointment on the platform to see a dermatologist was significantly higher than that in the first review.Factors responsible for this difference may be attributed to the increased use of social media by both patients and doctors, which has increased the visibility of both the platforms available and that of the dermatologists, considering that social media and referrals from friends were the most common means that patient learned about booking a virtual consultation.This is not surprising because the use of social media by physicians for personal and professional reasons has improved in recent times.14-16Lifestyle modifications by patients based on interventions from social media have significantly increased as healthcare workers may be able to pass the information to a larger number of people in more socially acceptable ways.17-18The dermatologists in this review had well-established social media platforms on which they frequently advocated for skin health.The patients’ level of education may also be partly responsible for the use of TD services because the majority of those who booked a virtual consultation had a postgraduate degree.The patients who utilized the platform to book the appointments (whether physical or virtual)were educated to at least college level, and most of them had no difficulty navigating the platform and paying for the consultation.
Women booked more appointments with a dermatologist online than did men, which could reflect the health-seeking behavior of women.19The most common symptoms were lesions on the face and pruritus in patients who booked a virtual consultation, whereas hyperpigmentation followed by pruritus were the most common complaints among those who booked a physical consultation.This is not surprising because acne was the most common reason for booking a virtual consultation, and most patients had used a preliminary treatment prior to seeing a dermatologist.The diagnosis made after the consultations varied widely from acne to papulosquamous disorders and skin infections; this differed from the pattern of skin diseases at various outpatient clinics across Nigeria, where skin infections were among the most commonly encountered conditions.20-21This may be explained partly by the fact that most patients with skin infections would have attained relief by consulting with their primary doctors.Modification of skincare routines, antifungal drugs, and triple-action creams were the most frequently utilized treatments prior to the consultation.Triple-action creams, which are widely abused in Nigeria, usually contain a combination of an antifungal (often clotrimazole), antibiotic(such as neomycin), and high-potency steroid (such as clobetasol dipropionate).A study in South East Nigeria revealed that up to 66% of primary doctors prescribed triple-action creams as first-line treatment, while only 25% knew that triple-action creams are not beneficial in treating skin conditions.22
Only a few patients had reservations about booking the TD appointment; their reasons included concern regarding whether the platform was a fraud, whether a virtual consultation would be enough to address all their issues,and whether the quality of the network would be adequate during the consultation.Most patients who booked a virtual consultation booked the appointment because of the convenience, followed closely by the presence of the COVID-19 pandemic.All the patients who booked a virtual consultation agreed that it met their expectations, and the majority had good Internet service during the consultation.The outcome of both the virtual and physical consultations was comparable because there was no significant difference in the clinical outcome between patients who booked physical versus virtual consultations.Up to one-third of patients who booked a physical consultation opined that they would be willing to book a virtual consultation in the future because of the convenience.However, most patients still preferred a physical consultation to a virtual consultation despite the fact that they were satisfied with the consultation because they felt the doctors were knowledgeable and paid attention to details during the consultation.Patients also had the email addresses of the reviewing dermatologists and could send pictures in cases where the quality of the network was fluctuating.
Developing countries are now adopting the use of TD,especially in rural areas and as a means of increasing the reach of dermatology services to the difficult-to-reach areas of the country where dermatology services are limited.3,23This review shows that rural areas are still not utilizing TD services in Nigeria.Possible contributing factors may include lack of awareness, limited Internet facilities, and lack of proper existing structures to disseminate TD services to rural areas.The cost of the consultation may also be a limiting factor to the use of TD in rural areas, and dermatologists may need to provide the services free as corporate social responsibility or at a highly reduced rate.The store-and-forward method by the primary doctors to the dermatologists may also be a more efficient way to adopt TD in rural areas.However, the utilization of TD has improved in urban areas and may serve as a means of improving the reach of dermatology care in Nigeria, especially if properly integrated into primary and secondary healthcare facilities where dermatologists are limited.Dermatologists should also use social media in an ethically acceptable manner to improve visibility and increase awareness about skin health.
The limitation of the study was the inability to perform biopsies.However, only two cases required a biopsy but improved with management after a clinical diagnosis.There was also a time lag between when the patients were seen and when the questionnaires were carried out, especially for the patients seen earlier in the year.This may have been associated with poor recollection of events.Also the major limitation of TD, which is also evident in the present review, is the inability to perform biopsy and other procedures for the patients.Patients whose condition did not improve after management were encouraged to come in for a physical consultation and further evaluation.
In conclusion, TD holds great promise and may allow dermatology care to become readily available across the country.Greater advocacy is needed at all levels regarding the availability of such services in the country, especially in rural areas; this may improve the overall utilization of the services.Proper structures such as electronic medical record-keeping, data safety, and improved Internet services will also be highly beneficial to increasing the reach of TD.
杂志排行
国际皮肤性病学杂志的其它文章
- Transcription and Secretion of lnterleukin-1β and HMGB1 in Keratinocytes Exposed to Stimulations Mimicking Common lnflammatory Damages
- Dermoscopic Assessment of Pityriasis Versicolor: A Cross-Sectional Observational Study
- Evaluation of Serum Vitamin D Concentration and Blood Eosinophil and Basophil Counts in Patients With Vitiligo: A Cross-sectional Study From Rafsanjan and Zarand, Iran
- Basal Cell Carcinoma Excision Guided by Dermoscopy: A Retrospective Study in Macau
- The Role of Endoplasmic Reticulum Stress in Melanoma
- The Relationship Between Ultraviolet B and DNA Methylation in Skin Cancers
