Randomized intervention and outpatient follow-up lowers 30-d readmissions for patients with hepatic encephalopathy, decompensated cirrhosis
2023-07-04AntoinettePusateriKevinLitzenbergClaireGriffithsCaitlinHayesBipulGnyawaliMichelleManiousSeanGKellyLanlaContehSajidJalilHaikadyNagarajaKhalidMumtaz
Antoinette Pusateri, Kevin Litzenberg, Claire Griffiths, Caitlin Hayes, Bipul Gnyawali,Michelle Manious, SeanG Kelly, Lanla F Conteh, Sajid Jalil,Haikady N Nagaraja, Khalid Mumtaz
Abstract
Key Words: Decompensated cirrhosis; Hospital readmissions; Interventions
INTRODUCTION
Cirrhosis affects approximately 5 million annually[1] and has been reported to be the 8thleading cause of death with more than 40000 deaths annually in the United States[2].A study on the burden of gastrointestinal (GI), liver, and pancreatic diseases in the United States revealed that liver diseases had the highest mortality at 3.1%[3].In addition to high mortality, cirrhosis is also associated with high morbidity.The sequelae of decompensated cirrhosis (DC) are often managed during hospital admissions and include volume overload in the form of ascites, edema or hepatic hydrothorax, portal hypertension leading to bleeding esophageal or gastric varices, as well as hepatic encephalopathy (HE),hyponatremia, acute kidney injury (AKI), and spontaneous bacterial peritonitis (SBP)[4].
Several studies have demonstrated hospital readmissions in DC place a large financial burden on the United State healthcare system.The 30-d readmission rate has been reported to be 20%-37%[5-14].We have recently published on early readmission rates up to 27% in patients with DC and developed the Mumtaz readmission risk score based on United States data[15].We also reported that nearly one-third of patients with HE were readmitted within 30 d, and early readmission adversely impacted healthcare utilization and calendar-year mortality[16].
Interventions to reduce readmissions have been shown to be safe and effective.For instance, Moraleset al[17] developed a program including a hepatologist follow-up exam within 7 d after discharge.This program resulted in a reduction in 30-d readmissions, 60-d mortality, emergency department visits and associated costs[17].Similarly, another group demonstrated that follow-up with a “care management check-up”as opposed to “standard outpatient care”reduced 30-d readmission, 12-mo mortality and saved 1500 euros per patient month of life[18].
There is a paucity of prospective studies on interventions to reduce early readmission rates in patients with DC.Therefore, we prospectively studied 30-d readmission rates in patients with DC and compared various interventions (INT) with standard of care (SOC) to reduce early readmission rates.We hypothesized that DC patients in the INT arm would have decreased 30-d readmissionvsthe SOC arm.
MATERIALS AND METHODS
This study was conducted at the Ohio State University Wexner Medical Center (OSUWMC), Columbus,Ohio from July 2019 to December 2020.Our study was approved by OSUWMC Institutional Review Board.All aspects of the studying involving human participants including informed consent for enrollment were in accordance with the ethical standards of our Institutional Review Board and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Screening
All patients admitted with DC to the hepatology (inpatient or consult) service were screened for enrollment.Patients meeting inclusion criteria were approached for study consent.Of note, due to the global coronavirus disease 2019 (COVID-19) pandemic, beginning March 2020, only COVID negative patients were approached for informed consent.Elective readmissions for inpatient procedures including endoscopy, trans-arterial chemoembolization, transjugular intrahepatic portosystemic shunt(TIPS), paracentesis or readmissions unrelated to DC such as motor vehicle accidents were excluded.
Randomization and data collection
Study data were collected and managed using research electronic data capture (REDCap) hosted at The Ohio State University Wexner Medical Center[19,20].Informed consent was obtained from all individual participants included in the study.Consented patients were randomly assigned to either the INT arm or the SOC arm in a 1:1 ratio using the REDCap randomization tool.The following data were collected on all patientsviaREDCap software including demographics (age, sex, insurance type, income based on the zip code), hospitalization data [date of index admission defined as initial admission during which patient consented for study, reason for admission, length of stay (LOS) defined as difference in days between index admission date and index admission discharge date, discharge disposition,associated cost of care of admission as obtained through medical record billing tab], etiology of cirrhosis(alcoholic and non-alcoholic including viral, non-alcoholic fatty liver disease, autoimmune, primary biliary cirrhosis, primary sclerosing cholangitis or cryptogenic), complications of cirrhosis (HE, AKI,ascites, variceal bleeding, SBP, hepatorenal syndrome, coagulopathy, portal hypertension, hepatopulmonary syndrome, hepatocellular carcinoma), and procedures performed during admission[esophago-gastro-duodenoscopy, colonoscopy or flexible sigmoidoscopy, paracentesis, TIPS and hemodialysis (HD) on admission and discharge].We also collected data including Elixhauser comorbidity index, discharge medications, and laboratory data (complete blood counts, serum creatinine, liver function tests including total bilirubin, INR, and sodium).Child Turcotte Pugh (CTP)and Sodium-model for end stage liver disease (MELD-Na) score were calculated from the data.The nurse case manager (CM) also recorded labs & medications at readmission and discharge and associated cost of readmission.Status of early readmission, liver transplantation, and mortality at one year were also collected.
Follow-up
The CM phoned each patient enrolled in either arm weekly for 30 d after index discharge to find out if the patient has been readmitted to OSUWMC or another hospital.In the INT arm, during the call CM also ensured i) early (defined as within 30 d from index admission discharge) outpatient hepatology follow-up ii) compliance of medication, iii) arrangement of outpatient paracentesis if needed, and reviewed outpatient hepatology clinic follow-up records.SOC arm as per our center’s protocol had to be taken care of by the primary inpatient team.This included arranging early outpatient clinic follow-up,providing list of medications, and advice for outpatient paracentesis if needed at the time of discharge.Due to the nature of intervention, the study could not be blinded.
Definition of outcomes
Early readmission was defined as admission within 30 d of index admission discharge.Reasons for readmission were gathered by CM by reviewing the electronic medical record (EMR) of all enrolled patients readmitted at OSUWMC or outside hospital within 30 d of index admission.Predictors of early readmission were also compared in the two arms.
Sample size
Based on the sample size calculation, target of recruitment for the study was 848 patients, admitted to the hospital with DC under the hepatology (inpatient and consult) services.Patients were randomly assigned in a 1:1 ratio into INT or SOC arms.Based on our previous study using the National Readmissions Administrative Database, we expected a 30-d readmission rate of 27% among patients meeting inclusion criteria, which yield 114/424 patients with 30-d readmission events, thus meeting the target sample size.Based on this calculation, a total sample size of 848 (424 per group) provided 80%power to detect a 30% decrease in 30-d readmission rate (from 27% to 19%) with a type I error rate of 0.05.However, planned sample size could not be achieved due to the COVID-19 pandemic related restriction started in our center in March 2020.Therefore, we end up with available sample size of a total of 240 patients.The modified consort flow diagram for enrollment in our study trial is illustrated in Figure 1.
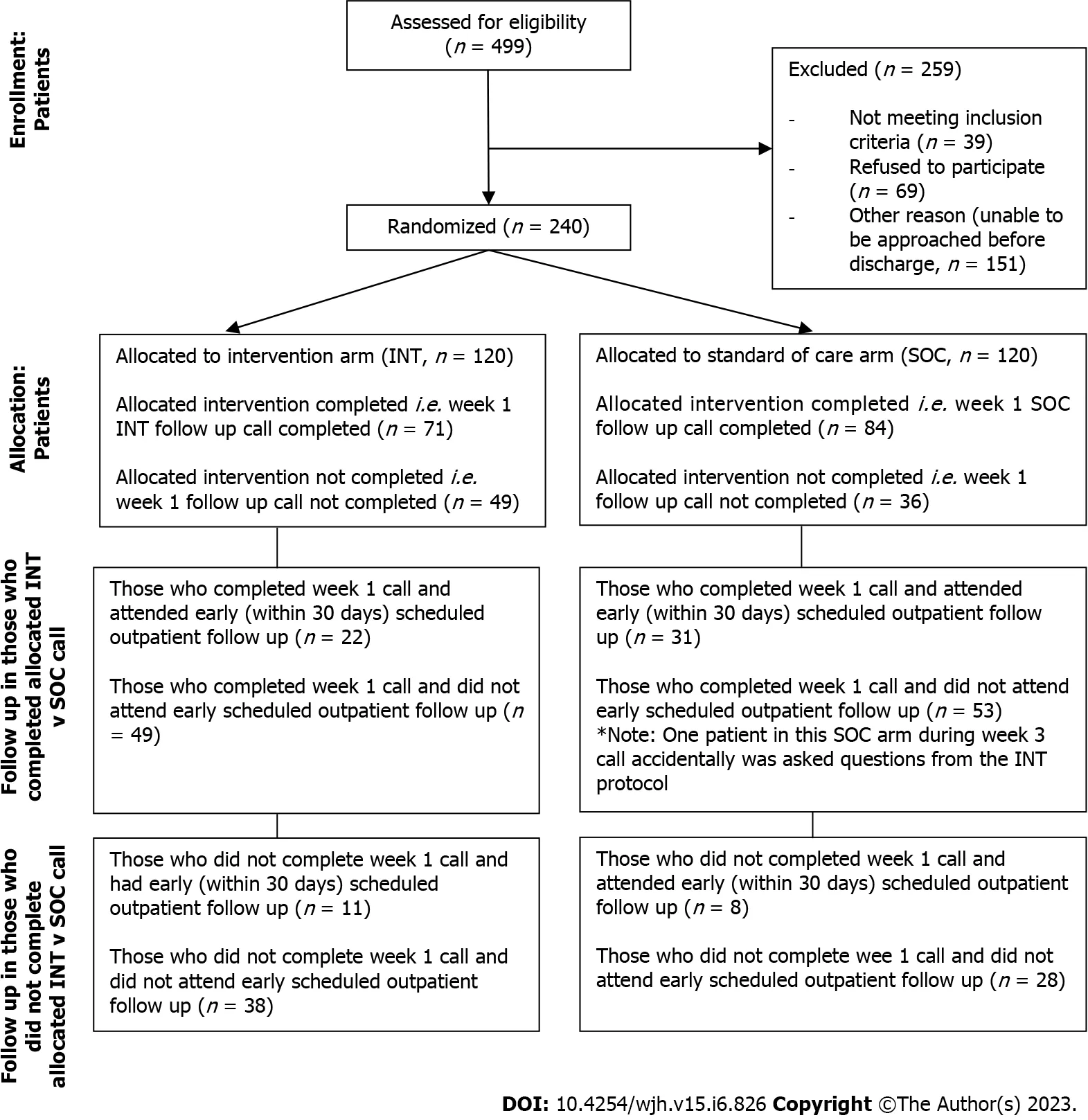
Figure 1 Modified consort flow diagram of patients eligible for enrollment in study trial.INT: Intervention; SOC: Standard of care.
Statistical analysis
Means of continuous response variables between two groups were compared using robust t-test (Welch test).Proportions were compared using χ-test or Fisher’s exact test as applicable.Logarithmic transformation was used for comparing the LOS and admission cost across groups.Level of significance was kept at 0.05 for each comparison.JMP Version 15 (SAS Institute, NC) was used for all the analyses.
RESULTS
Initial screening data
From July 1, 2019, to December 1, 2020, 1392 patients were screened.Due to the COVID-19 pandemic,recruitment was held from March 2020 to July 2020 and subsequently resumed until December 2020.Out of the patients screened, only 499 (35.85%) were eligible for inclusion; however, 240 patients consented and randomized: 120 each into the INT and SOC arm (Figure 1).
Patient demographics and clinical characteristics
The mean age of patients was 56.34 ± 11.19 years, majority were males (135, 56.25%), belonged to White race (n= 202, 84.17%) and non-Hispanic or Latino ethnicity (n= 227, 94.58%).Almost two-thirds of the patients had public insurance (n= 76, 31.67% on Medicare andn= 70, 29.17% on Medicaid); 73 (30.42%)had private insurance.At admission, the mean MELD-Na score and mean CTP Score were 21.89 ± 8.03 and 9.36 ± 1.96, respectively.Major etiology of cirrhosis was alcohol (n= 121, 50.42%) followed by nonalcoholic fatty liver disease (n= 79, 32.92%) and viral hepatitis (n= 43, 17.92%).Furthermore, 116(48.33%) patients were actively under evaluation for liver transplantation.
Characteristics of index admissions
The index admission mean LOS was 8.13 ± 5.83 d (median 6, range 1-43 d).The mean cost of index admission was $60595 ± $47174 (n= 225, median $42932, range $1630-251991).The top five reasons for index admission included volume overload (n= 111, 46.25%), AKI (n= 65, 27.08%), hepatic encephalopathy (n= 45, 18.75%), variceal bleed (n= 42, 17.50%), lower GI bleed (n= 19, 7.92%) and hyponatremia (n= 16, 6.67%).The top five interventions performed were esophago-gastro-duodenoscopy (n= 136, 56.67%), paracentesis (n= 115, 47.92%), colonoscopy/flexible sigmoidoscopy (n= 24, 10%), HD (n= 15, 6.25%) and TIPS (n= 10, 4.17%).Most patients were discharged from index admission to home (n= 159, 66.25%) followed by home with health care (n= 42, 17.50%) and skilled nursing facility (n= 32, 13.33 %, Table 1).
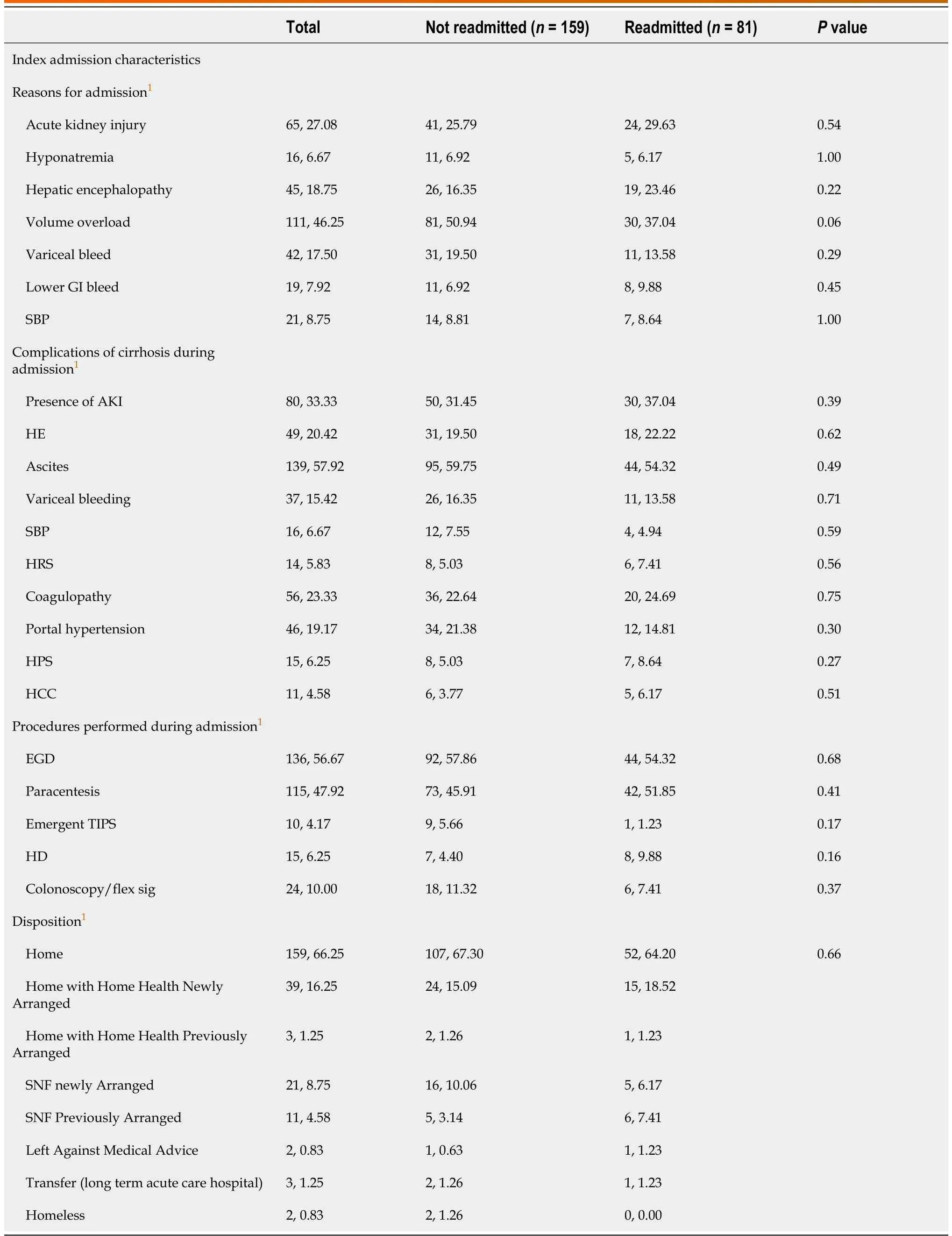
Table 1 Characteristic features of index admission by readmission status, n (%)
Characteristics and reasons for early readmissions
Overall, 81 (33.75%) patients were readmitted within 30 d of discharge.The major reasons for first readmission included hepatic encephalopathy (n= 26, 32.10%) followed by volume overload (n= 22,27.16%), AKI (n= 16, 19.75%), variceal bleed (n= 12, 14.82%) and hyponatremia (n= 10, 12.35%).14 patients were readmitted twice, 3 admitted thrice and one admitted 5 times within 30 d.The mean time to first readmission was 12.65 ± 7.55 d (median 12 d, range 1-30 d).The mean LOS of first readmission was 8.11 ± 8.98 days.The mean cost of stay of first readmission was $55548.29 ± $65164.91 (Table 2).Those readmitted had a higher MELD-Na score on index admission (23.54 ± 7.80vs21.05 ± 8.03,P=0.02) and index discharge (21.67 ± 7.95vs19.39 ± 6.89,P= 0.03) than those not readmitted.Similarly,those readmitted had a higher index admission creatinine (1.80 ± 1.53vs1.39 ± 1.16,P= 0.03), index discharge creatinine (1.61 ± 1.34vs1.20 ± 0.97,P= 0.02), and higher index admission INR (1.80 ± 0.64vs1.63 ± 0.50,P= 0.05) than those not readmitted.
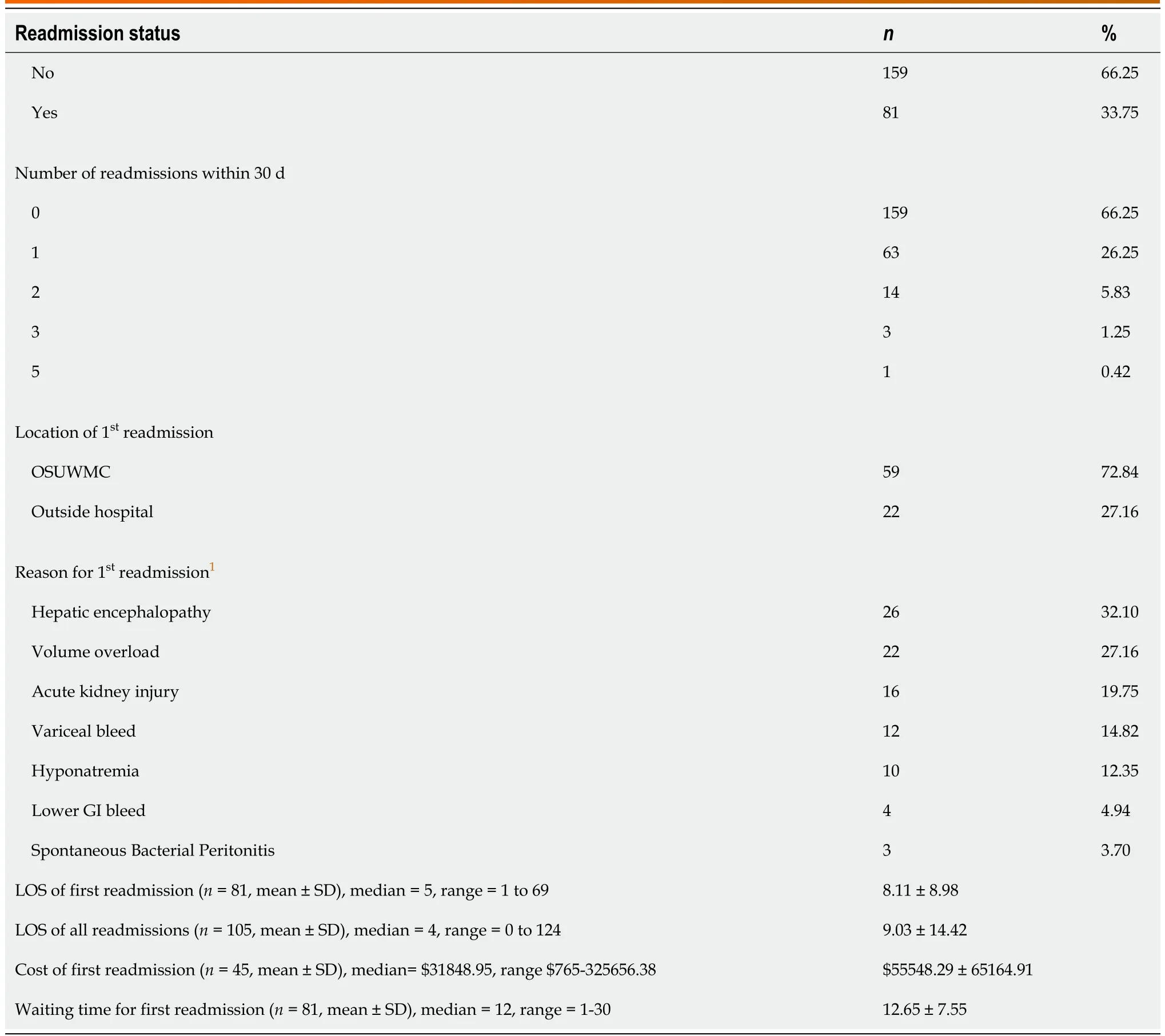
Table 2 Characteristics and reasons for readmission
Comparison of demographics and clinical characteristics in two intervention arms
Demographics including age, race, ethnicity, income, and insurance were comparable in two groups, as well as etiology of cirrhosis, MELD-Na score, CTP score, status of evaluation for liver transplant.There were majority females in the INT arm (60/120, 50%vs45/120, 32.50%) and males in SOC arm (75/120,62.50%vs60/120, 50%,P= 0.03, Table 3).Index admission characteristics, disposition and index admission were also comparative in two arms (Tables 4 and 5).

Table 3 Comparison of patient demographics and clinical characteristics by randomization arm, n (%)

Table 4 Characteristic features during index admission in two randomization arms, n (%)

Table 5 Clinical and laboratory features during index admission and discharge in two randomization arms, n (%)
Comparison of reasons of 1st readmission and outcomes in the INT vs SOC arm
There was no difference in the readmission rates for patients in the INT (n= 4, 35.83%)vsSOC arm (n=38, 31.67%,P= 0.59, Table 6).Other outcomes including number of readmissions within 30 d (P= 0.65),index admission cost (P= 0.49), index admission LOS (P= 0.63), 1streadmission LOS (P= 0.58), all readmissions’LOS (P= 0.82) and waiting time for 1streadmission (P= 0.06) were comparable in two arms.
从图10中可以看出,ACI取值较为保守,EC2与MC2010较贴近试验值。当试验值取值较小时,各国规范取值基本一致;当试验值取值较大时,各国规范取值的差异性较为明显。
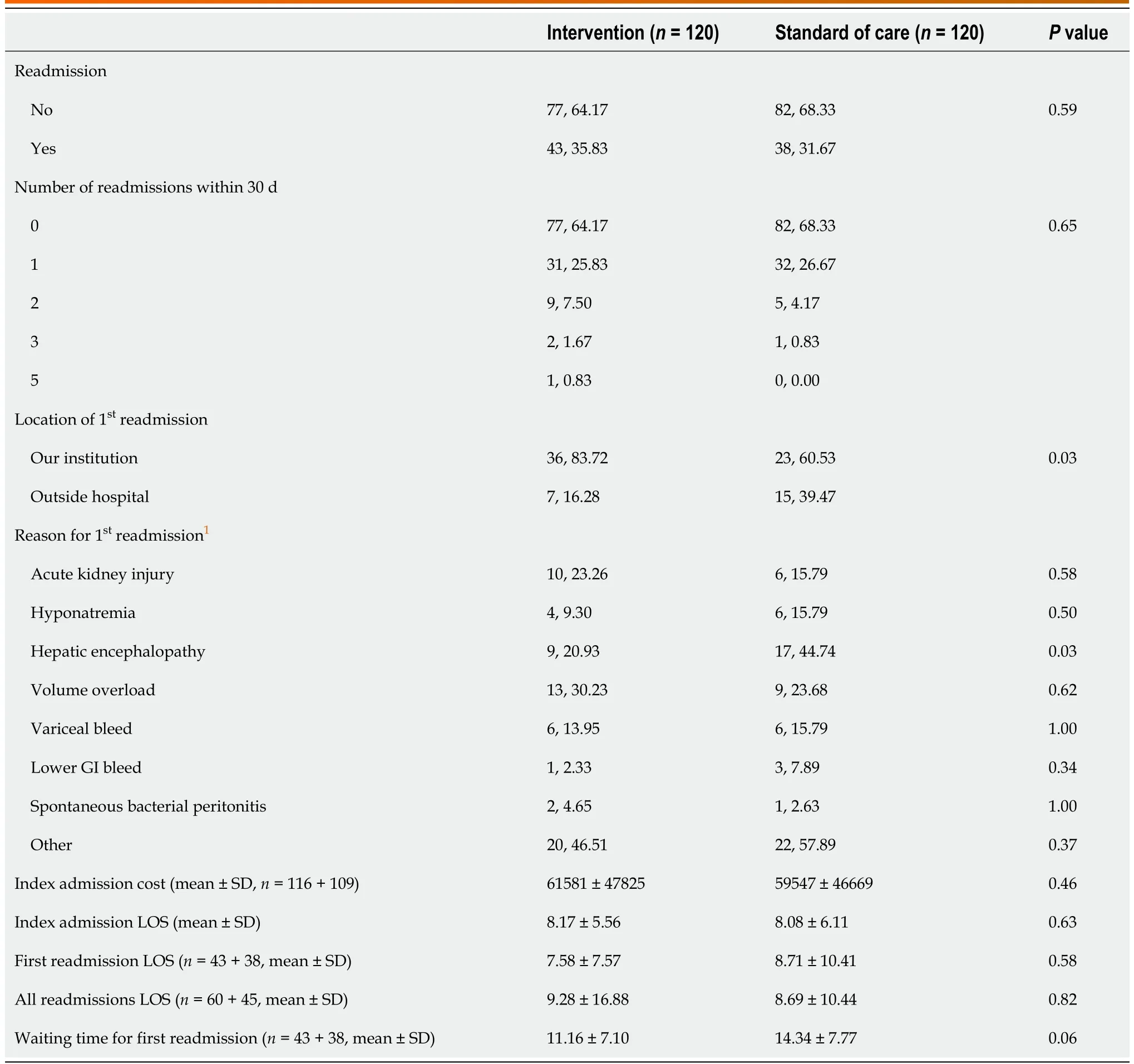
Table 6 Outcomes and reasons of readmission characteristics by randomization arms, n (%)
Statistically significant differences were noticed in INT arm in location of 1streadmission (n= 36,83.72% at OSU as compared ton= 23, 60.5% outside hospital,P= 0.03), and lesser 1streadmission with HE in the INT arm (n= 9, 20.9%)vsSOC (n= 17, 44.7%,P= 0.03).Finally, contingency analysis of readmission data showed fewer readmissions in patients who attended outpatient follow-up within 30 days of discharge from index admission (n= 17, 23.61%vs n= 55, 76.39%,P= 0.04).
At the end of our study, 47 (19.58%) patients received a liver transplant and 62 (25.83%) died; among those who died, 5 patients were post-transplant and 22 died in hospice.Due to the COVID-19 pandemic we were unable to achieve the anticipated sample size.Therefore, multivariate analysis was not performed.
DISCUSSION
This prospective randomized study investigated early readmission rates and healthcare utilization in patients with DC.Our readmission rate of 33.75% is higher than the United States national average(27%).While our nurse CM interventions did not reduce told readmissions, we found that HE was the top reason for readmission and such interventions were helpful in reducing early readmissions in patients with HE.This is an important lesson learned given increased burden of HE on hospitalizations,falls, mortality, impaired quality of life and caregiver burden[21].In the validation of readmission using the liver-renal-risk score or “LIRER score”, Freitaset al[22] showed that HE was not only a predictor of30 d readmission independent of MELD score, index, first-year, two-years and overall mortality, but also HE at admission had significantly higher mean LIRER scores.Furthermore HE patients on Medicare and geographically from the South or Midwest have higher in-hospital mortality[23].Considerable research has been done to address HE readmissions.Bajajet al[24] found that efforts to reduce medication-precipitated HE, prevent aspiration pneumonia and optimize HE medications on hospitaldischarge should be areas of focus to decrease HE readmissions.Tapperet al[25] demonstrated that development of a checklist for HE protocols integrated into the EMR and order entry system reduced odds of 30-d readmission for patients with HE (from 39.2% to 27.6%).Thus, our results are congruent with existing evidence that interventions should be invested in post-discharge education andcommunication for all patients with cirrhosis, especially with HE.
One of the components of intervention in our study was to arrange appointment of patients in the clinic within a week with their hepatologist.Patients with DC who attended their follow up appointment within 30 d of discharge from index admission had fewer readmissions.This suggests that overall,in our cohort, outpatient linkage with a hepatologist should be a priority to reduce readmission rates[26].Moraleset al[17] in their retrospective program looked at the impact of follow-up of cirrhotics within 7 d after discharge with a hepatologist.They reported reduced 30-d readmission, 60-d mortalityand rate of emergency department visits and associated costs in those who followed up within 7 d.Morandoet al[18] demonstrated that follow up with a “care management check-up”group as opposed to “standard outpatient care”reduced 30-d readmission, reduced 12-mo mortality, and saved almost 1500 euros per patient month of life.While Kanwalet al[9] found early outpatient follow-up after discharge was associated with a small increase in readmissions, they found an lower overall mortality in their patients with cirrhosis admitted to Veterans Affairs hospitals.Thus our results are also consistent with the current evidence that patients with DC likely benefit from early post-hospitalization follow up with specialty providers[27,28].
One of the major limitations of our study was inability to enroll patients according to the proposed sample size due to the COVID-19 pandemic.Our study was underpowered to perform multiple regression analysis to detect differences in readmission rates in INTvsSOC arm.From March 2020 to July 2020 our recruitment process was put on hold due to hospital regulations to reduce patient and staff exposure.Despite this major limitation, we were able to enroll 80.17% (279 consented out of 348 approached) of patients in our study.
This study was also performed in the setting of a large academic medical center and a high-volume liver transplant center.While our methods and results may be applicable to the clinical practice of other such centers, the same impact may not be appreciated by smaller, community hospitals that are not liver transplant centers.
Future work in patients with DC should continue to focus on prospective intervention strategies to reduce early readmissions and educate patients and providers.To achieve desired sample size, we would suggest collaborations with various centers to identify and recruit patients with DC into a multicenter prospective cohort.Given our finding that there were fewer readmissions in patients with follow-up within 30 d, studies should evaluate the use of telehealth visits for follows up, especially in the COVID19 era, as outlined by Stottset al[29].
CONCLUSION
In conclusion, this prospective randomized study investigated the impact of various pragmatic interventions to reduce early readmission and healthcare utilization in patients with DC.Our study was underpowered to detect statistically significant differences in readmission rates in INTvsSOC arm.We reported that readmission rate of our medical center was 33.75% and HE was the top reason for readmission.We found a reduction in early readmission in patients with HE in the INT arm and those who attended their follow up appointment within 30 d of discharge from index admission.We demonstrated that simple interventions in patients with DC are pragmatic and there is need for more prospective multicenter trials in this area of research.
ARTICLE HIGHLIGHTS
ACKNOWLEDGEMENTS
This research was supported by the Clinical Research Center/Center for Clinical Research Management of The Ohio State University Wexner Medical Center and The Ohio State University College of Medicine in Columbus, Ohio.The project was entitled “GASTR29: Prospective validation of readmission risk score and interventions to prevent readmission in patients with decompensated cirrhosis (CCTS ID#:6018)”.This project was funded by the Ohio State University Self Insurance Program and supported by NIH Award Number UL1TROO2733 from the National Center for Advancing Translational Science.We also give a special thanks to our nurse case managers from The Ohio State University Wexner Medical Center Clinical Research Center for their work in the weekly patient calls: Holly Bookless, RN, Elizabeth Cassandra, RN and Dina McGowan, RN.
FOOTNOTES
Author contributions:Pusateri A and Mumtaz K study design, team administration, training team members for recruiting, recruiting patients for study, interpreting data, drafting manuscript; both approved the final submitted version of this manuscript; Litzenberg K, Griffiths C, Hayes C, Gnyawali B and Manious M recruiting patients for study, drafting manuscript, approved the final submitted version of manuscript; Jalil S, Kelly S and Conteh L reviewed and edited the final draft of the manuscript; Nagaraja K analyzed data, edited manuscript, and approved the final submitted version of this manuscript.
Supported byGASTR29: Prospective validation of readmission risk score and interventions to prevent readmission in patients with decompensated cirrhosis (CCTS ID#: 6018).
Institutional review board statement:This study was conducted at the Ohio State University Wexner Medical Center(OSUWMC), Columbus, Ohio from July 2019 to December 2020.Our study was approved by OSUWMC Institutional Review Board.All aspects of the studying involving human participants including informed consent for enrollment were in accordance with the ethical standards of our Institutional Review Board and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Institutional animal care and use committee statement:This is not applicable to our study.
Informed consent statement:All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United States
ORCID number:Antoinette Pusateri 0000-0002-8458-7827; Bipul Gnyawali 0000-0003-4745-2787; Sean G Kelly 0000-0002-9434-9924; Lanla F Conteh 0000-0002-4372-993X; Sajid Jalil 0000-0001-6123-153X; Khalid Mumtaz 0000-0001-7868-6514.
S-Editor:Liu XF
L-Editor:A
P-Editor:Yuan YY
5Berman K, Tandra S, Forssell K, Vuppalanchi R, Burton JR Jr, Nguyen J, Mullis D, Kwo P, Chalasani N.Incidence and predictors of 30-day readmission among patients hospitalized for advanced liver disease.Clin Gastroenterol Hepatol2011;9: 254-259 [PMID: 21092762 DOI: 10.1016/j.cgh.2010.10.035]
杂志排行
World Journal of Hepatology的其它文章
- Management of sepsis in a cirrhotic patient admitted to the intensive care unit: A systematic literature review
- Liver injury from direct oral anticoagulants
- Lower alanine aminotransferase levels are associated with increased all-cause and cardiovascular mortality in nonalcoholic fatty liver patients
- Acute pancreatitis in liver transplant hospitalizations: Identifying national trends, clinical outcomes and healthcare burden in the United States
- Role of vascular endothelial growth factor B in nonalcoholic fatty liver disease and its potential value
- Tumor budding as a potential prognostic marker in determining the behavior of primary liver cancers
