孕晚期阴道微生态失调对新生儿败血症的影响
2023-06-05弓培慧贾晓云康娅楠张岳琴李秀辉周浩白丽霞
弓培慧 贾晓云 康娅楠 张岳琴 李秀辉 周浩 白丽霞
Abstract Objective:To analyze the correlation between vaginal microecology disorder in the third trimester and neonatal septicemia,so as to provide a reference for better prevention and treatment of neonatal septicemia.Methods:A total of 128 mothers of neonates with neonatal septicemia admitted to a tertiary grade A hospital from September 2019 to September 2021 were selected as the case group,and 128 mothers of healthy neonates hospitalized in the same period were randomly selected as the control group.The vaginal microecology of the two groups in the third trimester was detected,the correlation between vaginal microecology disorder in the third trimester and neonatal septicemia was analyzed,and the evaluation value of vaginal microecology index on the risk of neonatal sepsis was tested.Results:The rate of vaginal microecological disorder in the case group(89.1%) was higher than that in the control group(79.7%),the positive rate of candida in case group(7.8%) was higher than that in control group(2.3%),the positive rate of G?bacilli(95.3%) was lower than that of the control group(100.0%),and the difference was statistically significant(P<0.05).Logistic regression analysis results showed that candida positivity in the third trimester was associated with neonatal sepsis(OR=3.721,P=0.045).Kendall correlation analysis showed that they were positively correlated(r=0.125,P=0.047).The ROC showed that the AUC of Candida positivity in the third trimester was 0.527 for the assessment of neonatal sepsis.Conclusion:Clinical attention should be paid to vaginal microecological disorder in the third trimester to prevent and reduce the occurrence of neonatal sepsis.
Keywords third trimester; vaginal microecology; neonates; septicemia; ROC; influencing factors; nursing
摘要 目的:分析孕晚期陰道微生态失调与新生儿败血症的相关性,为更好地防治新生儿败血症提供参考依据。方法:选取2019年9月—2021年9月某三级甲等医院收治的128例新生儿败血症患儿的母亲为病例组,随机选取同期住院的128例健康新生儿的母亲为对照组。检测两组孕晚期阴道微生态,分析孕晚期阴道微生态失调与新生儿败血症的相关性,并检验阴道微生态指标对新生儿败血症发生风险的评估价值。结果:病例组阴道微生态失调率(89.1%)高于对照组(79.7%);念珠菌阳性率(7.8%)高于对照组(2.3%);革兰阴性杆菌阳性率(95.3%)低于对照组(100.0%),差异均有统计学意义(P<0.05)。Logistic回归分析结果显示,孕晚期孕妇念珠菌阳性与新生儿败血症的发生相关(OR=3.721,P=0.045)。Kendall相关性分析结果显示,孕晚期孕妇念珠菌阳性与新生儿败血症的发生呈正相关(r=0.125,P=0.047)。受试者工作特征曲线(ROC)显示,孕晚期孕妇念珠菌阳性可用于评估新生儿败血症发生的ROC曲线下面积(AUC)为0.527。结论:临床应重视孕晚期阴道微生态失调,预防和降低新生儿败血症的发生。
关键词 孕晚期;阴道微生态;新生儿;败血症;受试者工作特征曲线;影响因素;护理
doi:10.12102/j.issn.1009-6493.2023.08.012
新生儿败血症是一种全身性细菌感染引起的疾病,是威胁新生儿生命的主要原因,其发病率高、病情进展快、临床表现早期无特异性,容易误诊或漏诊[1?2]。2015年全球疾病负担研究证实,新生儿败血症是新生儿死亡的第三大病因[3]。研究发现,孕晚期孕妇体内雌激素与孕激素水平过高,会导致孕妇体内糖原积聚及自身免疫功能下降,进一步导致新生儿败血症的发生[4]。阴道微生态失调和新生儿败血症关系密切,但二者的相关性并不明确。本研究通过分析孕晚期阴道微生态各指标与新生儿败血症的相关性,旨在为新生儿败血症的防治提供参考依据。
1 对象与方法
1.1 研究对象 选取2019年9月—2021年9月某三级甲等医院收治的128例新生儿败血症患儿的母亲为病例组,随机选取同期住院的128名健康新生儿的母亲为对照组。检测两组孕晚期阴道微生态,分析孕晚期阴道微生态失调与新生儿败血症的相关性。
1.2 纳入与排除标准 纳入标准:①孕周≥28周;②妊娠前无B族链球菌(GBS)定植;③健康单胎妊娠;④规律产检(可追踪其新生儿是否患败血症);⑤孕晚期均行阴道分泌物及GBS检查。排除标准:①合并心、肝、肾等内科疾病或具有自觉阴道炎症者;②检查前3 d有性生活史;③近2周有激素、抗生素(包括外阴及阴道用药)或免疫抑制剂使用史。
1.3 研究方法
1.3.1 阴道微生态 根据《阴道微生态评价的临床应用专家共识》[5],满足以下全部条件为阴道微生态正常,任何1项出现异常即可诊断为阴道微生态失调。①阴道菌群密集度为Ⅱ级或Ⅲ级;②多样性为Ⅱ级或Ⅲ级;③优势菌为乳酸杆菌;④阴道pH值为3.8~4.5。
1.3.2 新生儿败血症 新生儿败血症诊断参照《新生儿败血症诊断及治疗专家共识(2019年版)》[6]。128例新生儿败血症患儿中,有124例为早发败血症,4例为晚发败血症;10例血培养阳性。
1.3.3 统计学方法 采用SPSS 25.0软件进行数据统计分析,定性资料采用频数、百分比(%)描述,符合正态分布的定量资料采用均数±标准差(x±s)描述,单因素采用t检验、χ2检验和Kendall相关性分析;多因素采用Logistic回归分析;绘制受试者工作特征(ROC)曲线。
2 结果
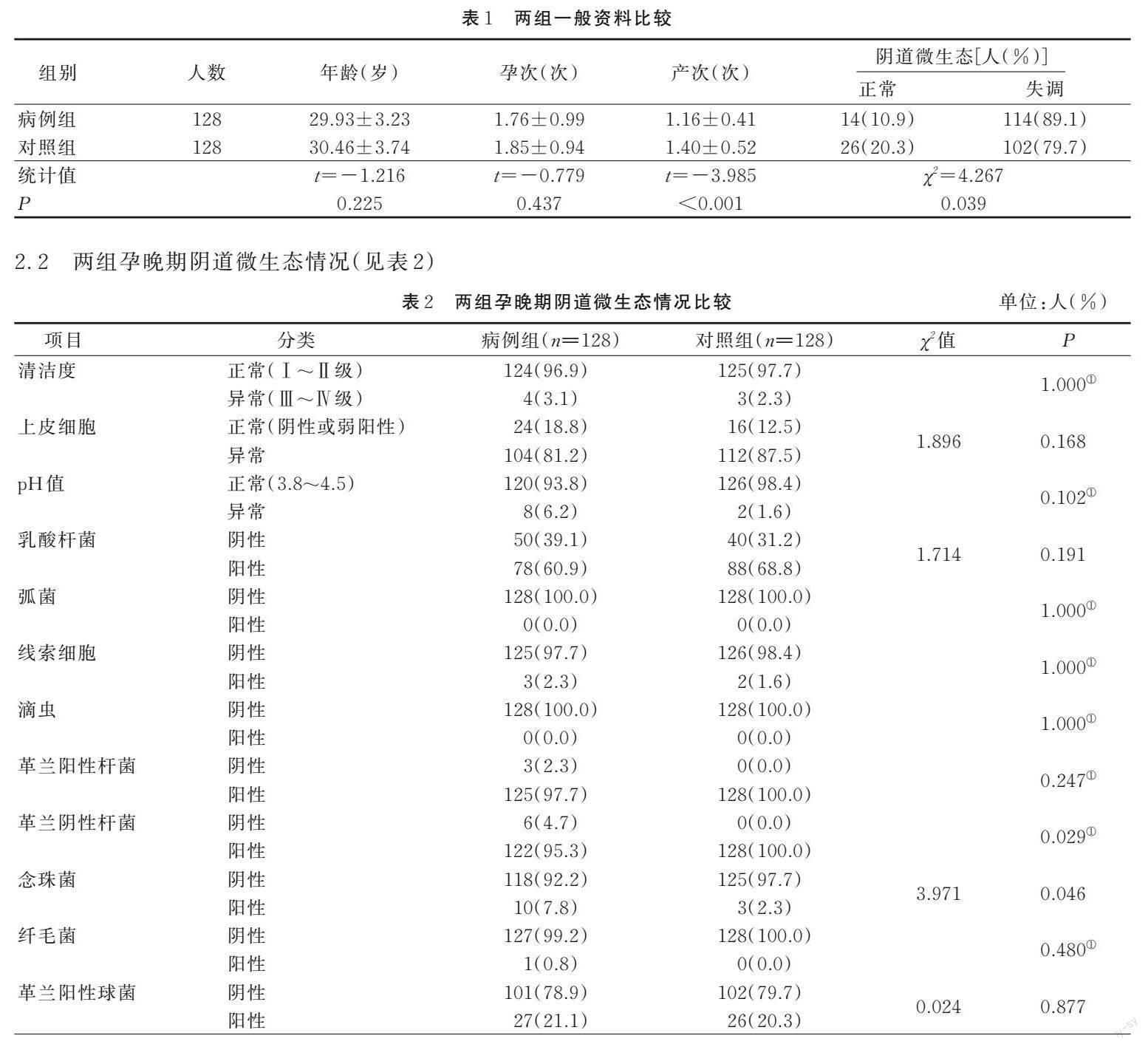
2.1 两组一般资料(见表1)
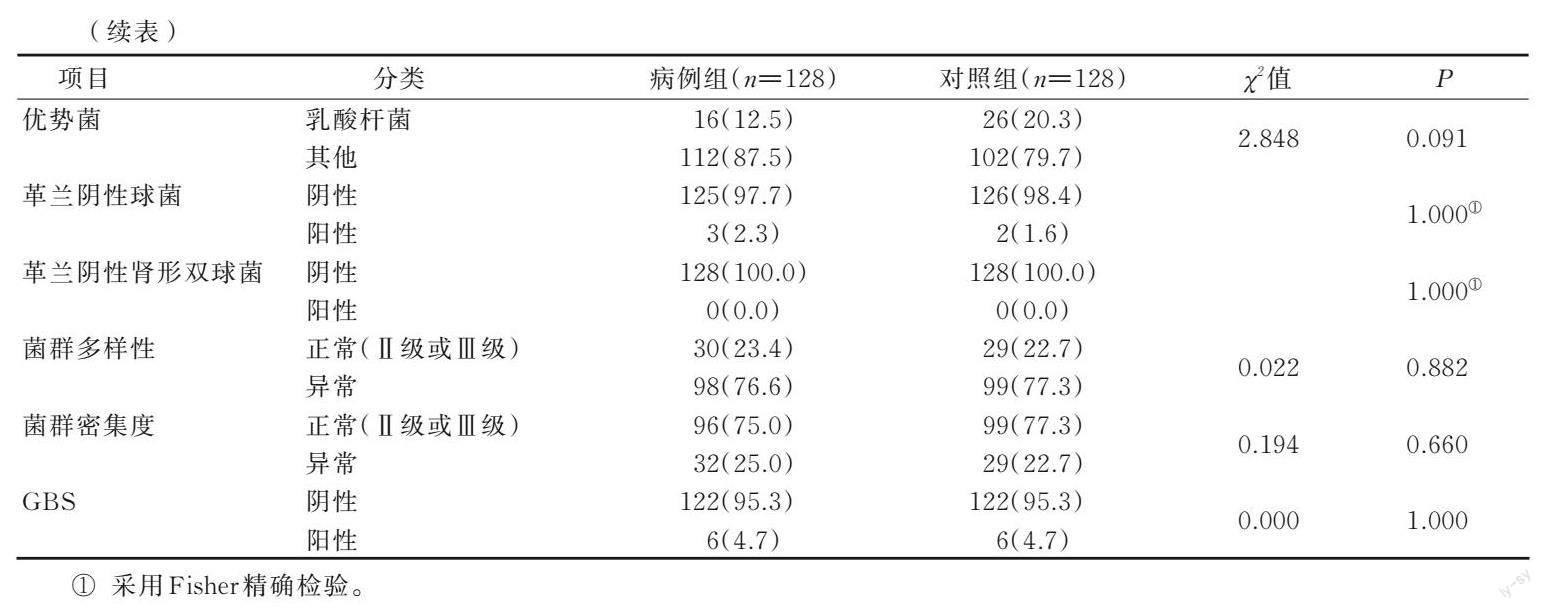
2.2 两组孕晚期阴道微生态情况(见表2)
2.3 孕晚期阴道微生态失调与新生儿败血症相关性分析 将是否患新生儿败血症作为因变量(新生儿败血症=1,健康新生儿=0),单因素分析中差异有统计学意义的念珠菌、革兰阴性杆菌作为自变量。采用Logistic回归分析结果显示,孕晚期孕妇念珠菌阳性与新生儿败血症的发生相关(OR=3.721,P=0.045)。Kendall相关性分析结果显示,孕晚期孕妇念珠菌阳性与新生儿败血症的发生呈正相关(r=0.125,P=0.047)。
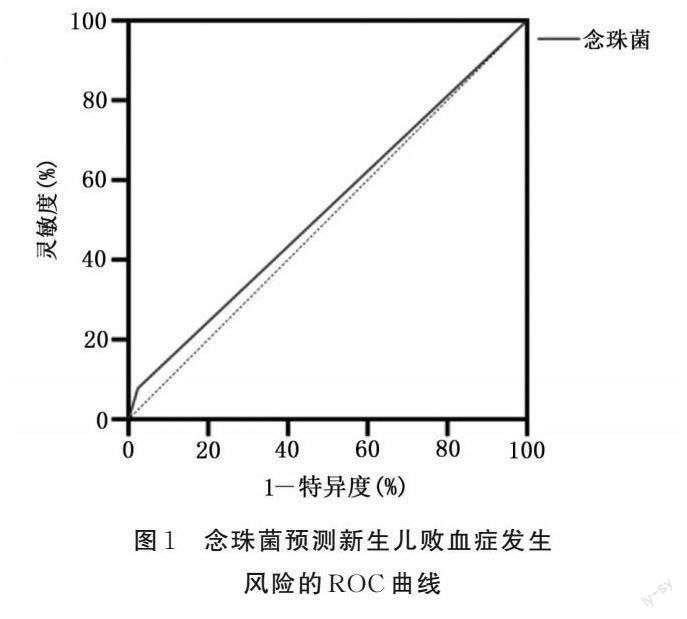
2.4 念珠菌预测新生儿败血症发生风险的ROC曲线 将新生儿是否患新生儿败血症作为状态变量,阴道微生态失调指标作为检验变量,绘制ROC曲线。结果显示,念珠菌阳性用于评估新生儿败血症发生的ROC曲线下面积(AUC)为0.527。
3 讨论
3.1 阴道微生态失调与新生儿败血症 新生儿败血症是危及新生儿生命健康的重要疾病。早期诊断和及时应用抗生素对新生儿败血症的防治至关重要[7]。孕晚期孕妇处于特殊的生理阶段,阴道微生态平衡容易受到破坏,孕晚期阴道微生态失调,病原体可自阴道或宫颈部上行,在胎膜或子宫等处繁殖[8?10];此外,孕晚期阴道微生态失调可通过胎盘将病原体传至胎儿或胎儿出生后因窒息吸入污染羊水,从而导致新生儿败血症的发生[11]。本研究中,病例组的阴道微生态失调率高于对照组,差异有统计学意义(P<0.05),证实了孕晚期孕妇阴道微生态失调与新生儿败血症的发生密切相关。
3.2 念珠菌与新生儿败血症 念珠菌是女性阴道一种常见的真菌性机会致病菌,当人体微生态环境紊乱或抵抗力降低时,可能会发生念珠菌感染[12]。本研究结果显示,孕晚期阴道念珠菌阳性与新生儿败血症呈正相关(r=0.125),与以往研究结果[13]一致。可能是由于念珠菌与GBS阴道定植有关,念珠菌是GBS阴道定植的独立危险因素[14?16]。GBS是新生儿败血症发生的主要原因,其检出率在新生儿败血症中有升高趋势[17?19]。本研究中孕晚期孕妇GBS阴道定植与新生儿败血症的发生差异无统计学意义(P>0.05),分析原因可能是在妊娠35~37周对所有孕妇进行规范的GBS筛查,预防性使用抗生素,降低了新生儿GBS感染的机会。
3.3 念珠菌预测新生儿败血症发生风险的价值 绘制ROC曲线发现,念珠菌阳性对新生儿败血症发生风险有评估价值,但预测价值较低(AUC=0.527)。新生儿一旦发生败血症其死亡率很高,尽管念珠菌阳性对新生儿败血症发生风险的评估价值较低,但是提前知晓与新生儿败血症发生的相关指标可以降低新生儿败血症的发生。因此,积极筛查孕晚期阴道微生态失调指标,及时采取针对性的治疗措施,可恢复孕妇阴道微生态平衡。此外,孕晚期孕妇应注意个人卫生,增强个人体质,提高机体免疫力,减少感染机会。
參考文献:
[1] PIMENTA J M,EBELING M,MONTAGUE T H,et al.A retrospective database analysis of neonatal morbidities to evaluate a composite endpoint for use in preterm labor clinical trials[J].AJP Reports,2018,8(1):e25-e32.
[2] 苗莉,李娟.脐血降钙素原对新生儿早发败血症诊断价值研究[J].中国实用儿科杂志,2017,32(8):623-626.
MIAO L,LI J.Diagnostic value of procalcitonin in umbilical cord blood for early neonatal septicemia[J].Chinese Journal of Practical Pediatrics,2017,32(8):623-626.
[3] PERIN J,MULICK A,YEUNG D,et al.Global,regional,and national causes of under-5 mortality in 2000-19:an updated systematic analysis with implications for the Sustainable Development Goals[J].The Lancet Child & Adolescent Health,2022,6(2):106-115.
[4] NURIEL-OHAYON M,NEUMAN H,KOREN O.Microbial changes during pregnancy,birth,and infancy[J].Frontiers in Microbiology,2016,7:1031.
[5] 中华医学会妇产科学分会感染性疾病协作组.阴道微生态评价的临床应用专家共识[J].中华妇产科杂志,2016,51(10):721-723.
Infectious Diseases Cooperation Group of Obstetrics and Gynecology Branch of Chinese Medical Association.Expert consensus on clinical application of vaginalmicroecological evaluation[J].Chinese Journal of Obstetrics and Gynecology,2016,51(10):721-723.
[6] 中华医学会儿科学分会新生儿学组,中国医师协会新生儿科医师分会感染专业委员会.新生儿败血症诊断及治疗专家共识(2019年版)[J].中华儿科杂志,2019,57(4):252-257.
The Subspecialty Group of Neonatology,the Society of Pediatric.Expert consensus on the diagnosis and management of neonatal sepsis(version 2019)[J].Chinese Journal of Pediatrics,2019,57(4):252-257.
[7] 徐俊芳,平莉莉,翟淑芬.不同新生儿败血症病原菌、耐药性及影响因素研究[J].中国妇幼健康研究,2022,33(8):6-11.
XU J F,PING L L,ZHAI S F.Study on pathogenic bacteria,drug resistance and influencing factors of different neonatal septicemia[J].Chinese Journal of Woman and Child Health Research,2022,33(8):6-11.
[8] KARAT C,MADHIVANAN P,KRUPP K,et al.The clinical and microbiological correlates of premature rupture of membranes[J].Indian Journal of Medical Microbiology,2006,24(4):283-285.
[9] WAITES K B,KATZ B,SCHELONKA R L.Mycoplasmas and ureaplasmas as neonatal pathogens[J].Clinical Microbiology Reviews,2005,18(4):757-789.
[10] ALLAIRE A,NATHAN L,MARTENS M G.Chlamydia trachomatis:management in pregnancy[J].Infectious Diseases in Obstetrics and Gynecology,1995,3(2):82-88.
[11] BULABULA A N H,DRAMOWSKI A,MEHTAR S.Transmission of multidrug-resistant gram-negative bacteria from colonized mothers to their infants:a systematic review and Meta-analysis[J].The Journal of Hospital Infection,2020,104(1):57-67.
[12] 谢印容.妇科炎症感染中微生物检验方法的临床效果观察与分析[J].中國医药科学,2020,10(17):173-175.
XIE Y R.Observation and analysis of the clinical effect of microbiological examination methods in gynecological inflammatory infection[J].China Medicine and Pharmacy,2020,10(17):173-175.
[13] 祁文瑾,石一复,许妙玲.妊娠期妇女阴道念珠菌对克霉唑、咪康唑、制霉菌素的敏感性研究[J].中华全科医师杂志,2007,6(5):280-283.
QI W J,SHI Y F,XU M L.In vitro susceptibility of vaginal Candida isolated from pregnant women to clotrimazole,miconazole and nystatin[J].Chinese Journal of General Practitioners,2007,6(5):280-283.
[14] PIDWILL G R,REGO S,JENKINSON H F,et al.Coassociation between group B streptococcus and Candida albicans promotes interactions with vaginal epithelium[J].Infection and Immunity,2018,86(4):e00669-e00617.
[15] MEYN L A,KROHN M A,HILLIER S L.Rectal colonization by group B streptococcus as a predictor of vaginal colonization[J].American Journal of Obstetrics and Gynecology,2009,201(1):76.e1-76.e7.
[16] COOLS P,JESPERS V,HARDY L,et al.A multi-country cross-sectional study of vaginal carriage of group B streptococci (GBS) and escherichia coli in resource-poor settings:prevalences and risk factors[J].PLoS One,2016,11(1):e0148052.
[17] SHARMILA V,JOSEPH N M,ARUN BABU T,et al.Genital tract group B streptococcal colonization in pregnant women:a South Indian perspective[J].Journal of Infection in Developing Countries,2011,5(8):592-595.
[18] SHANE A L,S?NCHEZ P J,STOLL B J.Neonatal sepsis[J].Lancet (London,England),2017,390(10104):1770-1780.
[19] GEYESUS T,MOGES F,ESHETIE S,et al.Bacterial etiologic agents causing neonatal sepsis and associated risk factors in Gondar,Northwest Ethiopia[J].BMC Pediatrics,2017,17(1):137.
(收稿日期:2022-11-17;修回日期:2023-03-22)
(本文編辑 曹妍)
