“Guidezilla” extension catheter combined with balloon technique for treating pulmonary artery stenosis caused by Takayasu arteritis
2023-03-06YifanWuJinziWangZiuiFuMinLiuWanmuXieXincaoTaoQiangHuangZenguoZai
Yifan Wu, Jinzi Wang, Ziui Fu, Min Liu,Wanmu Xie, Xincao Tao,g,*, Qiang Huang,**,Zenguo Zai,***
a National Center for Respiratory Medicine, Beijing, PR China
b State Key Laboratory of Respiratory Health and Multimorbidity, Beijing, PR China
c National Clinical Research Center for Respiratory Diseases, Beijing, PR China
d Institute of Respiratory Medicine, Chinese Academy of Medical Sciences, Beijing, PR China
e Center of Respiratory Medicine, China-Japan Friendship Hospital, Beijing, PR China
f Department of Pulmonary and Critical Care Medicine, The First Affiliated Hospital, Jiangxi Medical College, Nanchang University, Nanchang, China
g Chinese Academy of Medical Sciences Fuwai Hospital Center for Respiratory and Pulmonary Vascular Diseases, Beijing, 100037, China
h Department of Radiology, China-Japan Friendship Hospital, Beijing, China
i Graduate School of Peking Union Medical College, Chinese Academy of Medical Sciences, and Peking Union Medical College, Beijing, 100730, China
Keywords:
ABSTRACT Takayasu arteritis(TA)is a rare systemic vasculitis of the aorta and its primary branches,which usually occurs in young women.Due to its insidious onset and lack of specific symptoms,this disease can be easily misdiagnosed or missed.Approximately 50 % of the patients having TA with pulmonary artery involvement develop pulmonary hypertension(PH).The 3-year survival rate among patients with TA-related PH is lower than that among patients with TA alone.Early balloon pulmonary angioplasty (BPA) can improve the clinical symptoms and survival of patients with stable TA.To the best of our knowledge, this is the first case reported in the English literature in which a“Guidezilla”catheter was used during BPA to treat stenosis and occlusion of the pulmonary artery caused by Takayasu arteritis (TA).
1.Introduction
Takayasu arteritis(TA)is a chronic,nonspecific arterial inflammatory disease that mainly involves the aorta and its branches,descending aorta,abdominal aorta,and renal artery.The pulmonary and coronary arteries may also be involved.1TA with pulmonary artery involvement can lead to stenosis and occlusion of the pulmonary artery,leading to pulmonary hypertension (PH).Interventional therapy can be administered if the conservative treatment is not effective.2However, the most difficult aspect of balloon pulmonary angioplasty (BPA) is passage through the lesion, which involves the selection of a guidewire and catheter.This report presents a detailed case of BPA for TA-related pulmonary artery stenosis.
2.Case report
A 29-year-old woman complained of “shortness of breath for 8 months after activity, accompanied by coughing and hemoptysis for 4 months.”Eight months prior,the patient experienced chest tightness and breathlessness after activity,especially after climbing stairs to the fourth floor, accompanied by nonproductive cough, fever, hemoptysis, chest pain, and syncope.Four months prior, hemoptysis, a new clinical symptom, appeared.The patient was admitted to a local hospital.The erythrocyte sedimentation rate (ESR) was 91 mm/h.The pulmonary systolic pressure was estimated to be 58 mmHg on echocardiography.Computed tomographic pulmonary angiography(CTPA)showed stenosis and occlusion of the left pulmonary artery and multiple lesions in the left lung,which were considered to be pulmonary infarctions.The results of the chest magnetic resonance imaging (MRI) examination (enhanced scans) were consistent with those of CTPA.Positron emission tomography(PET)-CT showed diffuse thickening of the ascending aorta,thoracic aorta, and pulmonary artery, and increased metabolic activity, suggesting the possibility of TA.Multiple subpleural plaques in the left lung were considered pulmonary infarctions.After standard treatment with methylprednisolone and cyclophosphamide,the clinical symptoms improved,but dyspnea persisted.
The patient subsequently visited our hospital for further treatment.Vital signs revealed a temperature of 36.5°C, heart rate of 80 beats per minute, respiratory rate of 21 breaths per minute, and left and right upper limb blood pressures of 112/55 and 119/70 mmHg,respectively.No cyanosis on the lips or jugular venous distention was observed.Auscultation revealed P2 > A2 in the pulmonary auscultation area and obvious vascular murmurs in the left common carotid and left subclavian arteries.Laboratory examination showed a C-reactive protein level of 5.85 mg/dL and a normal erythrocyte sedimentation rate.A review of CTPA suggested left pulmonary artery stenosis and occlusion, and left lung infarction (Fig.1).No obvious changes were observed compared with the previous CTPA.Peripheral blood tests, chest MRI, and other related examinations confirmed that the patient had no signs of active inflammation.The results of right-heart catheterization (RHC) are presented in Table 1.Pulmonary angiography revealed severe pulmonary stenosis in the basal segment of the right lung and complete pulmonary occlusion in the medial anterior basal segment and left pulmonary artery(Fig.2).
After a multidisciplinary consultation and full communication with the patient,BPA was performed.An MP JR4 6-F guiding catheter(Cordis,Bridgewater, NJ, USA) was inserted into the left pulmonary artery through an 80-cm 8-F vascular sheath (Flexor; Cook Medical, Bloomington,IN,USA)to the target vessel.Subsequently,a 0.014-inch guide wire(Sion;Asahi Intecc,Seto,Japan)was used to pass the anterior basal segment of the right pulmonary artery, then balloon dilation catheters(3.5 mm × 20 mm and 4.5 mm × 20 mm; IKAZUCHI PAD; Kaneka,Osaka, Japan) were advanced over the guidewire for the dilatation.However, significant challenges appeared when attempting to achieve complete occlusion of the left pulmonary artery.The guidewire and balloon dilation catheter could not pass through the occlusion(Fig.3).A microcatheter(Corsair;Asahi Intecc)was attempted but failed(Fig.4).A 0.014-inch guidewire(Fielder XT;Asahi Intecc)was used again without success.Finally, an extension catheter (Guidezilla; Boston Scientific,Marlborough, MA, USA) was applied, since it can provide a strong supporting force.A new 0.014-inch guidewire (Sion; Asahi Intecc) was passed through the lesion successfully with the support of the extension catheter(Fig.5).Balloon dilatation catheters(1.5 mm×15 mm,2.5 mm× 20 mm, and 4.0 mm × 20 mm; IKAZUCHI PAD; Kaneka) were subsequently introduced to dilate the lesion, and the blood flow improved from grade 0 to grade III (Fig.6).

Fig.1.(A) Computer tomography pulmonary angiography (CTPA) showing left pulmonary artery stenosis and occlusion (white arrow), (B) and left lung infarction(white arrow).

Table 1 The results of right heart catheter in our hospital.
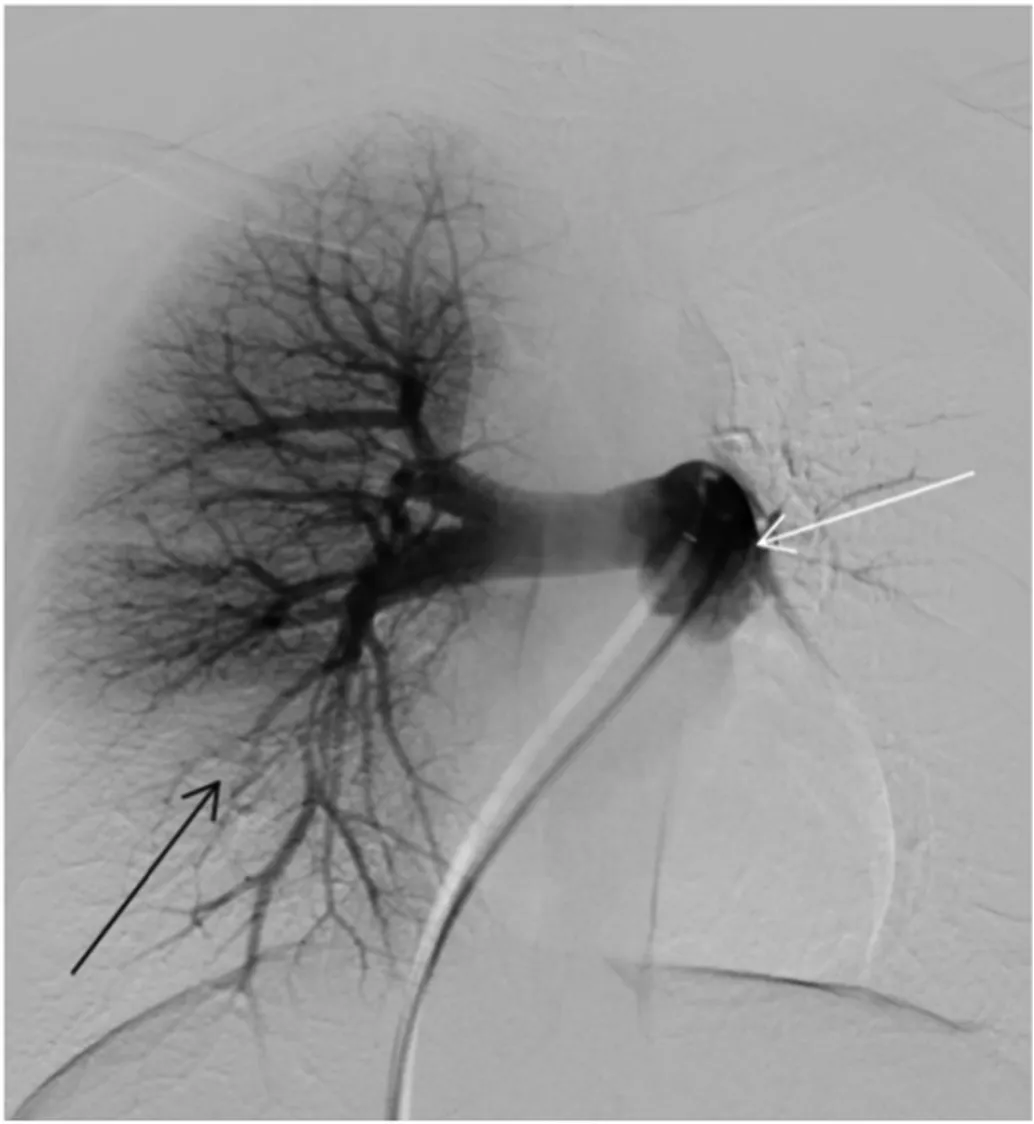
Fig.2.Pulmonary angiography revealing complete pulmonary occlusion in the medial anterior basal segment(black arrow),and complete pulmonary occlusion in the left pulmonary artery (white arrow).
After BPA, the patient's shortness of breath improved, and 6 months later, an RHC review showed that the mean pulmonary artery pressure(mPAP)had decreased to 20 mmHg.We conducted several BPA sessions to deal with other pulmonary arteries,which improved her quality of life.However, in March 2023, she was infected with COVID-19 and her symptoms worsened.After discussing with her, pulmonary artery stenting was performed, mPAP decreased to 18 mmHg and pulmonary vascular resistance decreased from 1.73 to 1.15 Wood units.
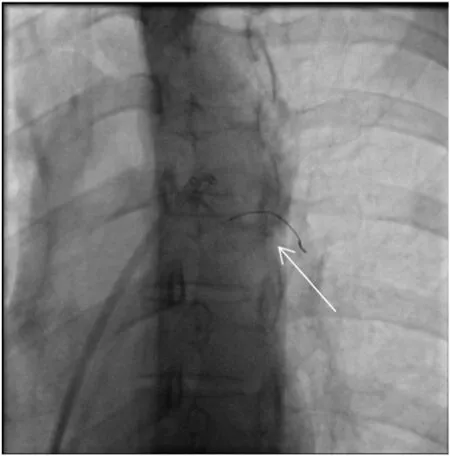
Fig.3.A 0.014-inch Sion guidewire combined with balloon dilation catheter is unable to pass through the occlusion (white arrow).

Fig.4.The Corsair microcatheter (white arrow) shown in pulmonary angiography.
3.Discussion
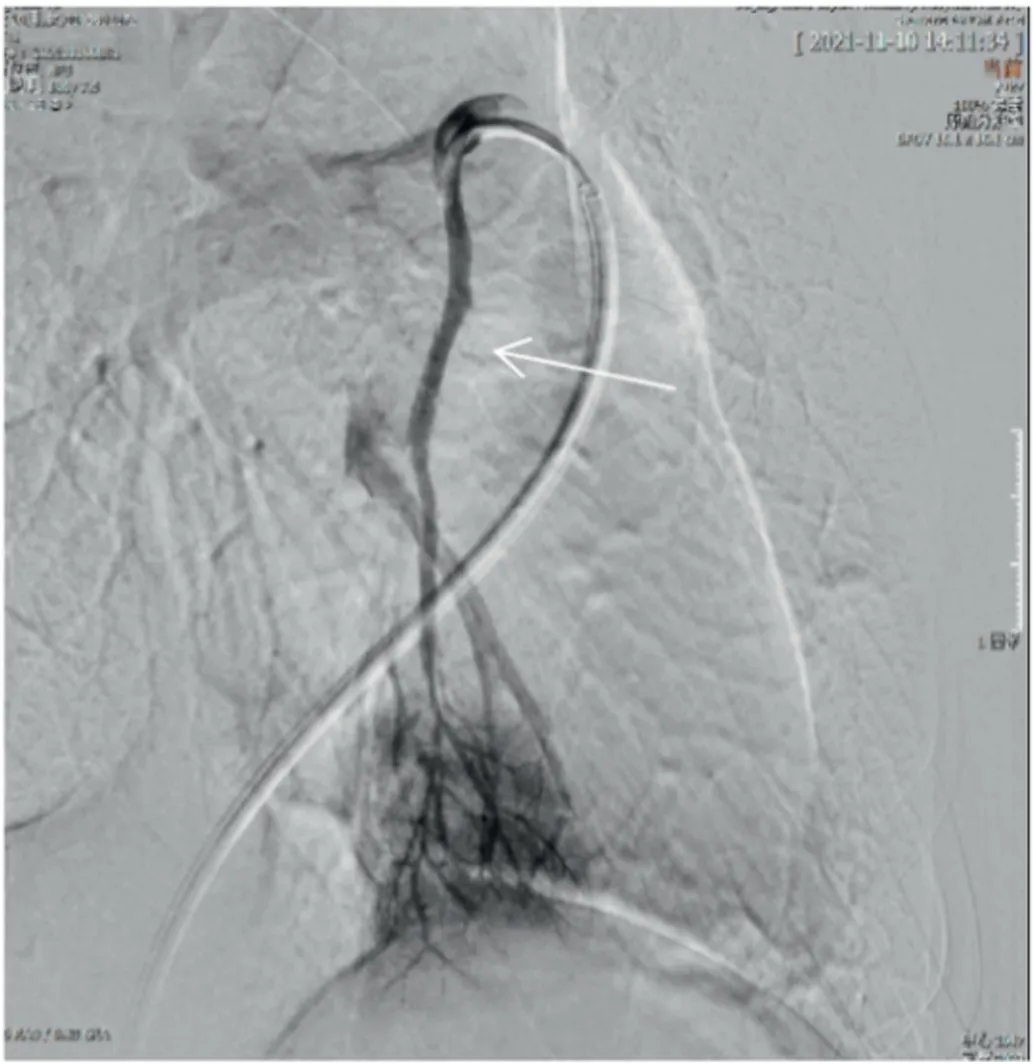
Fig.6.The blood flow increases to grade III.
TA is a rare systemic vasculitis of the aorta and its primary branches,which occurs more often in young women.3,4TA-related pulmonary artery involvement occurs in approximately 35 % of all cases.3Approximately 50 % of the patients having TA with pulmonary involvement develop PH.The insidious onset and lack of specific symptoms can lead to misdiagnosis and delayed diagnosis, causing difficulties in treatment.3,4The 3-year survival rate among patients with TA-related PH was lower than that among those with TA alone.4The primary cause of death in patients with TA-related PH is right heart failure.2Early treatment,including drug treatment and interventional therapy, can improve clinical symptoms and patient survival.Interventional therapy is typically administered after medication failure or when clinical symptoms persist.
Although BPA has been reported in patients with TA-related PH and proven to improve patient survival, some problems persist.5,6The branches of the pulmonary artery have a large anatomical angle, which brings great difficulty and challenges during BPA because the catheter and guidewire have difficulty passing through the lesion.Chronic thromboembolic pulmonary hypertension(CTEPH)is classified as group 4 PH and is characterized pathologically by organized thromboembolic material and altered vascular remodeling, leading to right heart failure.BPA has evolved into an important component of CTEPH treatment;however, during the surgical procedure, there will be cases where the guidewire cannot pass through the lesion.The Guidezilla extension catheter is a single-chamber rapid-exchange catheter compatible with the 6-F guide catheter, which consists of 120-cm- and 25-cm-long special wire-woven nets and a polymer guidepipe,with a total length of 145 cm.The inner and outer diameters are 1.45 mm and 1.68 mm,respectively.The outer surface is coated with a hydrophilic material and the pushrod is connected to the guidepipe segment in an embedded polymer-wrapped structure.Its structure offers some benefits: it can provide additional support and coaxiality to the lesion site,its inner diameter is large,it can stably transport instruments, and the hydrophilic coating on its surface reduces friction.
Guidezilla catheters with a strong supporting force are usually used in complex coronary interventions and have been proven to have good safety and efficacy.7The extension catheter is reportedly safe and effective in patients with CTEPH, consistent with our experience.8Similar to complex lesions in CTEPH,treating a total occlusion in TA with pulmonary artery involvement remains a challenge.Drawing on our experience with CTEPH,we felt that an extended catheter could also be used in TA as a strong supporting force.For patients with pulmonary vessel tortuosity or occlusion due to TA,the Guidezilla extended catheter can be used.To the best of our knowledge,this is the first case in which a Guidezilla catheter was used during BPA to treat TA-pulmonary involvement.We believe that this may provide experience for pulmonary vascular interventionists.Further investigation on the application of the Guidezilla catheter in the pulmonary vasculature is warranted to determine its clinical value.
Authors’ contributions
Zhenguo Zhai and Xincao Tao diagnosed and treated the patient.Yifan Wu, Jinzhi Wang and Zhihui Fu collected the clinical information and completed the manuscript.Qiang Huang, Wanmu Xie and Min Liu revised the manuscript.All authors approved the final version.
Funding
This study was supported by funds from the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2021-I2M-1–049) and National High Level Hospital Clinical Research Funding(2022-NHLHCRF-LX-01-0203).
Ethical approval
The study was approved by the ethics committee of China-Japan Friendship Hospital.All clinical practices and observations were conducted in accordance with the Declaration of Helsinki.
Patient consent for publication
Written informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article.
Declaration of competing interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
杂志排行
Journal of Interventional Medicine的其它文章
- Mechanisms and therapeutic strategies to combat the recurrence and progression of hepatocellular carcinoma after thermal ablation
- Overview of peripheral arteriovenous malformations: From diagnosis to treatment methods
- Embolization of brain arteriovenous malformations with squid co-polymer embolic material: Initial experience
- A novel cerebrovascular drug-coated balloon catheter for treating symptomatic intracranial atherosclerotic stenosis lesions:Study protocol for a prospective, multicenter, single-arm, target-value clinical trial
- Combination of transarterial radioembolization with atezolizumab and bevacizumab for intermediate and advanced staged hepatocellular carcinoma: A preliminary report of safety and feasibility
- Argon-helium cryoablation treatment of undifferentiated pleomorphic sarcoma of the thyroid: A case report and literature review
