Prediction of effective percutaneous transhepatic biliary drainage in patients with hepatocellular carcinoma: A multi-central retrospective study☆
2023-01-09HonWnYitoMoChunninZhnXiojunHuBinChnLuwnMuShuyiWnYinLinZhnwnXinMinshnHun
Hon Wn ,Yito Mo ,Chunnin Zhn ,Xiojun Hu ,Bin Chn ,Luwn Mu ,Shuyi Wn ,Yin Lin ,Zhnwn Xin ,*,Minshn Hun ,*
a Department of Interventional Radiology,The Third Affiliated Hospital of Sun Yat-sen University,Guangzhou,Guangdong,China
b Department of Radiology,Xiangya Hospital,Central South University,Changsha,Hunan,China
c Department of Oncology,Maoming People's Hospital,Maoming,Guangdong,China
d Center for Interventional Medicine,The Fifth Affiliated Hospital of Sun Yat-sen University,Zhuhai,Guangdong,China
e Department of Interventional Radiology,The First Affiliated Hospital of Sun Yat-sen University,Guangzhou,Guangdong,China
f Department of Rheumatology,The First Affiliated Hospital of Sun Yat-sen University,Guangzhou,Guangdong,China
g Cardiology Department,The First Affiliated Hospital of Sun Yat-sen University,Guangzhou,Guangdong,China
Keywords:Hepatocellular carcinoma (HCC)Percutaneous transhepatic biliary drainage(PTBD)Cholestasis Bilirubin Platelet count Nomograms Predictive model
ABSTRACT Background and aim: Percutaneous transhepatic biliary drainage (PTBD) does not always lead to a reduction in serum total bilirubin (TBil) level in patients with hepatocellular carcinoma and obstructive jaundice.We aimed to develop a model for pre-PTBD prediction of post-procedural TBil decrease in these patients.Materials and methods: Retrospective database searches were conducted at four teaching hospitals(reference period:January 2010 to December 2018),and baseline characteristics of eligible patients were extracted.Any decrease in TBil after PTBD and the lowest level of TBil post-PTBD<5 mg/dL,3 mg/dL,and 2 mg/dL were each taken as the standard of effectiveness for computation of its own predictive nomogram.For data dimension decrease and feature selection,the least absolute shrinkage and selection operator (LASSO) regression model was used.A multivariable logistic regression analysis was used to develop nomograms.Each nomogram's performance was internally evaluated for its calibration,discriminative ability,and clinical usefulness.Results: Included in the study were 138 patients.The model for end-stage liver disease (MELD) score,platelet count,and portal vein thrombosis (PVT) were predictors in the nomogram for any decrease in TBil;international normalized ratio (INR),MELD score,platelet count,and PVT were predictors for a decrease to <5 mg/dL;MELD score,cholinesterase level (CHE),platelet count,and PVT were predictors for a decrease to<3 mg/dL;and MELD score,CHE,platelet count,and pre-albumin level were predictors for a decrease to <2 mg/dL.The clinical value of the nomograms was proven by decision curve analysis.Conclusions: These models may help inform clinical decision making for performing PTBD procedures.
1.Introduction
Hepatitis B virus (HBV) infection,which is more common in Asia,is one of the primary risk factors for the development of HCC.1-3HCC is one of the most lethal tumors.1The prognosis of advanced stage disease,which is mostly influenced by locally invasive state or associated liver function damage,is especially poor,and only systematic or palliative treatments could be recommended.2,3Obstructive jaundice is an uncommon but complicated challenge for patients with HCC and underlying HBVrelated cirrhosis.4-9On the one hand,its rarity (reported prevalence rate of obstructive jaundice in HCC patients ranged from 0.278% to 5.630%,averaging at 1.250%) has limited the accumulation of high-quality evidence,which has restricted our capacity to create informed predictions and recommendations.2-17On the other hand,some medical professionals believed it to be a risky condition signifying a locally advanced stage,similar to portal vein tumor thrombosis,and that if it was not treated properly,there was a risk of cholangitis,hemobilia,and even hepatic failure;also,there was a factor of compromised liver function.4-17
It has been demonstrated that the alleviation of obstructive jaundice can improve survival and quality of life for these patients.4-17However,effective lowering of serum level of total bilirubin (TBil) is achieved in only a fraction of well-drained patients (Supplementary Table 1),4,6,7,9,11,12,17-21and because this condition is relatively uncommon,4-6,8,10,13-16the correlates of the outcomes of decompression are not well characterized.4-25Percutaneous transhepatic biliary drainage (PTBD) is one of the main methods of decompression,which is an invasive procedure with potential dangers as well as inconveniences and discomforts inherent to long-term drainage.18-25Therefore,identification of the factors that may help predict the effectiveness of PTBD assessed by post-procedural TBil level is of much clinical relevance.
This study only included patients with HBV-related cirrhosis since HCC occurring in these patients showed more aggressive behavior.1-3,26Moreover,this disease background characteristic would be a potentially significant confounder that required further research.We retrospectively reviewed clinical data of patients who were well drained using PTBD at four teaching hospitals and attempted to develop models to predict whether TBil would be reduced at all or reduced to less than 5 mg/dL,3 mg/dL,or 2 mg/dL,4 weeks after PTBD.22,24These thresholds have been commonly used as endpoints in similar studies.4-25
2.Methods
2.1.Ethical approval
This retrospective study conformed to the ethical principles enshrined in the 1964 Declaration of Helsinki and its later amendments.The study protocol was approved by the institutional review board of the Third Affiliated Hospital of Sun Yat-sen University,the First Affiliated Hospital of Sun Yat-sen University,the Fifth Affiliated Hospital of Sun Yat-sen University,and Maoming People's Hospital.The requirement for informed consent was waived.
2.2.Patients
We searched for patients with HCC who underwent PTBD for obstructive jaundice between January 1,2010,and December 31,2018,in the databases of the Third Affiliated Hospital of Sun Yat-sen University,the First Affiliated Hospital of Sun Yat-sen University,the Fifth Affiliated Hospital of Sun Yat-sen University,and Maoming People's Hospital.
The inclusion criteria to relieve obstructive jaundice were as follows: (i) diagnosis of HCC based on histologic or noninvasive criteria defined by major clinical guidelines with a history of HBVrelated cirrhosis;2,3(ii) serum TBil level >3 mg/dL within 3 days prior to the PTBD procedure;(iii) typical signs of biliary tract obstruction in computed tomography (CT),magnetic resonance imaging (MRI),or percutaneous transhepatic cholangiography images;and (iv) indication for PTBD.4,12,15,17The exclusion criteria were as follows: (i) improperly drained patients,defined as less than 75% (determined by at least two interventional radiologists upon review of the cholangiogram,preprocedural and follow-up imaging) of remaining liver segments drained or performance of a secondary drainage-related procedure after the first week postprimary PTBD procedure;2,23(ii) death within the first postprocedural week or lost to follow-up after discharge;and (iii) history of excessive alcohol consumption,hepatitis C infection,or nonalcoholic steatohepatitis.Considering the retrospective multicentral nature of this study,the first exclusion criterion was applied as a post hoc quality control measure.Before conducting further analysis,we evaluated the number of drainage catheters inserted for each patient across centers to confirm that no significant difference was observed pertaining procedural techniques among patients enrolled from different sites.Preprocedural total serum bilirubin,international normalized ratio (INR),model for end-stage liver disease(MELD)score,and platelet count of patients from each hospital were also compared,and there were no statistically significant differences observed.
2.3.Procedures
Routine pre-PTBD blood indices were obtained from all four participating hospitals.Preprocedural CT/MRI images were reviewed by at least two radiologists,and morphological features of the HCC were determined (Supplementary Table 2).2-25The interval between clinical onset of jaundice and PTBD was recorded as time to treatment (in days),as previously reported.4-17
PTBD procedures were performed by interventional radiologists using standard techniques.4,9The right or left approach was determined based on the location and the extent of the bile duct obstruction by the tumor as well as the feasibility of each approach.
2.4.Outcome
Follow-up medical records were reviewed.Morbidity,mortality,and laboratory data within a month after PTBD were recorded.Effective drainage was defined separately for calculation of the respective nomogram as (i) any decrease in TBil level,(ii) TBil reduced to<5 mg/dL,(iii) 3 mg/dL,or (iv)2 mg/dL.Follow-up test results obtained 4 weeks after the PTBD procedure,4,7,11,12,15,17and the lowest TBil level before death or before subsequent tests revealed a steady increase in TBil which were recorded and compared with the efficacy standards.The first follow-up TBil test result that was lower than 2 mg/dL was recorded as the lowest post-procedural TBil.
2.5.Statistical analysis
Statistical analysis was conducted with R software (version 3.5.1;http://www.rproject.org).Two-sidedP-values <0.05 were considered indicative of statistical significance.The least absolute shrinkage and selection operator(LASSO)method,which has been reported to be suitable for the regression of high-dimensional data,was used to select the most useful predictive characteristics from the data set.27Multivariable logistic regression analysis was then started,and the variables that survived the LASSO model according to the 1-standard error selection criterion were further tested by backward stepwise selection using the likelihood ratio test with Akaike's information criterion as the stopping rule.With the Hosmer-Lemeshow test,calibration curves were plotted to evaluate the accuracy of the predictive function.Discrimination performance of the prediction model was assessed using area under the curve of receiver operating characteristic curve (AUROC).Decision curve analysis (DCA) was conducted to determine the practicality of the prediction model by quantifying the probability of net benefits at different thresholds.27We also conducted univariate analysis on the baseline data.Continuous variables and categorical grades were presented as mean±standard deviation;dichotomous variables were expressed as frequencies and compared using theChi-squared test or the Fisher exact test.P-value <0.05 was considered indicative of statistical significance.A commercially available software package (SPSS 19.0 for Windows,IBM,Chicago,IL,USA)was used for univariate analyses.
3.Results
3.1.Demographics and univariate analysis
The final population included for analysis consisted of 138 patients (Fig.1).In six patients,imaging evidence indicated obstruction caused by external compression,while all other patients showed evidence of in-growth tumor in the biliary system.The effective rate was 73.19%(101 in 138 patients)when determined by any decrease of TBil 4 weeks after PTBD and 44.70% when determined by lowest recorded post-procedural TBil<5 mg/dL(59 in 132 patients whose preprocedural TBil levels were >5 mg/dL).The effective rate was 41.30%when the standard was 3 mg/dL(57 in 138 patients),and 31.88% when the standard was 2 mg/dL (44 in 138 patients).Success rates were comparable among different institutions(Supplementary Table 3).Among the included patients,6 had pre-PTBD TBil levels <5 mg/dL;they all showed lowest postprocedural TBil levels of <3 mg/dL,while two of them did not reach the 2 mg/dL standard.They were excluded from the 5 mg/dL endpoint analysis.Three patients died on the 10th,12th,and 17th day,respectively,with multiple organ failure being the cause of death in two patients and variceal hemorrhage in one patient.The mean period to achieve the lowest level of TBil by patients in the 5 mg/dL,3 mg/dL,and 2 mg/dL groups was 66.2 ± 39.5 days.Supplementary Table 4 summarizes the clinical characteristics of patients and the results of univariate analysis.
3.2.Feature selection
Based on the feature data of the 138 patients in our cohort that had non-zero coefficients in the LASSO logistic regression model,46 features were reduced to 5 potential predictors when looking at any decrease,to 4 potential predictors when the endpoint was set at<5 mg/dL,to 6 potential predictors for endpoint of 3 mg/dL,and to 5 potential predictors for endpoint of 2 mg/dL (Supplementary Fig.1).The indirect bilirubin/direct bilirubin ratio,time to treatment,MELD score,platelet count,and portal vein thrombosis(PVT)were selected as potential risk factors for any decrease in TBil.International normalized ratio(INR),MELD score,platelet count,and PVT were selected as potential risk factors for a decrease in TBil to<5 mg/dL.INR,Child-Pugh score,MELD score,cholinesterase level(CHE),platelet count,and PVT were selected as potential risk factors for a decrease to 3 mg/dL,while INR,MELD score,CHE,prealbumin level,and platelet count were selected as potential risk factors for a decrease to 2 mg/dL.
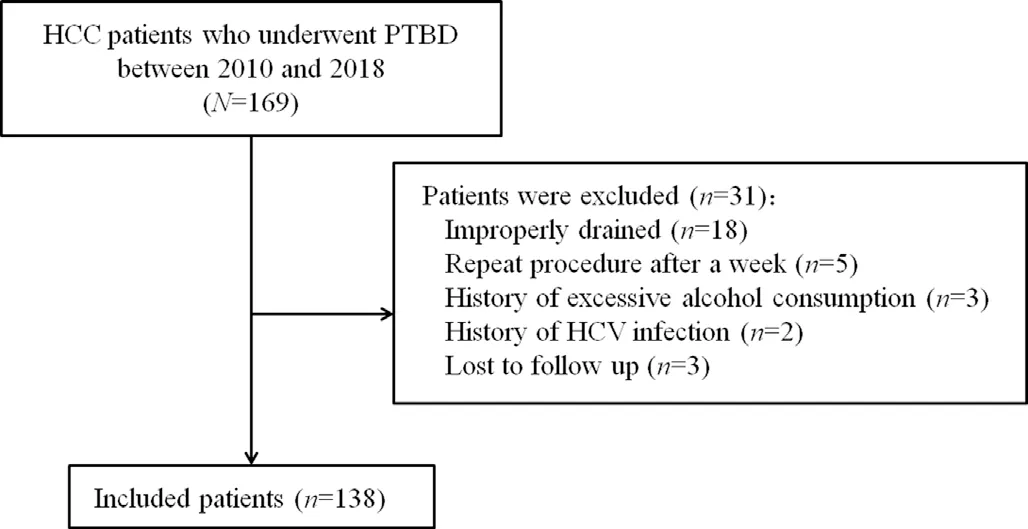
Fig.1.Patient flow diagram.
3.3.Development of a prediction model
Multivariable logistic regression analysis was started with the potential predictors.During the backward stepwise selection process,the indirect bilirubin/direct bilirubin ratio was eliminated from the model for any decrease in TBil,while the remaining four predictors,i.e.,time to treatment(β value,-0.0475),MELD score(β value,-0.1212),platelet count (β value,0.0122),and PVT (β value,-0.5382) were retained as the predictors.INR and Child-Pugh scores were eliminated using the same process,and the remaining four predictors,i.e.,MELD score (β value,-0.1587),CHE (β value,0.0003),platelet count (β value,0.0063),and PVT (β value,-0.4306) were retained as the predictors in the model for a decrease in TBil to 3 mg/dL.INR was eliminated,and CHE(β value,0.0003),MELD score (β value,-0.1011),platelet count (β value,0.0051),and pre-albumin level (β value,0.0118) were retained as predictors in the model for a decrease in TBil to 2 mg/dL.INR (β value,-2.5965),MELD score (β value,-0.1380),platelet count (β value,0.0081),and PVT (β value,-0.4632) were retained as predictors in the model for a decrease in TBil to<5 mg/dL.Models were presented as nomograms (Table 1,Fig.2).

Table 1Independent predictors included in the four nomograms for effective PTBD in patients with HCC with obstructive jaundice.
3.4.Apparent performance and internal validation of the nomogram
We used data of the same group of patients as the internal validation data set.The calibration curves of the nomograms for the effectiveness of PTBD,as measured by different standards,showed that good agreement between prediction and observation in our cohort (Fig.3).The Hosmer-Lemeshow test yielded statistically non-significant(P=0.891 for any decrease model,0.634 for<5 mg/dL,P=0.956 for 3 mg/dL,and 0.977 for 2 mg/dL TBil),which suggested that there was little departure from perfect fit.The Cindex for the prediction nomogram for any decrease in TBil was 0.847(95%confidence interval(CI),0.775-0.919).The C-indices for<5 mg/dL,3 mg/dL,and 2 mg/dL endpoints were 0.843 (95% CI,0.777-0.909),0.818 (95% CI,0.746-0.890),and 0.776 (95% CI,0.691-0.861),respectively (Fig.3).On ROC curve analysis,the optimal cut-off values were 0.786 for any decrease in TBil,0.602 for<5 mg/dL,0.557 for 3 mg/dL,and 0.301 for 2 mg/dL(Supplementary Fig.2).
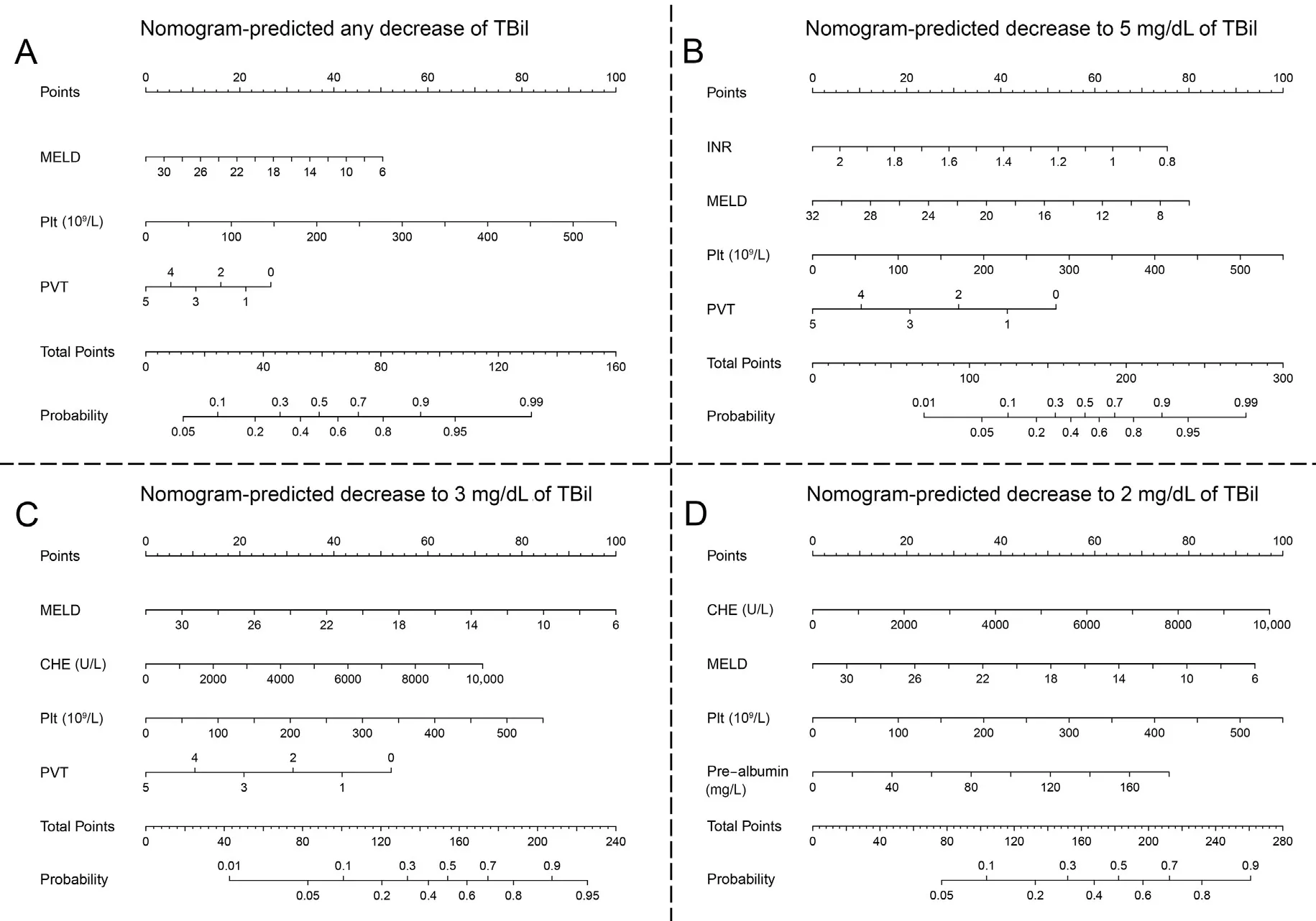
Fig.2.Nomograms for predicting the effectiveness of PTBD.The incorporated variables for the nomograms predicting any decrease(A),decrease to a lowest level of 5 mg/dL(B),and decrease to 3 mg/dL(C)and to 2 mg/dL(D)of TBil are shown,respectively,with three variables ultimately selected in each model.Abbreviations:CHE,cholinesterase level;INR,international normalized ratio;MELD,model for end-stage liver disease;Plt,platelet;PTBD,percutaneous transhepatic biliary drainage;PVT,portal vein thrombosis;TBil,total bilirubin.
3.5.Clinical use
Fig.4 shows the DCA graphs for the nomogram.The decision curves showed that when the threshold probability of a patient and doctor is 20% and 95%,respectively,implying that if a patient or doctor is willing to undergo/perform PTBD if any prediction model showed >20% and <95% chance of any decrease,using the nomogram to predict effectiveness would benefit the patient more than using either the treat-all-patients scheme or the treat-none scheme.The threshold pairs were 20% and 90% for <5 mg/dL,20%and 95% for 3 mg/dL,and 20% and 85%for 2 mg/dL,respectively.
4.Discussion
Hepatic parenchymal injury in patients with HCC also contributes to obstructive jaundice.6,7,11,13The effective rates in our cohort were 73.19%,44.70%,41.30%,and 31.88%,respectively,for any decrease in TBil,decrease to <5 mg/dL,3 mg/dL,or 2 mg/dL endpoints.These outcomes were comparable to previous reports(Supplementary Table 1).4,6,7,9,11,12,17-21However,clinical success rates were higher in all patients with malignant(excluding HCC or not) obstructive jaundice (Supplementary Table 1),4,6,7,9,11,12,17-21which was likely attributable to cirrhosis.
Our study selected 4 weeks as the time of evaluation because it was a common practice.PTBD may be preferred for patients and physicians who are willing to wait longer if the prediction models returned negative for their expected goal but positive for a less demanding target.However,we would remain conservative toward drainage if the prospect of any decrease after 4 weeks of adequate drainage was not satisfactory.
MELD score and platelet level appeared in all four nomograms.They should both be reflecting the effect of cirrhosis.2,3,17,18,28-32It was once found that after effective drainage,all laboratory parameters except platelet count improved.4This implied that platelet count might be correlated to chronic cirrhosis independently from recent jaundice because independence could explain its survival from predictor selection algorithm.Predictive values of other liver-function-related variables were not as reliable as MELD score and platelet.6,11,12,16,33
It is commonly accepted that PVT has an impact on patients with icteric-type HCC.2-17It was not in the prediction model for 2 mg/dL though.PVT was associated with the 2 mg/dL goal,and the trend of fewer patients with extensive PVT in more rigorous TBil target groups was conservative.However,the drop was more substantial from any decrease group to the <5 mg/dL group (Supplementary Table 4).It was indicated that PVT was a more effective negative predictive factor.Extensive PVT predicts a higher probability of no alleviation after PTBD.While all patients who reached the 5 mg/dL goal 4 weeks after PTBD could be able to achieve better TBil target,some might need more time,which correlated more closely with liver function and not PVT.It echoed the practice of some oncologists to prescribe anti-tumor treatment after achieving 5 mg/dL.
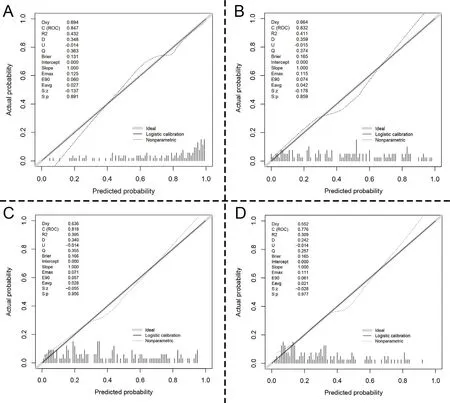
Fig.3.Calibration curves of the developed nomograms for effectiveness.Calibration curves of the prediction models for any decrease(A),decrease to a lowest level of 5 mg/dL(B),and decrease to 3 mg/dL (C) and to 2 mg/dL (D) are not significantly deviated from the diagonal (ideal) lines. P-values >0.05 indicate that the predicted probabilities of the nomograms are relatively accurate.
Some studies indicated that for selected HCC patients with obstructive jaundice,local treatment could be performed without drainage.However,liver failure and death have been reported in these patients.4,8,13,14,16Predicting TBil changes would therefore be beneficial.To our knowledge,this study is the largest multi-center study on the subject.We performed analysis on several endpoints for physicians following different routines.4-25The models performed well in internal validation.For all four endpoints,DCA analysis showed that predicted ranges of clinically beneficial prediction covered considerably wide probability spaces that encompassed their respective effective rates(Fig.4).We would therefore like to suggest that patients with earlier stage HCC and obstructive jaundice be evaluated by these models when planning for treatment without drainage.Considering that the mean survival time could be between only 1 and 3 months in patients with advanced HCC and jaundice who were drained without improvement,2,3,6,9,11,12,15,18-25it would be worthwhile to assess the risk of inefficacy before deciding whether to perform even palliative drainage for them.
Due to the small number of patients involved,external validation was impractical;however,internal validation showed good fit and DCA plots revealed acceptable potential benefit.Another limitation was that the size and count of the tumor lesions were ranked.This was done in accordance with current guidelines and to minimize error,although it may have caused the computational process to be underestimated.
5.Conclusions
In conclusion,the prediction models could facilitate preprocedural prediction of effectiveness of PTBD for HCC patients with HBV-related cirrhosis and obstructive jaundice.We analyzed several TBil targets so that the models could serve patients and physicians seeking data-based reference,when they are either looking for only the best palliative care or aiming to treat the HCC eventually.Such help is relevant because PTBD is after all an invasive procedure.
Authors’ contributions
H.Wang,Y.Mao and C.Zhang contributed equally to this work and should be considered co-first authors.The current study involved cooperation among four different institutions.H.Wang,Y.Mao and C.Zhang led the team in the majority of the collaboration works.H.Wang led data analysis and article writing,Y.Mao led data analysis and C.Zhang led data collection.X.Hu,B.Chen,L.Mu,S.Wang,and Y.Lin participated in study design,data collection,analysis,and article writing.Z.Xiang and M.Huang led the team on study design,together instructed as well as monitored data analysis and article writing,and were both responsible for the research.
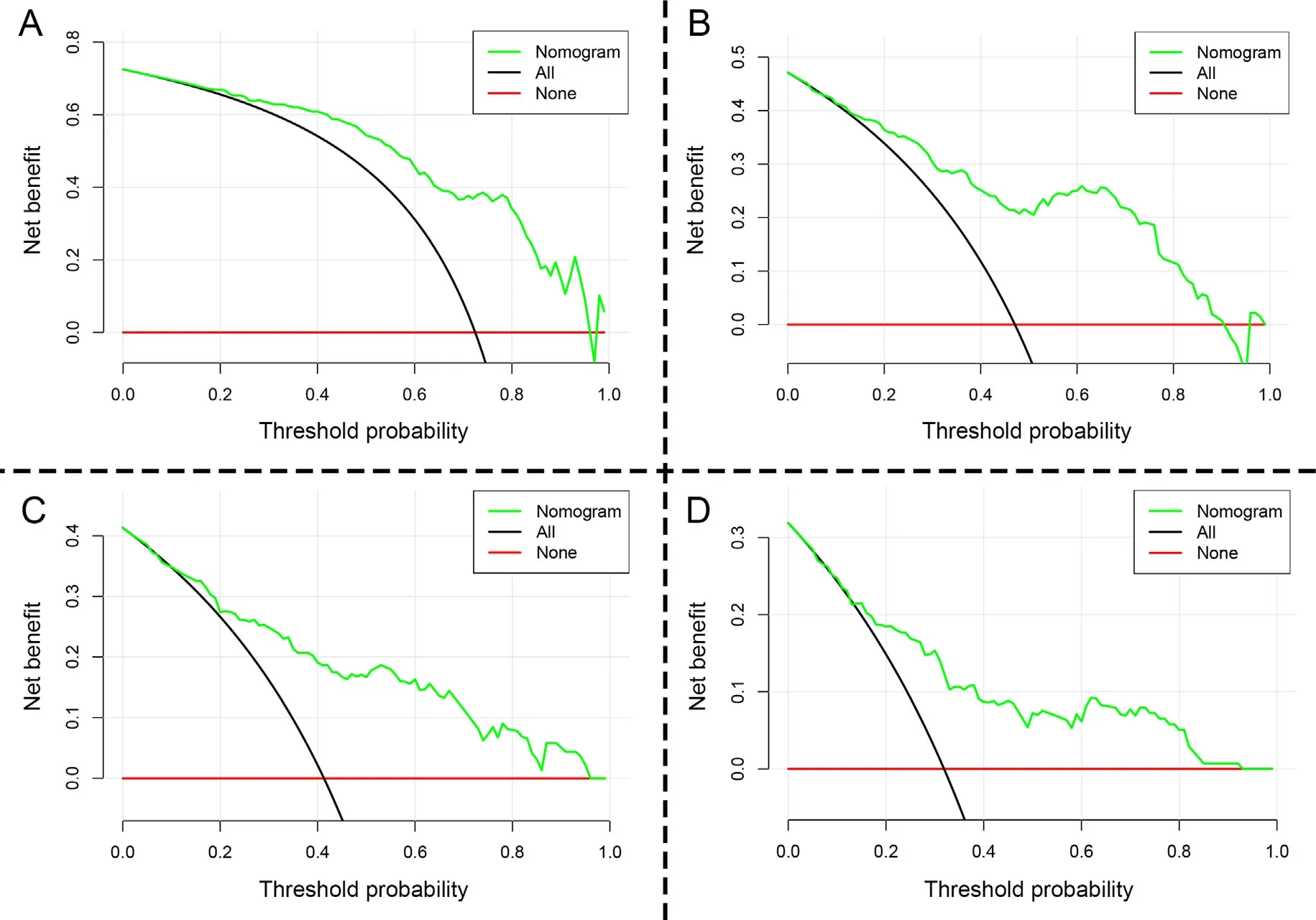
Fig.4.Decision curve analysis (DCA) of the developed nomograms indicating their respective usefulness.The y-axis shows the net benefit,and the x-axis represents the threshold probability.The probability at which the expected benefit with treatment is equal to the predicted benefit without treatment is known as the threshold probability.The green lines represent the developed nomograms.The black and red lines represent,respectively,the assumptions that all or none of the patients achieved effectiveness.For the“any decrease” endpoint,the DCA (A) showed that if the threshold probability was >0.2 and <0.95,then using the developed nomogram to predict effectiveness would confer greater benefit than treating either all or none of the patients.For<5 mg/dL endpoint(B),the threshold probability was>0.2 and<0.9.The threshold probability was>0.2 and<0.95 for 3 mg/dL (C) and >0.2 and <0.85 for 2 mg/dL (D).
Declaration of competing interest
No one in our team claims any conflict of interests.
Acknowledgements
We thank the patients and their families as well as the study-site personnel.This study was funded by National Natural Science Foundation of China (81701847 to Y.Mao) and Natural Science Foundation of Hunan Province(2017JJ3497 to Y.Mao).The funding body took no part in the design of the study and collection,analysis,and interpretation of data and in writing the manuscript.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.livres.2022.11.008.
杂志排行
Liver Research的其它文章
- Pathogenesis of fatty liver diseases and hepatocellular carcinoma☆
- Prevalence,diagnosis,treatment,and associated factors of hepatitis C in the United States from 1999 to 2018: A population-based crosssectional study☆
- Effects of apical sodium-bile acid transporter inhibitor and obeticholic acid co-treatment in experimental non-alcoholic steatohepatitis☆
- MUTYH is a potential prognostic biomarker and correlates with immune infiltrates in hepatocellular carcinoma☆
- Chemical basis of pregnane X receptor activators in the herbal supplement Gancao (licorice)☆
- Hepatic transcriptome profiling reveals early signatures associated with disease transition from non-alcoholic steatosis to steatohepatitis☆