CLlF-SOFA and CLlF-C scores for the prognostication of acute-onchronic liver failure and acute decompensation of cirrhosis: A systematic review
2023-01-03EbrahimRashedJonathanSoldera
Ebrahim Rashed, Jonathan Soldera
Abstract BACKGROUND Acute-on-chronic liver failure (ACLF) is a syndrome characterized by decompensation in individuals with chronic liver disease, generally secondary to one or more extra-hepatic organ failures, implying an elevated mortality rate.Acute decompensation (AD) is the term used for one or more significant consequences of liver disease in a short time and is the most common reason for hospital admission in cirrhotic patients.The European Association for the Study of Liver-Chronic-Liver Failure (EASL-CLIF) Group modified the intensive care Sequential Organ Failure Assessment score into CLIF-SOFA, which detects the presence of ACLF in patients with or without AD, classifying it into three grades.AIM To investigate the role of the EASL-CLIF definition for ACLF and the ability of CLIF-SOFA, CLIF-C ACLF, and CLIF-C AD scores for prognosticating ACLF or AD.METHODS This study is a literature review using a standardized search method, conducted using the steps following the guidelines for reporting systematic reviews set out by the PRISMA statement.For specific keywords, relevant articles were found by searching PubMed, ScienceDirect, and BioMed Central-BMC.The databases were searched using the search terms by one reviewer, and a list of potentially eligible studies was generated based on the titles and abstracts screened.The data were then extracted and assessed on the basis of the Reference Citation Analysis (https://www.referencecitationanalysis.com/).RESULTS Most of the included studies used the EASL-CLIF definition for ACLF to identify cirrhotic patients with a significant risk of short-term mortality.The primary outcome in all reviewed studies was mortality.Most of the study findings were based on an area under the receiver operating characteristic curve (AUROC) analysis, which revealed that CLIFSOFA, CLIF-C ACLF, and CLIF-C AD scores were preferable to other models predicting 28-d mortality.Their AUROC scores were higher and able to predict all-cause mortality at 90, 180, and 365 d.A total of 50 articles were included in this study, which found that the CLIF-SOFA, CLIF-C ACLF and CLIF-C AD scores in more than half of the articles were able to predict short-term and long-term mortality in patients with either ACLF or AD.CONCLUSION CLIF-SOFA score surpasses other models in predicting mortality in ACLF patients, especially in the short-term.CLIF-SOFA, CLIF-C ACLF, and CLIF-C AD are accurate short-term and long-term mortality prognosticating scores.
Key Words: End-stage liver disease; Acute-on-chronic liver failure; CLIF-SOFA; CLIF-C ACLF; CLIF-C AD
lNTRODUCTlON
Acute-on-chronic liver failure (ACLF) is a syndrome characterized by liver decompensation in individuals with chronic liver disease.It is associated with one or more extra-hepatic organ failures and an elevated mortality rate[1-4].
Acute decompensation (AD) is the term used for the occurrence of one or more significant complications of liver disease in a short period of time (i.e., bacterial infection, gastrointestinal haemorrhage, ascites, encephalopathy)[5-9].It is the most common reason for hospital admission in cirrhotic patients.Most of these patients will develop AD without any other significant features, while others will develop AD associated with multiple organ failures (i.e., kidney failure, declining liver function, and/or other organ failures).Nevertheless, AD patients with extra-hepatic organ failures are at greater risk for shortterm mortality[10-12].
In Europe and America, the primary cause of ACLF is alcohol, while viral hepatitis infection is the main cause of ACLF in Asia, particularly in China[13].Despite procedures such as haemodialysis and liver transplantation significantly increasing short-term survival, they are not widely available in medical care due to their high cost, the requirement for hospital admission, and the limited availability of liver resources[14].ACLF places a significant financial burden on patients and on the healthcare system.
A European prospective multi-centric study named CANONIC developed and published in 2013 definitions and a classification and grading of ACLF.The most common reasons for cirrhosis were alcoholic liver disease, chronic hepatitis C, and/or both[15].Hepatic (alcoholic liver injury) and extrahepatic disorders (gastrointestinal bleeding or bacterial infection) were the most common precipitating disorders for decompensation of cirrhosis, with or without ACLF.The most common organ failures (OFs) were kidney (55.8% of ACLF patients) and liver failure (43.6%), then coagulation (27.7%) and cerebral failure (24.1%).Heart and respiratory failures were the least common, around 16.8% and 9.2%, respectively[15].Twenty-eight-day transplant-free mortality rate in ACLF patients was 32.8%, while in patients without ACLF, it was 1.9%[15].
Ascites, a higher model for end-stage liver disease (MELD) score, low haemoglobin (Hb) levels, and low mean arterial pressure were defined as predictive factors for ACLF development in a large singlecentre Italian prospective cohort of cirrhotic outpatients[16].The European Association for the Study of Liver-Chronic-Liver Failure (EASL-CLIF) consortium has stated that today's global mortality rate of ACLF ranges from 30% to 50%.
The aim of the current study is to provide an overview of research into the role of the EASL-CLIF definition for ACLF, as well as the ability of CLIF-Sequential Organ Failure Assessment (SOFA), CLIF-C ACLF and CLIF-C AD scores to predict adverse outcomes associated with chronic liver disease.
Prognostic scoring systems
Various predictive scores have previously been developed.Nearly fifty years ago, the Child-Turcotte-Pugh (CTP) (Table 1) score was established as the most relevant liver-specific score[17].Wiesner's study evaluated data to develop the MELD score that outperformed the CTP score in predicting 90-d death in individuals with chronic end-stage liver disease[18].The MELD-Na score (Table 2), which combines the MELD score with serum sodium content, has enhanced predictive accuracy in patients with cirrhosis awaiting liver transplantation[19].The CLIF-SOFA score, a new scoring system that is an adaptation of the original SOFA score, was used to describe ACLF in the EASL-CLIF CANONIC study of ACLF in cirrhotic patients (Table 3).It has been used to distinguish AD from ACLF, classifying it into three grades[15].The EASL-CLIF consortium also established the CLIF consortium organ failure (CLIF-C OF) score.
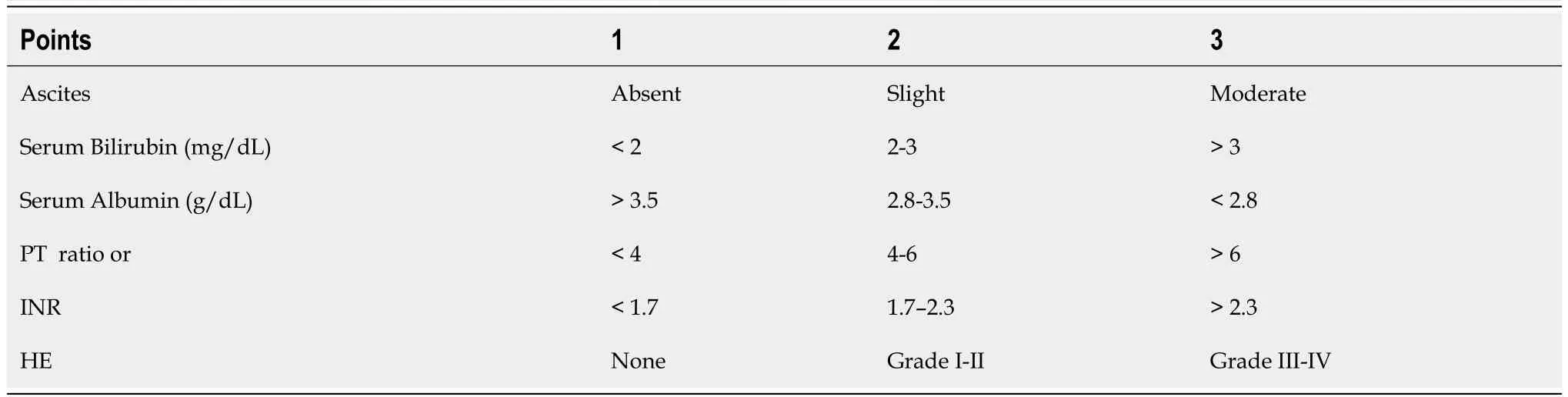
Table 1 Child-Turcotte-Pugh scores

Table 2 MELD and MELD-Na[62,63]: Model for end-stage liver disease-sodium
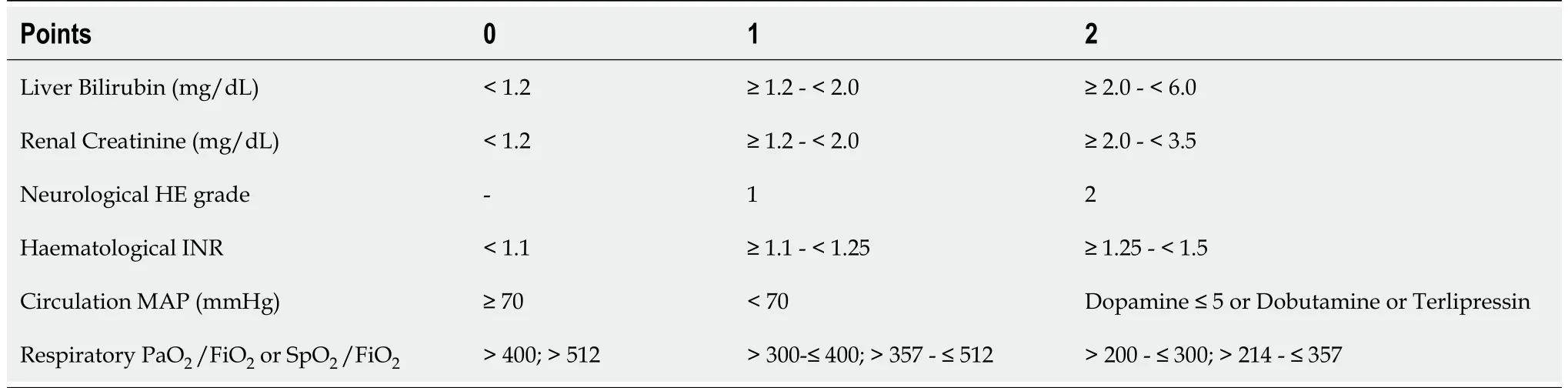
Table 3 CLlF-SOFA score[64]
Jalanet al[20], described that age and white blood cell (WBC) counts are independent risk factors for death in subsequent investigations and developed the CLIF-C ACLF score.The EASL-CLIF Group created an online calculator for calculating CLIF-SOFA and either CLIF-C ACLF or CLIF-C AD (https://www.clifresearch.com/ToolsCalculators.aspx).
CLIF-C ACLF Score Formula: The CLIF-C ACLF Score Formula[21] combines (CLIF-C OF score, age, and WBC) with the following formula: CLIF-C ACLF = 10 × [0.33 × CLIF-OFs + 0.04 × Age + 0.63 × Ln (WBC)] - 2.
CLIF-C AD Score Formula: The CLIF-C AD Score Formula (non-ACLF patients with AD) combines (Age, Creatinine, international normalized ratio (INR), WBC, and Sodium) with the following formula[22,23]: CLIF-C AD = 10 × [0.03 × Age + 0.66 × Ln (Creatinine mg/dL) + 1.71 × Ln (INR) + 0.88 × Ln (WBC 109cells/L) - 0.05 × (Sodium mmol/L) + 8].
ACLF Grades[15]: Grade I ACLF: Only kidney failure.[According to Shahet al[24], grade 1 could be with one of the following: Liver failure, kidney failure, coagulation, circulatory, or lung failure, with creatinine (1.5 - 1.9 mg/dL), or hepatic encephalopathy (grade 1 or 2), or brain failure with creatinine (1.5 - 1.9 mg/dL)].Grade II ACLF: Two organ failures.Grade III ACLF: Three organ failures.
MATERlALS AND METHODS
This study is a literature review using a standardized search method, conducted using the steps following the guidelines for reporting systematic reviews set out by the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-analyses)[25].
Search strategy
For relevant original studies, a literature search was conducted using PubMed, ScienceDirect, and BioMed Central-BMC databases.The search command used was a combination of words and Boolean characters: ("CLIF-SOFA" OR "CLIF-C ACLF" OR "CLIF-C AD") AND ("acute-on-chronic liver failure").Reference Citation Analysis (https://www.referencecitationanalysis.com/) was used to supplement the search.
Study selection
Studies were included if they analyzed data of patients more than 18 years old from the emergency department or inpatient settings.They needed to report data using ACLF definitions and scores published by the EASL-CLIF group and had a full text available.Studies were excluded if they used only scores other than CLIF-SOFA and CLIF-C AD or CLIF-C ACLF, if they were not written in English or if they were reviews, letters, editorials, opinion articles, conference abstracts, andin-vitrostudies.
Data extraction and synthesis
The databases were searched using the above search terms by one reviewer, and a list of potentially eligible studies was generated based on the titles and abstracts screened.Then, a full-text review was conducted, using the inclusion and exclusion criteria.
RESULTS
Study selection
Figure 1 shows the study search and the selection process, including the reasons for exclusion after a full-text review.A total of 50 related articles were included in the final review.
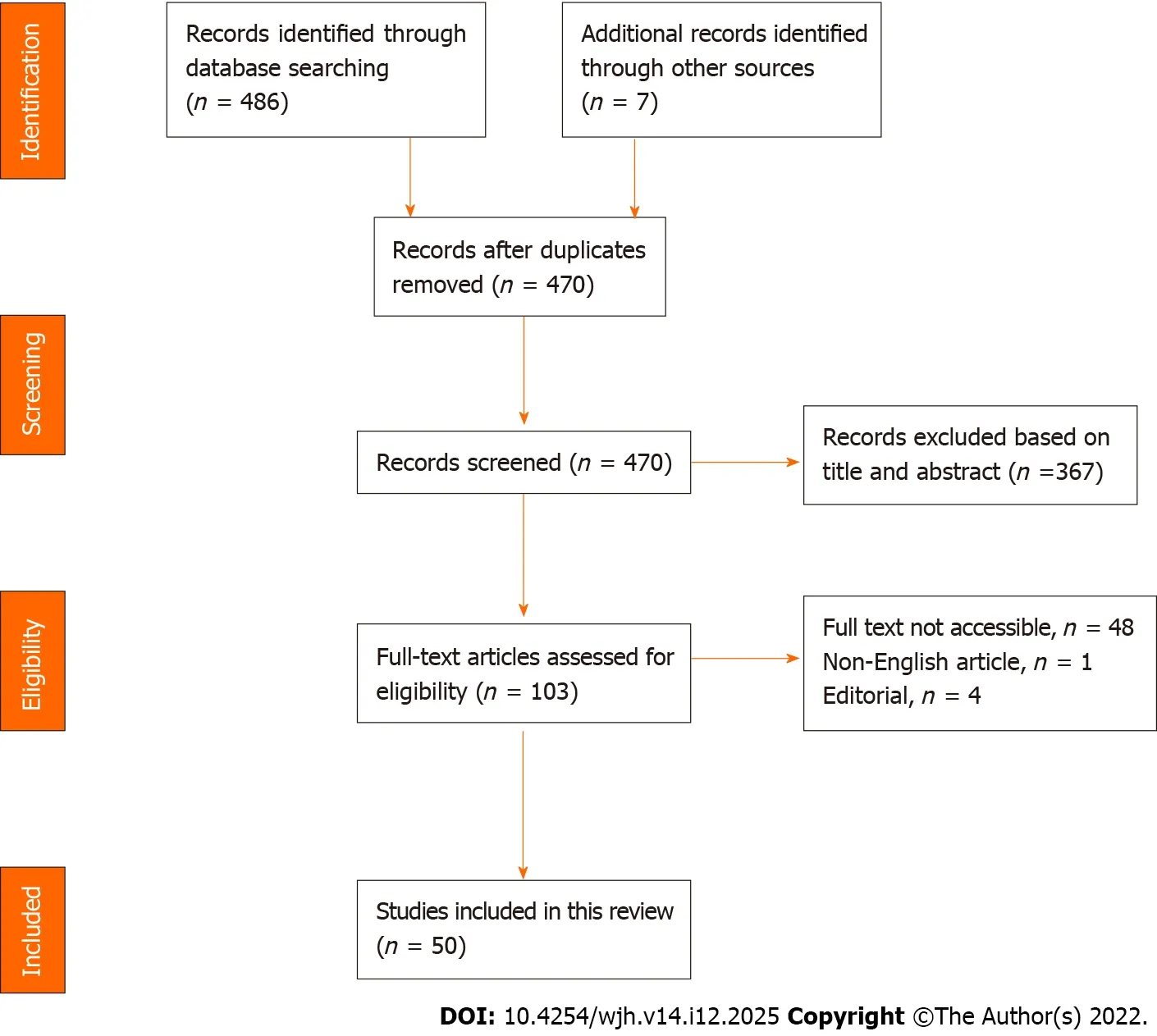
Figure 1 PRlSMA diagram of the study selection process.
Study quality
Most of the included studies used the EASL-CLIF definition for ACLF to identify patients with cirrhosis who had a significant risk of short-term mortality.Some articles used the Asian Pacific Association for the Study of the Liver and Chinese Group on the Study of Severe Hepatitis B-ACLF (COSSH-ACLF) prognostic criteria.The included studies were not assessed using a quality assessment tool, although they were considered to be good quality.
Study outcome
The primary outcome in all reviewed studies was mortality.Most of the studies' findings were based on an area under the receiver operating characteristic curve (AUROC) analysis, which revealed that CLIFSOFA, CLIF-C ACLF, and CLIF-C AD scores were preferable to other models predicting 28-d mortality (Table 4).They had the greatest AUROC scores predicting overall mortality at 90, 180, and 365 d.

Table 4 Summary of selected studies
DlSCUSSlON
ACLF has become a serious medical challenge, and it remains a complex clinical scenario for hepatologists and specialists in different related departments due to its severe presentation, and quick disease course with high short-term mortality.Regional differences when defining ACLF and understanding its diagnostic methods has led to many clinical phenotypes.The current therapeutic management of ACLF patients primarily focuses on treating and supporting multiple organ failures[26].
The CANONIC study introduced accurate criteria for the diagnosis of this condition.The CLIF-SOFA score was developed and evaluated for the prognosis of ACLF in the CANONIC research[15].This development has increased the ability to distinguish patients with ACLF from those with AD using the CLIF-SOFA parameters[15].
Every scoring system has advantages and disadvantages.Even though the CLIF-SOFA score has a significant prognosticative accuracy, its calculation is challenging due to the combination of many indicators[14].The CTP score is calculated by the ascites, serum bilirubin, albumin, prothrombin time, and hepatic encephalopathy (HE) levels[17].The presence of HE and ascites is a component of the CTP score; nevertheless, these are subjective, without a defined cut-off value.The MELD score includes three laboratory markers: INR, bilirubin, and creatinine; nevertheless, it is susceptible to confounding factors such as haemorrhage, ascites, and diuretic treatment, and there are no obviously defined cut-off levels for identifying patients with cirrhosis[27].The MELD score does not include subjective indicators, which may diminish evaluating reliability[28].
Hyponatraemia is strongly associated with the prognosis of cirrhotic patients, especially those with ascites; thus, the MELD-Na score was developed to improve on the MELD score[29].
Jalanet al[20] in 2014, showed that the CLIF-C OF accuracy is similar to the CLIF-SOFA score in predicting mortality.The CLIF-C ACLF score does not consider only the role of extra-hepatic organ injuries, circulatory system failure, and coagulation impairment on prognosis, but also includes the WBC count, in order to assess the level of inflammation.In this study, the CLIF-C ACLF score outper-formed the CTP, MELD and MELD-Na scores[30].

images/BZ_50_229_229_2250_3204.png

images/BZ_51_229_229_2250_3207.png

images/BZ_52_229_229_2250_3237.png

ACLF: Acute-on-chronic liver failure; AD: Acute decompensation; AUC: Area under the curve; AOVH: Acute oesophageal variceal haemorrhage; HRS: Hepatorenal syndrome; CTP: Child-Turcotte-Pugh; SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2; MELD: Model of End-Stage Liver Disease; iMELD: integrated MELD; MELD-Na: sodium MELD; CPC: Child-Pugh class; SOFA: Sequential Organ Failure Assessment; CLIF-SOFA: CLIFConsortium modification of Sequential Organ Failure Assessment; CLIF-C OF: Organ Failure score; ICU: Intensive care unit; CHB: Chronic hepatitis B; IPA: Invasive pulmonary aspergillosis; CMA: Cow milk induced allergies; APASL: Asian Pacific Association for the Study of the Liver; CPS: Complex Problem Solving; LT: Liver transplantation; PPV: Pulse pressure variation; BSI: Bronchiectasis severity index.
This was also true of the CANONIC study data, which demonstrated that CLIF-SOFA, CLIF-C OF and CLIF-C ACLF scores were able to outperform CTP, MELD, and MELD-Na scores when predicting short- and long-term mortality in ACLF patients[15,20].
ACLF and infection
Zhanget al[31] in 2018, assessed the relationship between bacterial infection and predictors of mortality in ACLF patients with autoimmune liver disease.No significant association was found between 28-d and 90-d transplant-free mortality and any predictor.The CTP, MELD, and CLIF-SOFA scores of ACLF patients with bacterial infection were all high[31].
ACLF and ascites
Ascites at admission were a potential risk for post-enrollment development of ACLF in the study by Moreauet al, as it is an independent prognostic factor of renal failure following bacterial infection[15,32,33].CLIF-SOFA scores at enrollment and ACLF diagnosis were significant independent predictors for post-enrollment ACLF development and ACLF-associated death, respectively[15].
ACLF and albumin-bilirubin
The albumin-bilirubin (ALBI) score, which uses albumin and bilirubin values to indicate liver injury, effectively predicts the outcome of hepatocellular carcinoma[34].The ALBI score and the CLIF-SOFA score had a comparable effect in predicting the outcome of ACLF patients, according to the findings of Liuet al[35].
ACLF and hepatitis B virus
Hepatitis B virus (HBV) is the most common etiology of ACLF in the East, which differed from patients in Western societies.HBV-ACLF is a pan-Asian and African condition associated with excessively elevated short-term mortality[36].In 2021, Liet al[37] created a new simple prognostic score that can accurately predict outcomes in HBV-ACLF patients.The C-indices of the new score were significantly higher than the C-indices of four existing scores (COSSH-ACLF, CLIF-C ACLF, MELD, and MELD-Na) for 28- and 90-d mortality.Without assessing organ failure, the novel prognostic score can correctly predict short-term mortality in patients with HBV-ACLF and could be used to guide clinical care[37].In Taiwan, a viral hepatitis endemic country[38], a study demonstrated that APACHE III, CLIF-OF and CLIF-C ACLF scores have outperformed other models for predicting 28-d overall mortality[38].
ACLF and HRS
Terreset al[39] assessed and compared the significance of liver-specific scores in predicting mortality in hepatorenal syndrome (HRS) patients who received terlipressin.CTP was superior to CLIF-SOFA, CLIFACLF, MELD, and MELD-Na in estimating 30-d, 90-d, and 365-d mortality[39].
ACLF and AOVH
CTP was superior to CLIF-SOFA, CLIF-ACLF, MELD, and MELD-Na in estimating 30-d and 90-d mortality in AD patients, while CLIF-SOFA was better in ACLF patients with acute oesophageal variceal haemorrhage (AOVH) who received terlipressin[40].
ACLF and SBP
CLIF-SOFA has demonstrated superior performance in spontaneous bacterial peritonitis (SBP)[41] and alcoholic hepatitis[42].
ACLF and AKI
Both the standard and the modified CLIF-SOFA scores demonstrated remarkable accuracy for the prognostication of 28-d transplant free-mortality evaluation (AUC-ROC greater than 0.9) in acute kidney injury (AKI) patients with cirrhosis and AD.Nevertheless, it presents a reduced effectiveness in 90-d mortality assessment (AUC-ROC 0.78).These results are comparable to the results reported by Angeliet al[43] in 2015.
Hepatic and extra-hepatic injury
A study by Guptaet al[44] in 2017, that included hepatic and extra-hepatic ACLF patients showed that, in the hepatic group, iMELD was the best indicator of 28-d mortality.On the other hand, CLIF-SOFA was the strongest predictor of death in the extra-hepatic ACLF cohort.The majority of patients in this cohort were decompensated, and infection was the most frequent extra-hepatic event, leading to systemic inflammation and extra-hepatic organ involvement with fewer liver failures[44].
Critically unwell conditions
In predicting 90-d mortality, the SOFA score surpassed the more commonly used prognostic liverspecific scores (MELD, SOFA, CLIF-SOFA, CLIF-C OF, and CLIF-C ACLF/CLIF-C AD) in a study conducted to describe the best mortality risk factor(s) in critically unwell ACLF patients[45].The CLIF-C ACLF, CLIF-C OF and ACLF grades varied widely between ACLF patients who underwent liver transplantation and those who died waiting for an organ.At the time of admission, those with two or three organ failures had survival rates ranging from 30% to 55%, whereas patients with more than three organ failures had mortality rates approaching 80%[46].
AD and SARS-CoV-2
Mendizabalet al[47] performed a study to evaluate whether severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection affects the outcome of hospitalized cirrhotic patients and to assess the effectiveness of the different prognostic models in predicting mortality.CLIF-C scores performed better than North American Consortium for the Study of End-Stage Liver Disease (NACSELD)-ACLF score, CTP, and MELD-Na.
ACLF and alcohol intake
Aggressive alcohol intake, alcoholic hepatitis, and bacterial infection were the most common causes of ACLF in alcohol liver disease[48].The AUROCs of the CLIF-SOFA, CLIF-OF, and CLIF-C scores showed a slight superior effect in estimating short-term mortality; however, they were equivalent to MELD and MELD-Na[49].To clarify this finding, Chirapongsathornet al[49] had elevated short- and long-term mortality rates.In patients with ACLF, as per the CLIF-C definition, the prediction accuracy of the CLIFSOFA, CLIF-OF and CLIF-C scoring tools were no better than the accuracy of MELD and MELD-Na scores.In a retrospective investigation by Leeet al[50] the CLIF-SOFA score surpassed other scoring systems in estimating short-term mortality in alcoholic cirrhotic patients with AD.
Prognostic scores and liver transplantation
The MELD score is commonly used in liver transplantation (LT) as a scoring method for organ allocation and is the standard model prognostic tool for predicting 3-mo to 6-mo survival in patients with liver failure[51].Nevertheless, ACLF has a distinct clinical characteristic (Table 5); therefore, the MELD score for patients with ACLF is not expected to be optimal[52].

Table 5 Acute-on-chronic liver failure vs acute decompensation liver transplantation[45]
The MELD score was associated with post-transplant survival but is considered to have poor prediction accuracy[53].No more trials demonstrated that CLIF-SOFA, CLIF-C ACLF, or CLIF-C OF had good prognostic value for short-term survival after LT[52].
General comparison of prognostic scores
Despite the excellent predictive accuracy of CLIF-C ACLF and CLIF-C OF scores, they were developed analyzing data from patients generally with alcohol-related liver disease from Europe and the United States, and more research is necessary to confirm whether this is appropriate for Asian populations.However, according to the study by Zhanget al[14], the scores were also applicable in Asian populations.
A higher CLIF-SOFA was separately associated with higher mortality; this is consistent with previous research, which found that the CLIF-SOFA was better than other liver-specific scores in predicting mortality[42,54,55].It has been shown by other researchers that CLIF-C ACLF or CLIF-C AD, MELD, and MELD-Na are preferred, even for extra-hepatic injuries[56,57].
In the study by Zhanget al[14], the prognostication accuracy and power of the six scores (CTP score, MELD score, MELD-Na, CLIF-ACLF score, CLIF-C OF score and CLIF-SOFA score) were analyzed and compared for 28-, 90- and 180-d overall mortality.The AUROC of CLIF-SOFA was superior to other predictive scores at 28-, 90-, and 180-d mortality, particularly at 28 d.The CLIF-SOFA score provides an overall and efficient evaluation of the severity of multi-organ failure in patients with ACLF by considering various systems, including the hepatic, respiratory, coagulation, circulatory, nervous, and renal systems.Zhanget al[14] and other researchers found that at all times, the CLIF-SOFA scores AUROCs were higher than those of other scores.A study performed by Perdigotoet al[58] showed that when ACLF is present, the CLIF-C OF score has good accuracy and is able to diagnose ACLF.MELD, on the other hand, performed better in terms of 90-d mortality prediction.
The CLIF-C ACLF score is the most accurate way to predict 28-d mortality in patients with ACLF.The CLIF-C AD score was also beneficial in predicting death in cirrhotic individuals with AD who did not meet diagnostic criteria for ACLF, although it did not outperform other well-established prognostication measures[59].
The CANONIC study found that 28-d mortality was 33.9%, while two Brazilian studies found that mortality rates in ACLF patients were 39%[56,60].
Within the included articles in this study from 2013 to 2022 (Figure 2), CLIF-SOFA was superior to other scores for predicting mortality (mostly in the short-term) in ACLF patients in more than 50% of the included articles, followed by CLIF-C ACLF and CLIF-C AD (30% of the articles)[61-89].CLIF-C OF was more accurate at 10%.CTP accurately prognosticated ACLF patients with HRS and AOVH patients with AD.The MELD score accurately predicted short-term mortality in ACLF patients who underwent LT (Figure 3).

Figure 2 Year of publication.
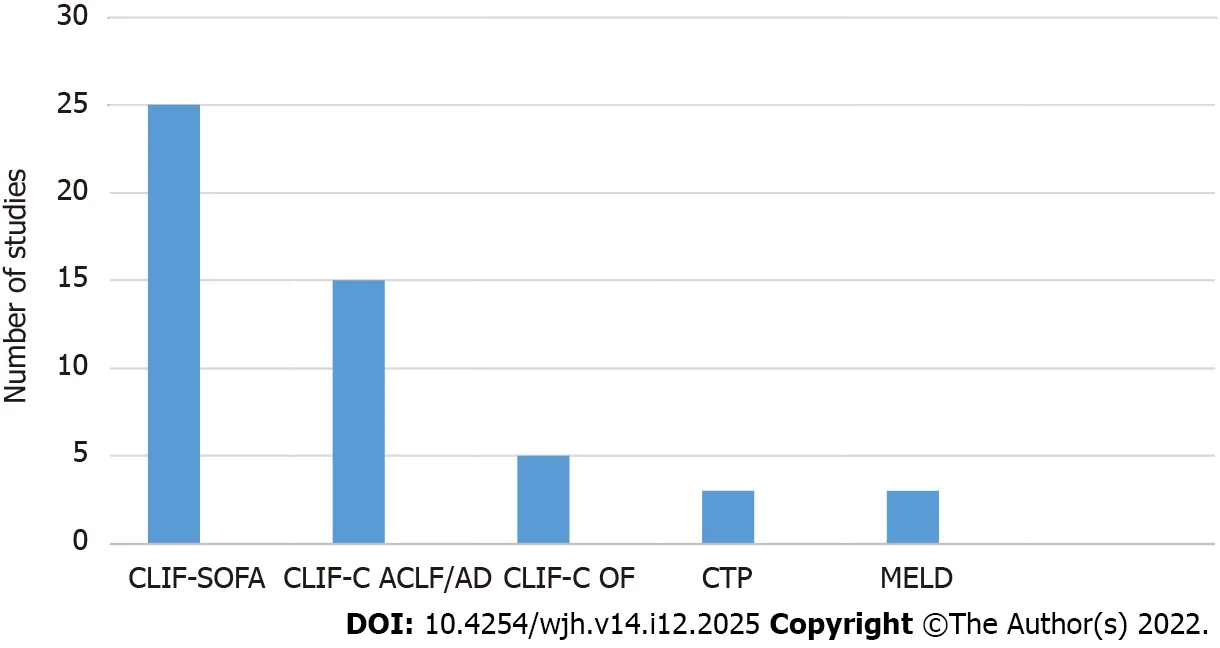
Figure 3 Predicting scores accuracy according to studies.ACLF: Acute-on-chronic liver failure; AD: Acute decompensation; CTP: Child-Turcotte-Pugh; SOFA: Sequential Organ Failure Assessment; CLIF-SOFA: CLIF-Consortium modification of Sequential Organ Failure Assessment; CLIF-C OF: Organ Failure score; MELD: Model of End-Stage Liver Disease.
CONCLUSlON
The CLIF-SOFA score surpasses other predictive models in prognosticating short-term mortality in ACLF patients.CLIF-SOFA, CLIF-C ACLF, and CLIF-C AD are accurate in predicting scores for shortterm and long-term mortality in patients with ACLF and in predicting adverse outcomes associated with chronic liver disease.
ARTlCLE HlGHLlGHTS
Research background
Acute-on-chronic liver failure is a syndrome characterized by decompensation in individuals with chronic liver disease, and is generally secondary to one or more extra-hepatic organ failures, implying an elevated mortality rate.Acute decompensation is the term used for one or more significant consequences of liver disease in a short time and is the most common reason for hospital admission in cirrhotic patients.
Research motivation
The European Association for the Study of Liver-Chronic-Liver Failure (EASL-CLIF) Group modified the intensive care Sequential Organ Failure Assessment score into CLIF-SOFA, which detects the presence of acute-on-chronic liver failure (ACLF) in patients with or without acute decompensation(AD), classifying it into three grades.
Research objectives
To investigate the role of the EASL-CLIF definition for ACLF and the ability of CLIF-SOFA, CLIF-C ACLF, and CLIF-C AD scores for prognosticating ACLF or AD.
Research methods
This study is a literature review using a standardized search method, conducted using the steps following the guidelines for reporting systematic reviews set out by the PRISMA statement.Using specific keywords, relevant articles were found by searching PubMed, ScienceDirect, and BioMed Central-BMC.The databases were searched using the search terms by one reviewer (MSc student), and a list of potentially eligible studies was generated based on the titles and abstracts screened.
Research results
Most of the included studies used the EASL-CLIF definition for ACLF to identify cirrhotic patients with a significant risk of short-term mortality.The primary outcome in all reviewed studies was mortality.Most of the studies' findings were based on an AUROC analysis, which revealed that the CLIF-SOFA,CLIF-C ACLF, and CLIF-C AD scores were preferable to other models in predicting 28-d mortality.They had the greatest AUROC scores predicting overall mortality at 90, 180, and 365 d.A total of 50 articles were included in this study, which found that the CLIF-SOFA, CLIF-C ACLF, and CLIF-C AD scores could predict short-term and long-term mortality in patients with ACLF or AD in more than 50%of the articles found.
Research conclusions
The CLIF-SOFA score surpassed other predictive models in predicting short-term prognosis in ACLF patients.CLIF-SOFA, CLIF-C ACLF, and CLIF-C AD are accurate in predicting scores for short-term and long-term mortality in patients with ACLF and in predicting adverse outcomes associated with chronic liver disease.
Research perspectives
Within the included articles in this study from 2013 to 2022, CLIF-SOFA was superior to other scores for predicting mortality (mainly in the short-term) in ACLF patients in more than 50% of the included articles, followed by CLIF-C ACLF and CLIF-C AD (30% of the articles).CLIF-C OF was accurate at 10%.CTP accurately predicted the score for ACLF patients with HRS and AOVH patients with AD.The MELD score accurately predicted short-term mortality in ACLF patients who underwent LT.
FOOTNOTES
Author contributions:Both authors contributed to writing and reviewing the final draft of the manuscript.
Conflict-of-interest statement:All the authors declare no conflict of interest.
PRlSMA 2009 Checklist statement:PRISMA 2009 was observed, and a PRISMA figure is included in the manuscript.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United Kingdom
ORClD number:Ebrahim Rashed 0000-0001-5095-2868; Jonathan Soldera 0000-0001-6055-4783.
S-Editor:Liu JH
L-Editor:Webster JR
P-Editor:Liu JH
