Nurses’ experiences of caring for preterm infants in pain: A metaethnography
2022-11-05TingtingZhoAngelStrkwetherAdmMtsonShnmLinwlWnliXuXiomeiCong
Tingting Zho ,Angel R.Strkwether ,Adm Mtson ,Shnm Linwl ,Wnli Xu ,Xiomei Cong ,e,*
a School of Nursing,University of Connecticut,Storrs,CT,USA
b College of Nursing,University of Florida,Gainesville,FL,USA
c Division of Neonatology,Connecticut Children’s Medical Center,Hartford,CT,USA
d Department of Pediatrics,University of Connecticut School of Medicine,Farmington,CT,USA
e School of Nursing,Yale University,Orange,CT,USA
Keywords:Neonatal intensive care units Premature infant Pain measurement Parents Pain Nursing care Nurses
ABSTRACT Objective:Preterm infants are subjected to numerous painful procedures during their neonatal intensive care unit (NICU) hospitalization.Despite advancements in pain alleviation,nurses remain challenged to provide timely and effective pain management for preterm infants.Greater understanding of the lived experience of nurses caring for preterm infants in pain could provide novel insights to improve pain management for this vulnerable population.The aim of this meta-ethnography was to synthesize and interpret qualitative findings of nurses’ experiences of taking care of preterm infants in pain.Methods:An extensive literature search in PubMed,CINAHL,PsycINFO,Scopus,BIOSIS and ProQuest Dissertation and Theses Database was conducted,including studies within the past 10 years.Two nursing researchers conducted data extraction and analysis independently.Inclusion criteria were applied to search for qualitative studies of nurse participants who worked in the NICU taking care of preterm infants.Studies published in a language other than English,articles that did not include qualitative data and qualitative data that could not be extracted from the findings or did not discuss nurses’experiences were excluded.Critical Appraisal Skills Programme was used for literature quality evaluation.Results:Eight studies remained after further screening according to inclusion and exclusion criteria.These eight studies were conducted from 2013 to 2018 and totally enrolled 205 nurses from Iran,Canada,the United States,Finland,Sweden,Switzerland,and Australia.Five themes emerged on the nurses’perspectives of taking care of preterm infants in pain: 1) They sense the neonatal pain;2) Adverse consequences of unrelieved pain;3) Barriers of managing pain;4) Concerns of available approaches for pain relief;5) Failure to work with parents.Conclusions:This meta-ethnography identified nurses’understanding of pain in preterm infants that can be assessed,and they acknowledged that unrelieved pain could cause developmental deficits in infants.The barriers are lack of training and support on pain assessment and intervention in preterm infants.Optimizing workload and environment,developing age-specified pain assessment and intervention,receiving emotional support and training,and building up a rapport with parents are urgent needs for nurses to provide better care to infants having pain.
What is known?
· Preterm infants experience enormous pain during their early life in the neonatal intensive care unit (NICU),which may cause adverse consequences that may persist into adulthood.
· Timely and effective pain assessment and intervention provided by NICU nurses to preterm infants will benefit their health outcomes.
What is new?
· This review thoroughly summarizes NICU nurses’ lived experience in their assessment and management of neonatal pain,which provides new insights into nurses’concerns and research gaps in NICU standard nursing care.
· The findings indicate nurses’ experiences with the adverse consequences of unrelieved pain,barriers to managing pain,concerns about current approaches for pain relief,and urgent needs to work with parents when caring for preterm infants with pain.
1.Introduction
Approximately 15 million infants are born each year prematurely worldwide,defined as <37 weeks gestational age[1].As part of lifesaving treatment,these preterm infants are exposed to more than 300 necessary but invasive procedures during an average neonatal intensive care hospital stay[2].Our recent study showed that during the first 28 days of hospital stay,averagely preterm infants experienced 614.12 acute pain/stress events (e.g.,mouth care,diaper change,position change,heel-stick,suctioning) and 1,023.65 h of chronic pain/stress stimulation (e.g.,nasogastric and orogastric tube in situ,continuous positive airway pressure manipulation,chest tube placed on wall suction) [3].Repetitive pain-induced stresses have been shown to sensitize the nervous system of preterm infants [4] through enhanced nociceptor excitation [5] and reduced inhibitory transmission in the spinal cord dorsal horn [6].Altered pain sensitivity [7] has been associated with significant changes in the somatosensory function,increasing vulnerability to chronic pain [8],and neurodevelopmental impairments[9,10].The adverse consequences of repetitive pain-induced stresses can persist through childhood and even into adulthood[11,12].
Pediatric nurses are playing a pivotal role in caring for preterm infants in pain.Nurses take charge of pain assessment,pain management,infants and parents advocacy,and parents’ education.However,due to preterm infants’ immature nervous system [13]and challenging work environments in a newborn intensive care unit (NICU) such as infants’ medical complexity,demand for care,and lack of resources [14-16],there is limited evidence to inform the effectiveness in infants’ pain assessment and management.Thus,the synthesis of nurses’ experiences and perspectives caring for infants in pain will help provide novel insights to improve pain assessment and management for this vulnerable population.
Although a previous qualitative study revealed some themes and metaphors regarding nursing experiences in pain assessment and management in infants [13],there is a lack of summary of nurses’ lived experience in pain assessment and management.We thus conducted this review to thoroughly summarize nurses’ concerns in infants’ pain assessment and management in each study.Therefore,we can discover the patterns among those findings;identify the research gap;better understand the existing knowledge;interpret and develop the new theory;improve the nursing care standards and strengthen the health services[17].The purpose of this review is to develop a synthesis of qualitative studies to provide in-depth insight into nurses’ perceptions of pain assessment and alleviation in preterm infants.Our research question was developed according to the SPIDER model [18]: What are the nurses’ perceptions of pain assessment and alleviation in preterm infants at clinical settings?
2.Methods
2.1.Study design
Noblit and Hare’s[19]method of meta-ethnography was chosen because it is a well-developed methodology,has been widely used in health-related meta-synthesis,and its great potential for quality improvement in health service and public health [20].Enhancing transparency in reporting qualitative research synthesis (ENTREQ)was used to guide the data collection and synthesis reporting[21].
2.2.Procedure to locate qualitative studies
Articles were searched in PubMed,CINAHL,PsycINFO,Scopus,BIOSIS,and ProQuest Dissertation and Theses Database within the past 10 years (2012-07-01 to 2022-06-30).Five key terms were searched: nurses,pain,preterm infant,method,and settings.The categories were searched as follows,nurses:pediatric nurses,NICU nurses,nurses,nursing,pediatric nursing,neonatal nurses,nursing care,health professionals;pain:procedure pain,chronic pain,acute pain,pain assessment,pain intervention,pain management;preterm infant: preemie,infant,preterm,young gestational age,neonatal,premature,babies;method: qualitative study,experience,perspective,perceptions,ethnography,descriptive,phenomenology and mixed methods;settings: NICU,hospital,clinic,intensive care.
The target findings were grouped into five main parts: (a) pain in preterm infants;(b)the impact of pain on their health outcomes;(c) nurses’ stress;(d) challenges of pain assessment and management;(e) partner with parents.
2.3.Sample
Qualitative studies published within 10 years(2012-2022)were included if they addressed the nurses’caring for premature infants in pain and comprised the sample of this meta-synthesis.
2.3.1.Inclusion and exclusion criteria
Qualitative studies were included in the meta-synthesis if they met the following inclusion and exclusion criteria.Inclusion criteria: (a) primary qualitative studies (using any type of qualitative method including qualitative investigation in mixed methods studies) focused on the lived experience of nurses caring for premature infants with pain in the NICU;(b) published in English within the last 10 years (2012-2022).Exclusion criteria: (a)qualitative data cannot be extracted from the findings;(b) articles that did not discuss nurses’ experiences.
2.3.2.Quality appraisal
The quality appraisal was conducted by using the Critical Appraisal Skills Programme[22].Ten items checklist evaluated the research: the appropriation of research method,design,recruitment,data collection,the relationship between researcher and participants,the ethical consideration,data analysis,clarity,and value of findings.Qualitative studies were excluded from the review if they did not match any requirement of 10 questions [23].
2.4.Data extraction and analysis
Noblit and Hare’s seven steps of meta-ethnography approach[19]was used in this review including:1)Getting started.Conduct a literature review of nurses’ experiences and perspectives in caring for preterm infants with pain,consider whether the meta-synthesis is really needed to be conducted to find the gap or what metasynthesis can contribute to the current knowledge system;2)Deciding what is relevant.Determine qualitative studies relevant to the meta-ethnography topic: the nurses’ perceptions of caring for infants in pain;3)Reading and rereading the studies.Develop the key concepts through reading and rereading the studies which are included in this meta-synthesis.Locate the key metaphors and themes of each study by making a list or table.Modify and finalize the list and table.Develop a general map of the whole data;4)Determining how the studies are related.Extract key metaphors from each study,compare each theme and each metaphor with others,and find the patterns;5) Translating the studies into one another.Compare themes and metaphors between and within each study;6)Synthesizing translations.Translate the individual metaphors into the generalized themes;7)Expressing the synthesis.Disseminate the work and present the findings to a target audience,including nurses,other health care professionals and parents,policymakers,and nursing researchers.By conducting these seven steps methods,the final key metaphors were selected.
To examine the accuracy of data extraction,two researchers(T.Z.and X.C.) independently screened the studies by title,year,the contents of abstracts,inclusion and exclusion criteria,and data extraction and synthesis.During these search and review procedures,two researchers consistently compared and discussed their results.For any disagreements that occurred,a further discussion with other authors helped reach the final agreement.All metaphors were carefully compared and grouped by identifying the similarities and differences until the final themes emerged.
3.Results
After carefully searching the articles in the database,a total of 4,911 studies were identified of which 108 duplicates were removed.After reviewing all 4,803 abstracts,59 papers were left.After reviewing these 59 full articles,51 articles were excluded based on the inclusion and exclusion criteria: they are not the research about nurses’ experience;qualitative data cannot be extracted from the findings.Finally,eight articles[13,24-30]were included in the meta-ethnography(see Fig.1).Data were retrieved from eight articles which were published between 2013 and 2018.Authors,year of publication,sample size,age,sex,country,years of experience,education status,discipline,research design,and data analysis were extracted from the articles (see Tables 1 and 2).
3.1.Characteristics of the reviewed studies
Among the eight included studies,the total number of participants was 254 nurses,from seven countries,including the United States,Iran,Canada,Switzerland,Finland,Sweden,and Australia.Their age ranged from 20 to 64 years old.Two studies mentioned that their nurse subjects had bachelor’s degrees [24,25],while other studies did not specify their educational status.One study included three nurses who did not have any nursing experience yet[26].Four studies mentioned that their nurses had more than five years of experience in caring for preterm infants [24,25,27,28].Other three studies specified that their nurses had an average of 12.24 years-26.5 years of neonatal caring experience [13,29,30].
All the eight included studies had at least eight of ten items of CASP [22] (see Table 3),which meet the quality requirement of qualitative synthesis.Five articles clearly described all items in their study,while the other three studies did not consider the relationship between the researcher and participants and did not consider ethical issues.
Within all eight publications,totally 83 key metaphors were identified,and all metaphors were compared across qualitative studies using reciprocal translation [19].By using reciprocal translation comparation,authors assumed all the similar findings from eight articles and “adding” them together [19].Five overarching themes were developed by the authors after comparing the themes and metaphors from the original articles:1)They sense the neonatal pain;2) Adverse consequences of unrelieved pain;3)Barriers of managing pain;4)Concerns of available approaches for pain relief;5)Failure to work with parents.(see Table 4).Although not all key metaphors evenly appeared under each article’s overarching theme,five themes could be developed by analyzing the significant number of metaphors.
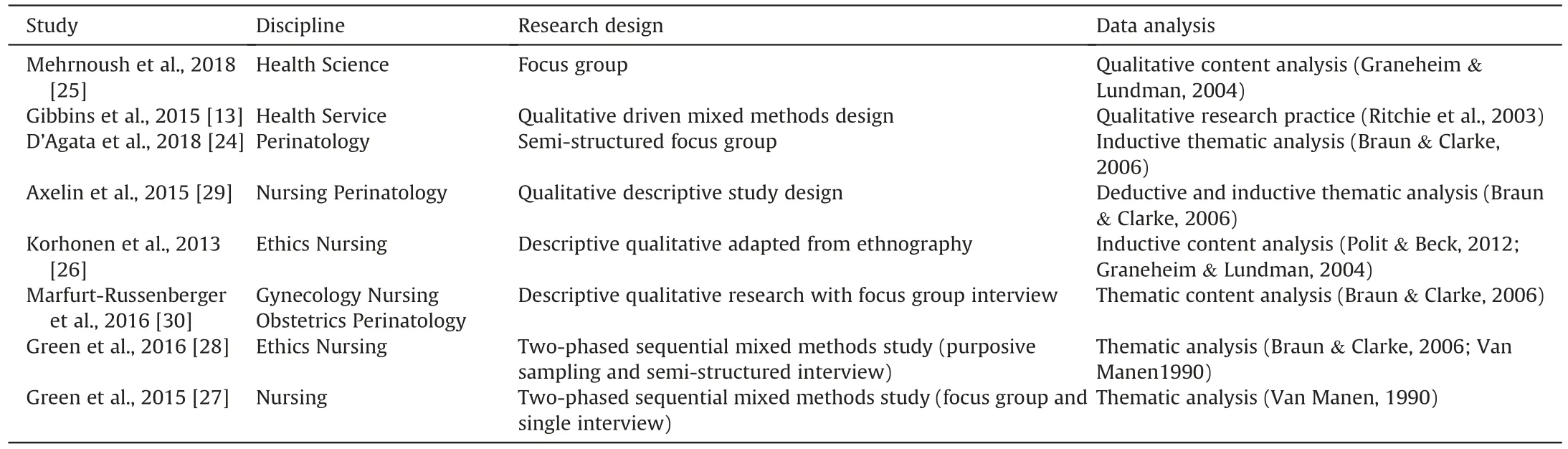
Table 1Methodological characteristic of qualitative studies in the meta-ethnography.
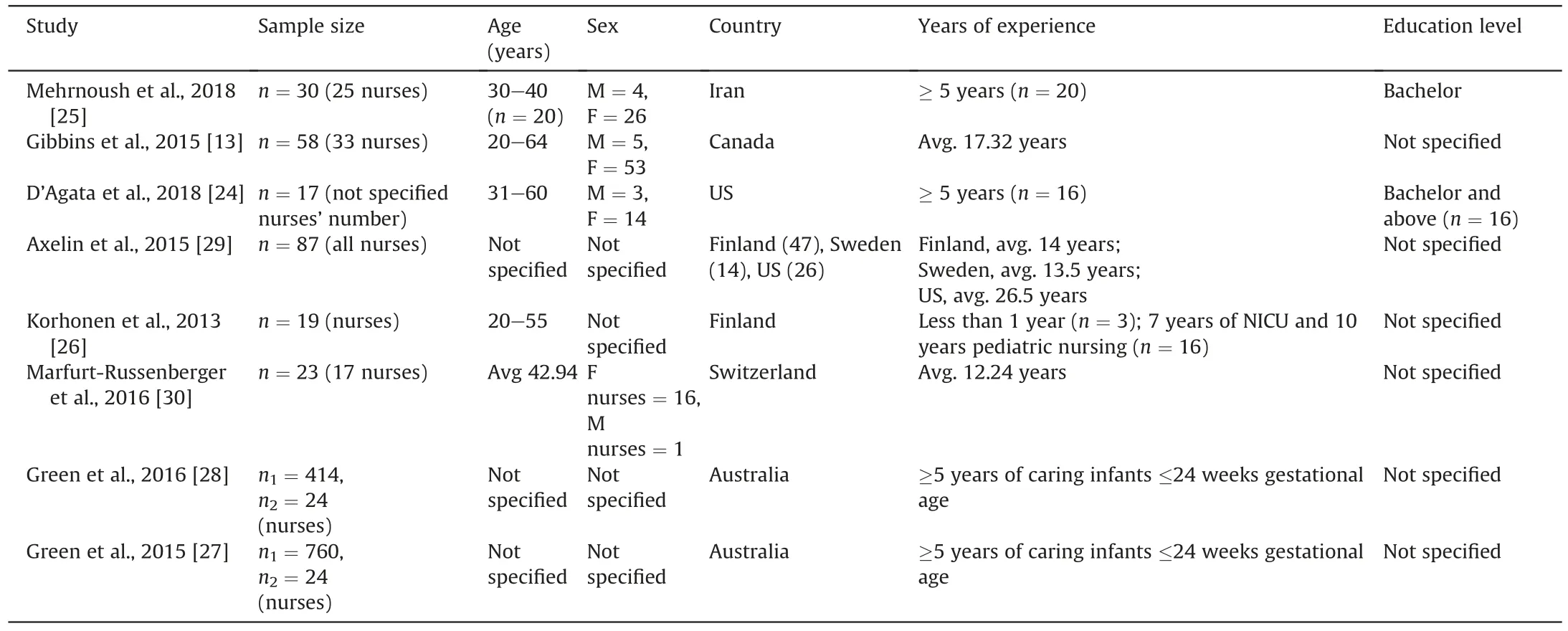
Table 2Demographic characteristics of participants in the individual studies in the meta-ethnography.
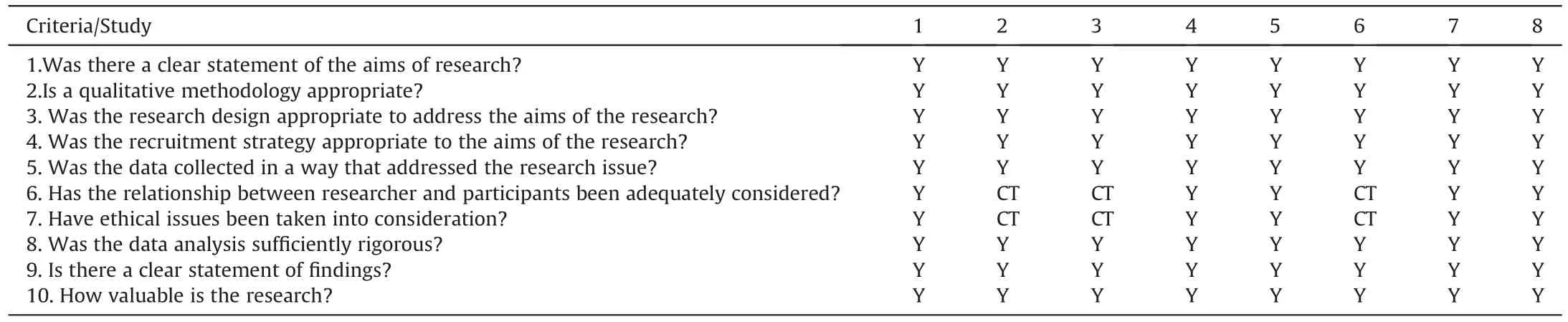
Table 3Quality appraisal of the included studies using the Critical Appraisal Screening Programme (CASP,2020).
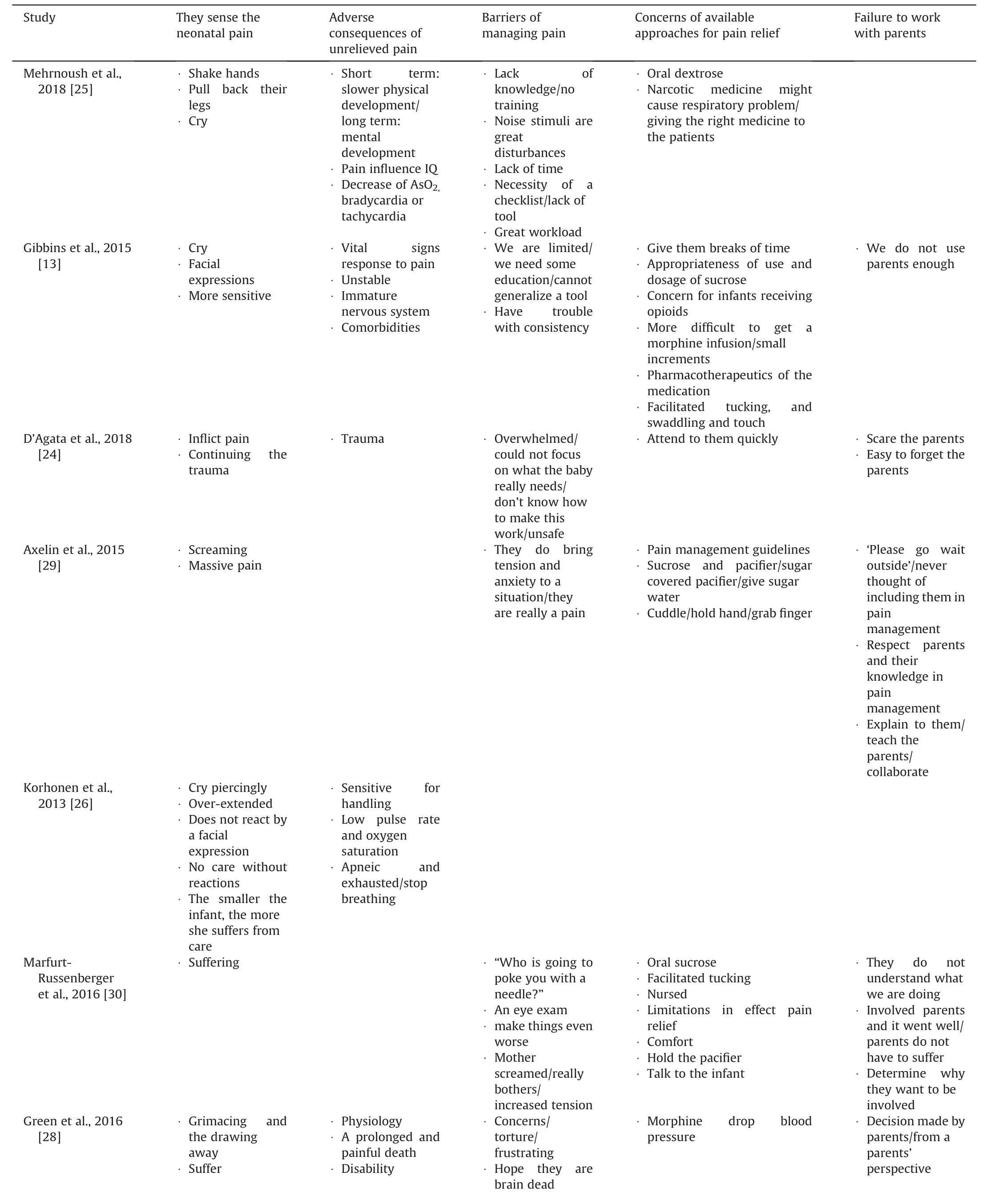
Table 4Individual study metaphors as related to five overarching themes.
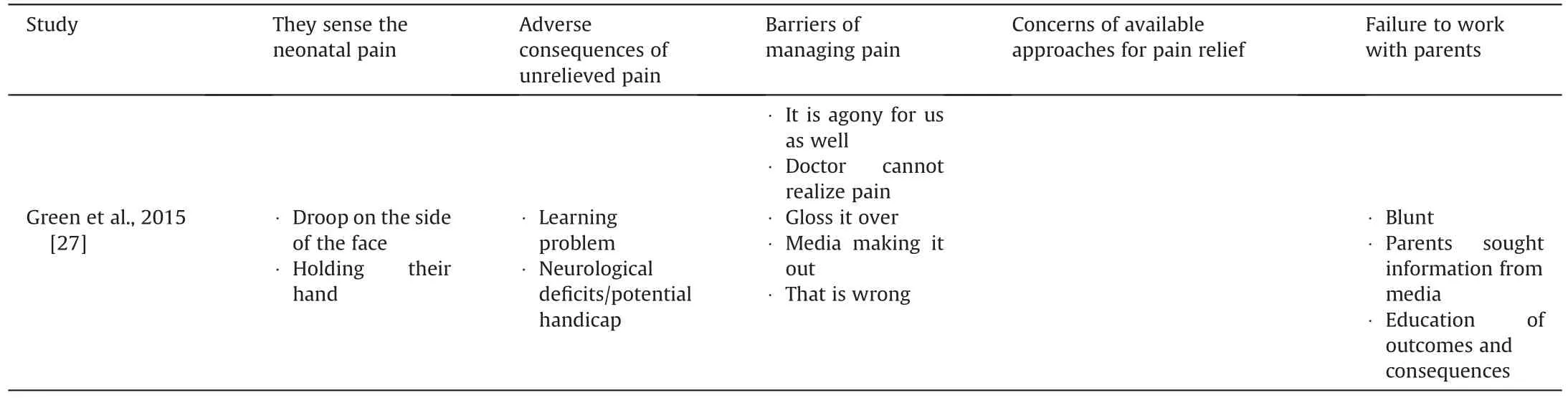
Table 4 (continued)
3.2.Themes of the meta-synthesis
3.2.1.They sense the neonatal pain
Seventeen key metaphors were identified to support that pain was true in preterm infants.It is critical that nurses accepted that preterm infants could feel pain.Their pain indicators could be categorized into facial expressions,body movements,and functional activity,although these indicators were subtle and easy to be ignored[13].The nurses’experience was critical because the cues of pain in preterm infants were ambiguous:“…the 37 weeker can tell us that they are not happy with what we’ve done and they communication that very well to us with their cry,with their face,with their response to us whereas with the little ones it’s a lot harder to interpret their facial expressions ….” [13] Infants’ cry was interpreted as hungry,wet diaper,or stress;however,their cry was a sign of pain to experienced neonatal nurses.One nurse stated that“they would shake their hands or pull back their legs or cry when they feel pain.”[25].
Other nurses understood that infants could have pain because saving the infants’ lives creates much pain that infants could not consent to [24].Some nurses felt that pain experience,to infants,just like trauma: “That mentality isn’t the same as going to war …we’re fighting,we’re battling to save the babies’ lives… but… to me,traumatic is just a severe word.”[24]Although nurses usually have a hard time dealing with these feelings,the understanding that infants are experiencing much pain will help nurses advocate for their patients and their families.
Preterm infants’ characters (low gestational age,low birth weight,immature nervous system,undeveloped immune system,comorbidities)and pain itself would mutually influence each other,complicating preterm infants’ pain experience.Moreover,understand that the smaller the infant was,the more pain he/she was experiencing because of their lowered pain threshold [25].The nurse described these as suffering: “… the smaller the infant the more she suffers from care.” [26] Another nurse said: “I know the researchers said that babies don’t suffer pain because the nerve tracts aren’t myelinated.Don’t tell me that 24 weekers don’t suffer.Just because they don’t remember it and they don’t have the language skills to remember pain,doesn’t mean that they don’t suffer.It’s just that they can’t communicate.” [28]
Many nurses in Korhonen’s study[26]admitted that pain is true in preterm infants even though some preterm infants do not have any facial expressions.They mentioned that as follows: “Her condition becomes worse… if she is in very poor condition,she does not react by a facial expression.” [26] Having low body weight was strongly associated with pain sensitivity.The thin skin of preterm infants with low birth weight,couldn’t protect them from all stimulation,such as temperature variation,diaper changing,or even touching.One nurse stated that they were sensitive to everything: “…They have less fatty tissues,they are…like low birth weight infants are sensitive to everything that you do to them,like the temperature control,they’re sensitive to that…” [13]
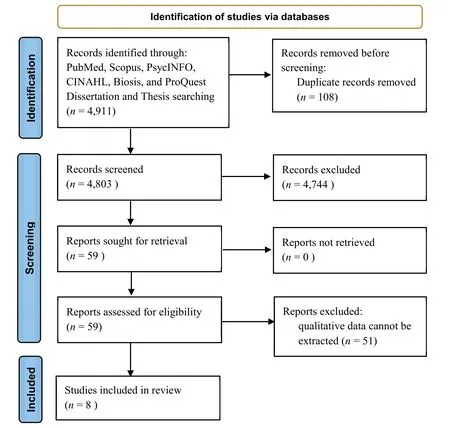
Fig.1.PRISMA flow diagram of the study selection.
3.2.2.Adverse consequences of unrelieved pain
Some nurses believed that pain would impact preterm infants’physiological,neurological,and psychological development during hospitalization and future life.These nurses stated: “Both of them[long and short-term side effects] are expectable.Short-term effects might be observed in slower physical development.Long-term sideeffects might appear in mental development;for instant frequent pain influences IQ of the patient.” [25]
Physical activities were fragile in preterm infants.Painful stimulation made their vital signs such as heart rate,blood pressure,and respiratory rate very unstable.The physical changes might cause short-term or even long-term side effects of pain in preterm infants.
3.2.3.Barriers of managing pain
The obstacles to managing pain in preterm infants are multifaceted.Lacking knowledge or training in pain assessment was mentioned by one nurse:“Another reason is lack of knowledge….we do not know how to deal with these cases.” [25] Nurses who had concerns and uncertainty stated that another reason for barriers of pain management was lacking standard policy to follow,lacking facilities,lacking pain scales,and lacking environmental factors control.Additionally,nurses who were taking care of preterm infants were complaining that too much workload they were bearing.The overwhelming assignment caused their ‘ignorance’ of pain assessment and pain management in infants.In Mehrnoush’s study[25],one nurse stated that:“There is a great workload on the nurses and in some cases,pain is not a priority.”
Further,many nurses were blaming themselves because they inflict painful procedures on vulnerable preterm infants.Nurses were experiencing moral distress and anxiety when they were providing treatment to infants.The pressure from the third party made the nurse’s job even harder.Some nurses complained about the stress caused by the parents’ presence,the pressure from neonatologist,and the misleading information provided by media complicated the misunderstanding of parents.
3.2.4.Concerns of available approaches for pain relief
Although the limited pain control strategies,nurses provided the infants with the necessary support to alleviate their pain.Pain intervention includes pharmaceutical and non-pharmaceutical strategies such as non-nutritive sucking,skin-to-skin kangaroo care,breastfeeding,touching,tucking,holding,talking,etc.Some nurses expressed their concerns about providing both pharmaceutical and non-pharmaceutical interventions to preterm infants.In Mehrnoush’s study[25],nurses described their concerns:“Add to this the fact that it is a narcotic medicine and might cause respiratory problems.” Nurses expressed their uncertainty about whether the standard care would cause pain in babies:“…it is more difficult for us to know with the tiny babies and even with the facilitated tucking,andswaddling and touch we’re not really sure what these babies feel.”[13]
3.2.5.Failure to work with parents
Parents had the power of pain management in preterm infants as well.However,parents were often excluded from pain management or treatment.Nurses pointed out the problem of missing cooperation with parents.In Axelin’s study[29],one nurse said:“A lot of time the doctor says,‘can you please go wait outside?’That way,I never have to deal with the conflict.” The possible reason may be because parents’ existence causes stress.One nurse described this when she said: “ ….when I had to squeeze the heel,the mother screamed.So it all took about twice as long as usual to fill the capillary tube.” [30].
There was an urgent need for cooperation with parents mentioned by some nurses.Better teamwork with parents would positively improve pain management.In Axelin’s study [29],one nurse stated the importance of including parents as team members: “Mothers holding a baby for a heel stick and … I think that’s equally or more effective than being in a warmer or in isolate with sucrose and a pacifier.” Parents’ involvement in pain intervention would benefit the parent-infant bond and increase the efficiency of nurses’ jobs.However,failure working with parents is very common in the NICU and one nurse said: “I think we don’t utilize the parents enough and all of that is getting better but we are certainly not where we should be but I don’t think we utilize the parents enough…and skin to skin enough and breast feeding while we are doing some of these heel pokes or capillary bold sampling or things like that.” [13]
4.Discussion
Meta-synthesis is an important interpretive method to synthesize qualitative findings from primary studies [31].Synthesis is an activity to bring together the separate pieces to form a whole.The synthesis of qualitative findings provides in-depth perception and systematic understanding of the existing phenomenon,knowledge,and experiences.This was the first meta-ethnography to the author’s knowledge focused on nurses’own perspective of caring for preterm infants in pain in the NICU.The findings from this synthesis address on five overarching themes:They sense the neonatal pain;Adverse consequences of unrelieved pain;Barriers of managing pain;Concerns of available approaches for pain relief;and Failure to work with parents.
The first qualitative article discussing preterm infants in pain was published in 1993 [32].This paper confirmed that both physicians and nurses believed that preterm infants experiencing pain and provided proper intervention to relieve the pain[32].Although we excluded this study in our synthesis because it was published more than ten years ago,the major findings in this article showed the historical root of clinical professionals’ perception of pain assessment and pain treatment in preterm infants.Consistent with their findings,our study showed that nurses understand that preterm infants were more vulnerable to pain stimulation,although the sign of pain in preterm infants was subtle or they might not express pain due to their immature nervous system,which was consistent with other study findings [2].The nurses in our study recognized neonatal pain by observing their facial expressions and body response [33].In addition,some nurses could identify unexpressed pain by assessing their heart rate,blood pressure,and respiration rate [33].
Our study found that while most nurses are knowledgeable about the pain in preterm infants,the adverse effects of pain are usually overlooked during infants’ NICU care.Our findings are in accordance with recent studies demonstrating the negative impact of pain on infants’ growth,physical status,immune system function,psychological health,and neurodevelopment [4,33].
Although other health clinicians’ experience is important to evaluate,it is critical to understand nurses’ own perspectives and needs because nurses exert control in pain intervention in the NICU[34].Therefore,we did not include other health professional’s perspectives in our synthesis.The nurses who stated barriers of caring for preterm infants,including lack of education,training,time,tool,policy,consistency,and cooperation with physicians and parents,were consistent with other studies [2,35].Although most nurses showed a positive attitude in pain control in infants,the overwhelming amount of paperwork and other workload are the major reasons nurses ignore pain alleviation in infants,consistent with another finding[36].Our study found that nurses’stress came from their belief that they inflicted the pain and did not get enough emotional support from other health caregivers or parents.Carrying too much stress without detachment could lead to nurses’powerlessness and hopelessness,which warrants relief.This finding is a necessary complement to other findings,focusing on mothers’ stress and infants’ stress [37,38].
To alleviate pain in preterm infants,it is urgent to administer effective pharmaceutical or nonpharmaceutical pain control in preterm infants.However,our study found many challenges faced by nurses to provide pain intervention including uncertainty and inconsistency of medication administration and the risk of adverse events of opioids,which were consistent with other study findings[33,39-41].
Parents’ exclusion in caring for preterm infants in pain is not rare due to nurses’ heavy workload,limited time,stress,and the desire to protect parents from anxiety in our synthesis.Some nurses in our study found that parents can facilitate pain intervention once they were provided enough education and training.This finding is consistent with another study that building rapport between parents and nurses made pain intervention successful in NICU[34].However,some nurses stated that the parents’absence asserted nurses’control of pain management.This finding may indicate the challenges that nurses and parents are facing when establishing their partnership.Our synthesis pointed out the limitation of nurses in providing support and education to parents,requiring further help from other clinicians.The lack of education and training in pain assessment and intervention for nurses themselves also complicated this problem.
Overall,the support to the nurses caring for preterm infants should focus on pain management education and training.The training should also be attainable to other clinicians,including physicians as a partner in pain treatment.To better support powerless nurses,policy change considers optimizing neonatal nurses’ workload,and standardized NICU pain care is urgent:releasing nurses from the overwhelmed paperwork,providing nurses the bedside sheets and necessary facilities,optimizing the environment in the NICU,and offering nurses emotional support such as psych services,and always the extra help from other colleagues when they are overloaded.
There are several limitations of this study.Our study only included eight studies with 254 nurses from seven countries with less diverse ethnicities and educational backgrounds,which cannot be generalized to nurses worldwide.Although we would like to involve parents as a team to help the nurses,our study only focused on mothers’teamwork with nurses,which excluded fathers’role in caring for preterm infants in pain.Additionally,this study did not mention many pharmacological pain interventions that may need future exploration.
5.Conclusion
This meta-ethnography identified nurses’understanding of pain in preterm infants that can be assessed through their facial expressions,body movement,and physiologic responses.Nurses are acknowledged that unrelieved pain can cause developmental deficits in infants.Barriers and challenges when taking care of preterm infants in pain are lack of support such as training,education,policy change,optimized workload,and cooperation from other health professionals.Nurses recognized that building a solid rapport with parents will benefit preterm infants’ health outcomes.Future studies are needed to develop age-specified pain assessment scales,investigate effective pharmaceutical and nonpharmaceutical interventions,manage nurses’ stress in caring for preterm infants,and enhance parents’ roles,including both mother and father,to build a healthy parent-infant bond.
CRediT authorship contribution statement
Tingting Zhao:Conceptualization,Methodology,Validation,Formal analysis,Investigation,Data curation,Writing -original draft,Writing -review &editing,Funding acquisition,Project administration.Angela R.Starkweather:Conceptualization,Methodology,Validation,Investigation,Resources,Data curation,Writing -review &editing.Adam Matson:Conceptualization,Methodology,Validation,Investigation,Resources,Data curation,Writing -review &editing.Shabnam Lainwala:Conceptualization,Methodology,Validation,Investigation,Resources,Writing -review &editing.Wanli Xu:Conceptualization,Methodology,Validation,Writing -review &editing.Xiaomei Cong:Conceptualization,Methodology,Validation,Formal analysis,Investigation,Writing -review&editing,Supervision,Project administration.
Funding
This study was supported by a grant from NIH/NINR Ruth L.Kirschstein National Research Service Award (NRSA) Individual Predoctoral Fellowship(Grant numbers:F31NR019940,PI:Tingting Zhao) and ENRS/Council for the Advancement of Nursing Science Dissertation Award (PI: Tingting Zhao).
Data availability statement
Authors declare the absence of shared data in the present study.
Declaration of competing interest
The authors have declared no conflict of interest.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2022.09.003.
杂志排行
International Journal of Nursing Sciences的其它文章
- Effects of equine-assisted interventions on older adults’ health: A systematic review
- Quality indicators for the care of older adults with disabilities in longterm care facilities based on Maslow’s hierarchy of needs
- Exploring social movement concepts and actions in a knowledge uptake and sustainability context: A concept analysis
- Palliative care needs and symptom burden in younger and older patients with end-stage renal disease undergoing maintenance hemodialysis: A cross-sectional study
- Lived experiences with unmet supportive care needs in pediatric cancer: Perspective of Chinese children and their parents
- Development and validation of a nomogram for predicting the risk of pressure injury in adult patients undergoing abdominal surgery
