Quality indicators for the care of older adults with disabilities in longterm care facilities based on Maslow’s hierarchy of needs
2022-11-05TomeiZhngYingLiuYlingWngChunhuiLiXiyuYngLiTinYinWuLuLinHuilingLi
Tomei Zhng ,Ying Liu ,Yling Wng ,Chunhui Li ,Xiyu Yng ,Li Tin ,b ,Yin Wu ,b,Lu Lin ,b,Huiling Li ,b,*
a School of Nursing,Medical College of Soochow University,Suzhou,China
b The First Affiliated Hospital of Soochow University,Suzhou,China
Keywords:Aged Health care quality indicators Health services for persons with disabilities Long-term care Nursing care Quality of health care
ABSTRACT Purpose: This study aimed to develop quality indicators for the care of older adults with disabilities in long-term care facilities (LTCFs) based on Maslow’s hierarchy of needs.Methods:The draft of the quality indicators was drawn up based on a literature review and research group discussion.The quality indicators were finalized by two rounds of expert consultation (involving 15 experts) using the Delphi method.The Analytic Hierarchy Process was applied to calculate the indicators’ weight.Results:The response rates of the two rounds of consultation were 100% and 93%,and the expert authority coefficients were 0.86 and 0.87.After two rounds of consultation,the expert opinion coordination coefficients of the first-,second-and third-level indicators were 0.42,0.25,and 0.96,respectively(P <0.05),and the variation coefficient was ≤0.25.The final quality indicators for the care of older adults with disabilities in LTCFs included 7 first-level,19 second-level,and 107 third-level indicators.Conclusion:The quality indicators for the care of older adults with disabilities in LTCFs are reliable,scientific,comprehensive,and practical and specify the content of person-centered care needs.This can provide a reference for evaluating and improving care quality in LTCFs.
What is known ?
· Maintaining high care quality of long-term care facilities(LTCFs)is essential for the development of long-term care services.
· Current indicators of care quality are more focused on care outcomes,such as the incidence of pressure injury,physical restraint,and unplanned weight loss.
· Some indicators for the care of older adults with disabilities in long-term care facilities were developed from the perspective of the service provider rather than the perspective of service recipients.
What is new ?
· This study constructed the quality indicators of care service in LTCFs based on Maslow’s hierarchy of needs.
· Services to satisfy physiological needs and safety needs of residents are the most important aspects to evaluate the care quality of LTCFs.
· The care quality indicators also include services meeting residents’ needs of belongingness and love,esteem,cognitive,aesthetic,and self-actualization.
1.Introduction
With the rapid aging of China’s population,the number of older people aged 60 years has reached 264 million,accounting for 18.7%of the total population by the end of 2020[1].The fourth sampling survey on the living conditions of older adults in urban and rural China in 2015 showed that the number of disabled and semidisabled older adults was large,approximately 40.63 million,accounting for 18.3%of the older population[2].Approximately one billion people worldwide have varying degrees of disability,and the incidence of disability increases significantly with age [3].The increasing number of older adults with disabilities(OADs)and the long time they survive after becoming disabled creates a huge demand for long-term care.In addition,with the loss of the ability to take care of themselves,the increase in the number of empty nesters,the change in the pension concept,and the weakening of the family’s role in providing care for older adults,an increasing number of older adults are willing to choose residential care homes(RCHs) for their later life.Driven both by market demand and pension policy support[4],the number and scale of RCHs in China have grown rapidly and have become an important support for the social pension service system.The care quality of long-term care facilities (LTCFs) is directly related to the health status and quality of life of OADs and is also related to potentially preventable hospitalization [5].Therefore,it is an indispensable part of the development of long-term care services [6].
In countries such as the USA[7],Australia[8,9],and Switzerland,several indicators are commonly used to monitor the care quality of LTCFs,including pressure injury,physical restraint,unplanned weight loss,falls and major injuries,and medication management[10].These indicators are more focused on care outcomes,although some can also be considered processes [11].In China,some care quality indicators [12,13] have been developed based on the structure-process-outcome model,which focuses on both care outcomes and processes.In addition,some quality indicators for the care of OADs in LTCFs were developed from the perspective of the provided service,which was based on the service quality model,such as the service quality gap model [14] and customerperceived service quality [15].However,care quality indicators are scarcely considered from the perspective of service recipients,namely,older adults who are disabled,semi-disabled,cognitively impaired,or in need of hospice care.
Maslow classified human needs into five levels [16]: physiological,safety,belongingness&love,esteem,and self-actualization.These were subsequently developed into seven levels with the addition of cognitive and aesthetic needs.This is the most influential and widely used theory for exploring basic human needs.Physiological needs,which refer to psychological drives like hunger and sleep,are usually taken as the starting point of Maslow’s motivation theory.If the physiological needs are relatively well gratified,a new set of needs emerge,which are roughly categorized by Maslow as safety needs.If both physiological and safety needs are fairly well gratified,then the need for higher-level needs such as belongingness and love and esteem will emerge[17].
The majority of residents in LTCFs are older adults with impairments in self-care or cognitive abilities,which requires us to assess the care quality for OADs in LTCFs in a holistic,residentcentered,needs-based manner.Therefore,this study aimed to develop quality indicators based on Maslow’s hierarchy of needs,focusing on OADs and their needs to provide a reference for improving care quality for older adults in LTCFs.
2.Methods
2.1.Design and process
A pre-investigation was conducted to identify the importance and necessity of developing needs-based care quality indicators and diverse care needs of OADs were screened.A list of the questions asked in the interviews is outlined in Supplementary 1 (see Appendix A).
The quality indicators for the care of older adults with disabilities in long-term care facilities were developed in four steps.First,we adopted Maslow’s hierarchy of needs as the guide to establishing a basic framework to develop indicators.The framework included seven domains which formed the first-level indicators:physiological,safety,belongingness &love,esteem,cognitive,aesthetic and self-actualization needs.Second,we conducted a systematic literature search to identify the care needs of OADs and searched the related national guidelines for long-term care in LTCFs.We drafted the initial indicators from screened related literature.Then,we used the Delphi technique to determine final indicators.Finally,we used the Analytic Hierarchy Process(AHP)to assign weights to the indicators.
2.2.Literature review
A systematic literature search was conducted.Four databases,WanFang,China Knowledge Resource Integrated Database (CNKI),MEDLINE via PubMed,and EMBASE,were searched for articles related to the care needs of OADs.Search items included a combination of subject headings,terms,and keywords such as “old adults,”“old people,”“disab*,”“nursing home*,”“institution*,”and“need*.” The data ranged from the database’s inception to December 2021.Search strategies for four databases are provided in Supplementary 2(see Appendix A),with combination of MeSH and free-text terms.Second,we also searched the related national guidelines about LTCFs’care quality on official websites,such as the Ministry of Civil Affairs of the People’s Republic of China,etc.
We set up a research group consisting of two geriatric nursing experts,one doctoral candidate,and two masters of science in nursing,all of whom were familiar with the long-term care of OADs.Two researchers independently screened the literature.Literature were included if they were related to the needs of OADs in LTCFs and excluded if the full text was unavailable.The screening results were cross-checked,and differences between the results were discussed preliminarily.If there were still differences between researchers after discussions,the disagreements were resolved in group discussion.Items related to quality indicators for LTCFs were extracted and collected from selected literature and related guidelines.These items were then assigned to corresponding need hierarchies as the second-level indicators based on Maslow’s hierarchy of needs.Specific indicators were developed as the thirdlevel indicators according to the national guidelines and research group discussion to ensure the measurability and contribution to the second-level indicators.
2.3.Delphi method
Delphi method was used to revise and finalize the care quality indicators.The inclusion criteria for the experts to be consulted in our study included: 1) more than 10 years of work experience in geriatric nursing,rehabilitation nursing,nursing management,geriatric nursing research,and other fields;2)age >30 years;and 3)voluntary participation in this study.According to the above criteria,15 experts were selected to participate in this study.Among the 15 experts,13 were women and 2 were men,2 were Ph.D.,8 had a master’s degree,and 5 had a bachelor’s degree;7 were experts in nursing management,6 in geriatric nursing,1 in quality management and 1 in hospice care.
Firstly,the questionnaire was sent to experts via WeChat or email.The questionnaire included the purpose and significance of this study,fulfillment requirements,the initial draft of the indicators,and basic information of the experts,such as name,sex,age,educational level,professional title,affiliation,years of work,professional field,etc.Experts assigned importance scores to each indicator using a 5-point Likert scale.Secondly,after the questionnaires were collected,data were analyzed.The coefficient of variation was used to calculate the concentration of expert opinions.The smaller the coefficient of variation,the better the concentration of expert opinions.A coefficient of variation ≤0.25 was used as the criterion for the inclusion of the indicators.This study used the coordination coefficient to determine the coordination of expert opinions.Kendall’s W ranges from 0 to 1;the higher the coordination coefficient,the better the coordination of expert opinions.The experts’ suggestions were summarized and discussed,and adjustments were made to the initial draft to form the second draft of the indicators.Finally,the revised quality indicators were sent to the experts for a second round of consultation until their opinions converged.The interval between each round of expert consultation was more than a month.
2.4.Assign weights to the quality indicators
The AHP proposed by Saaty in the early 1970s divided the overall decision-making objectives into three levels: top (goal level),middle(criterion level),and bottom(program level)[18].In this study,goal and criterion levels were identified and analysed.An expert judgment matrix was constructed using pairwise comparison of the mean importance scores in the final round.The square root method was used to calculate and normalize the weights of each indicator.The combined weight was calculated by continual multiplication,which was the product of the original weight of the indicator at this level and the weight of its superiorlevel indicator.The consistency ratio (CR) value was used to determine whether the matrix was internally consistent.A CR value ≤ 0.1 meant that the matrix was internally consistent;otherwise,the judgment matrix had to be adjusted until it passed the consistency test.
2.5.Ethical consideration
This study was reviewed by the Ethics Committee of Soochow University (number: SUDA20210730H01).All participants voluntarily participated in this study.
3.Results
3.1.Quality indicator drafts
A total of 3,286 articles were searched,and 878 duplicates were removed.A total of 2,280 articles were excluded after reading the titles and abstracts,115 articles were excluded after reading the full text,and 13 articles were retained [19-31].Besides,4 guidelines[32-35],were also included after browsing the website of the Ministry of Civil Affairs.Twenty initial second-level indicators were extracted from these 13 articles and 4 guidelines and categorized into seven hierarchies of needs based on Maslow’s theory.Totally 168 third-level indicators were formed with reference to the contents and evaluation methods of the LTCFs care quality guidelines[33,34].After discussion by the research team,a preliminary draft of the quality indicators comprising 7 first-level indicators,20 second-level indicators and 168 third-level indicators was formed.
3.2.Determination of quality indicators
Two rounds of expert consultation were conducted.Fifteen and 14 questionnaires were returned in the first and second rounds of expert consultation,respectively,with response rates of 100% and 93%.
In the first round,12 experts provided constructive suggestions,and 5 experts in the second round did.In the first round of expert consultation,no changes were made to first-level indicators.For second-level indicators,one new item was added,two were deleted,and one was modified.For the third-level indicators,10 new items were added,56 were deleted,one was merged with another,and 14 were modified.In the second round,the first-and second-level indicators remained unchanged.Among the thirdlevel indicators,10 items were modified,6 were deleted,and 8 were merged with others.Finally,quality indicators for OADs care in LTCFs were formed,including 7 first-level,19 second-level,and 107 third-level indicators (See Appendix B).
The authority coefficients of the experts in the two rounds of consultation were 0.86 and 0.87,respectively,indicating high authority of the experts and reliable consultation results.The two rounds of expert consultations in this study had coordination coefficients of 0.23-0.57 and 0.25-0.96,respectively.The chi-square test showed that the difference was statistically significant,indicating that the degree of coordination of expert opinions was good in both rounds of consultation,as detailed in Table 1.The coefficients of variation in the two rounds of expert consultation were all less than 0.25,indicating that the variability in expert opinion concentration was small,as shown in Table 2.The mean importance value was used to determine the importance of the indicators,which ranged from 1 to 5;the higher the score,the more important the indicator.
3.3.Weights to quality indicators
According to the AHP method,the care quality of OADs in LTCFs was identified as the goal level,represented by A in Table 3;the criterion level consisted of the first-,second-and third-level indicators represented by B,C and D,repectively.A total of 24 judgment matrices of these four layers were constructed for this study.The consistency test results for each matrix are presented in Table 3.The CR value of each judgment matrix was less than 0.1,indicating no logical errors.Table 4 lists the first-and second-level quality indicators and their weight coefficients.
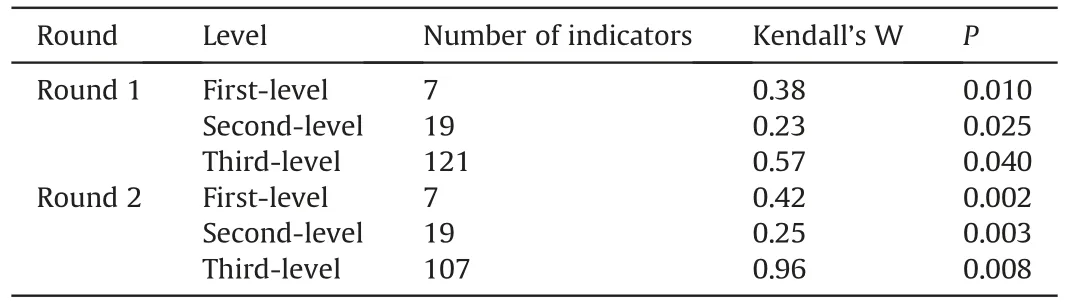
Table 1The coordination degree of expert opinions.
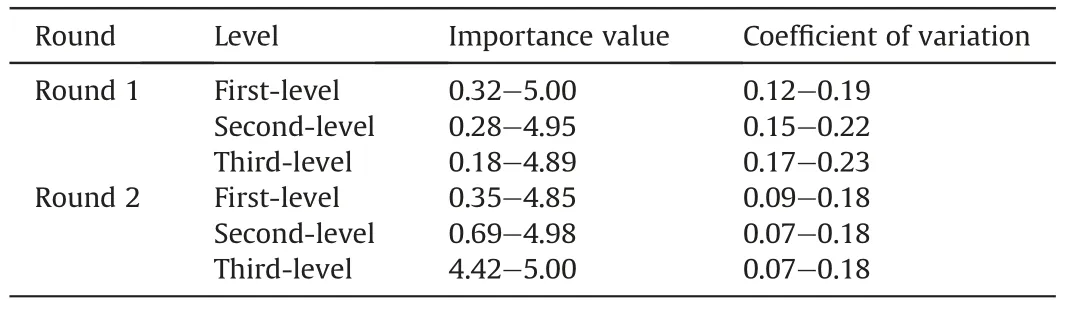
Table 2The concentration degree of expert opinions.
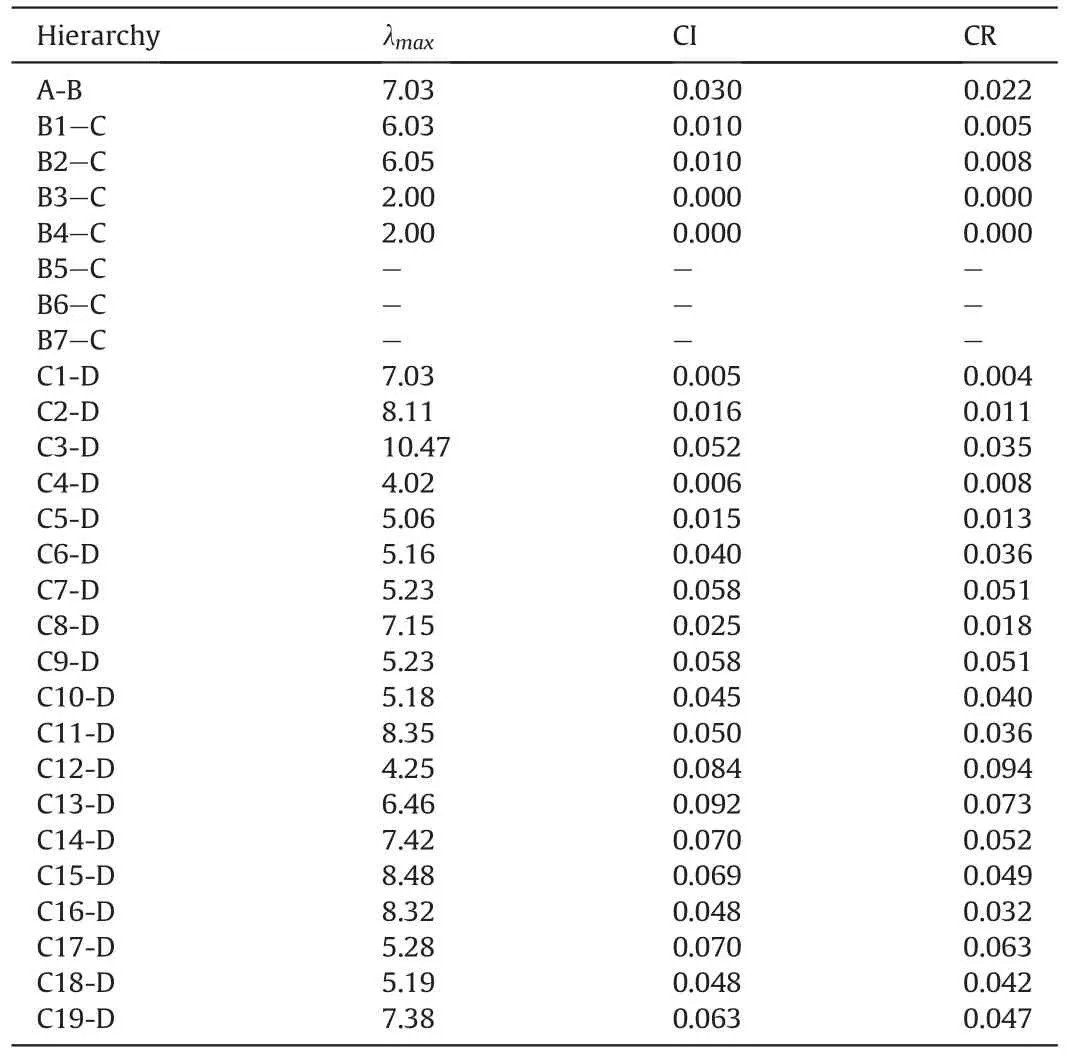
Table 3The results of the consistency test of each judgment matrix.
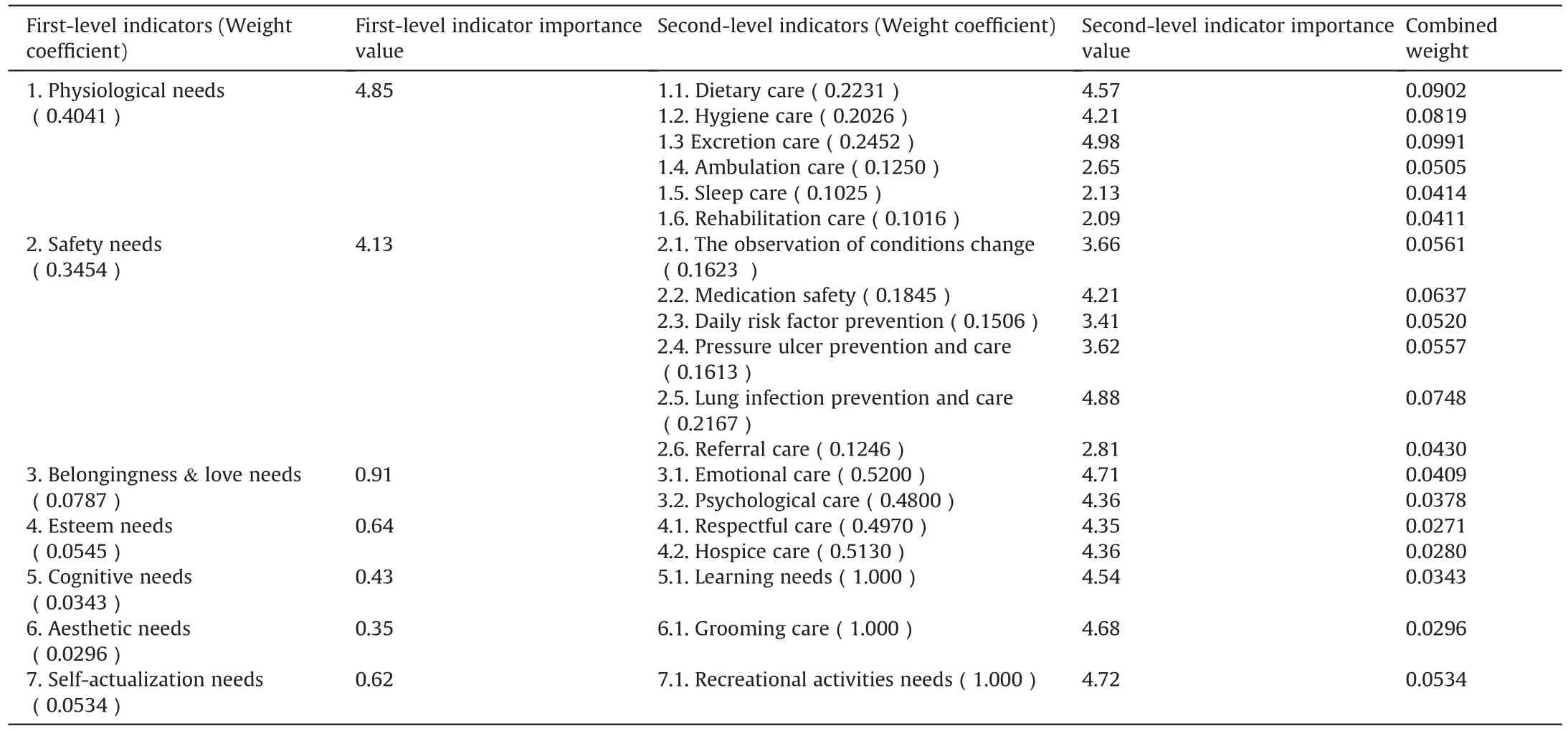
Table 4The first-and second-level quality indicators for the care of older adults with disabilities in long-term care facilities based on Maslow’s hierarchy of needs and weight coefficients.
4.Discussion
4.1.Characteristics of the quality indicators for OADs care in LTCFs
Overall,the quality indicators of OADs care in LTCFs developed in this study are person-centered,needs-based,scientific,authoritative,comprehensive,and practical.
In this study,we combined a systematic literature review,Delphi and the AHP method to develop quality indicators of care and confirmed the weight coefficient of each indicator.These quality indicators embodied the contributions of previous scholars,the experience and expertise of Delphi consultation experts,and the science of quantified measurement.The experts based their judgment on their rich clinical experience and profound theoretical foundation on the research topic.In addition,AHP can analyze an expert’s subjective judgment in mathematical form and conduct multi-objective decision-making analysis[18];therefore,compared with other long-term care quality evaluation indicators[28,31],ourstudy not only determined the care content based on the needs of OADs but also determined the weight of each indicator and its superior indicators.Therefore,the methods adopted in this study are both scientific and effective.
In the Delphi process,this study took full account of the experts’areas of expertise,research direction,work experience,and educational background.The questionnaire recovery rates for the two rounds of expert consultation were 100%and 93%,respectively.Twelve experts and five experts provided constructive opinions during the two rounds of the expert consultation.These results indicate that the experts had high enthusiasm for participating in this study.It is generally considered that an expert authority coefficient ≥0.7 is acceptable,and ≥0.8 suggests that the expert has a high degree of certainty about the content.The expert authority coefficients of the two rounds of expert consultation were 0.87 and 0.86,respectively,indicating a high degree of expert authority in this research area.The coordination coefficients of the two rounds of expert consultation were 0.23-0.57 and 0.25-0.96,respectively,both of which were statistically significant,indicating the expert opinions tended to be consistent and well-coordinated.Therefore,the quality indicators in this study had a certain degree of credibility and authority.
Guided by Maslow’s hierarchy of needs [16],this study has developed quality indicators covering the needs of OADs,ranging from low-level needs such as physiological and safety needs,to high-level needs such as cognitive and aesthetic needs.First,compared with the existing quality indicators,the quality indicators in this study could provide a new and comprehensive perspective to evaluate the care quality of OADs in LTCFs.A previous study showed that the high care quality of LTCFs should include comfortable living,medical rehabilitation,and a social environment for older adults,providing continuous care to improve their health outcomes and meet their explicit and implicit needs [36].The indicators developed by Liu et al.included three main aspects:basic activities of daily living(BADL),instrumental activities of daily living(IADL)and medical care[31].The indicators in this study are mainly focused on the lower level of needs,but more studies suggested that higher-level needs be warranted,such as the need to establish relationships with family members so as to make residents feel a sense of belonging and importance [37],solving psychological problems [38,39],mutual respect between older adults and RCH staff [37],learning and wanting to be involved in discussions about their own care [40],joining creative and educational activities,and games to fulfill their own values[40].Therefore,the care quality indicators in our study were comprehensive and they support the person-centered idea for residents who have lost all or part of their independence in daily life.Second,the three levels of quality indicators developed in this study were tailored to the OADs in LTCFs,so they are more focused and detailed.For example,the quality indicators system developed by Pi et al.was from a management perspective and could be applied in long-term care for all disabled older adults in different settings [12].Cao et al.[28] used medication guidance and care indicators,which need further details.In our study,the third-level indicators make the evaluation measurable and operational.
From the weight results,it can be seen that the ranking of the first-level indicators,as perceived by the experts,were physiological needs (0.4041),safety needs (0.3454),belongingness and love needs (0.0787),esteem needs (0.0545),self-actualization needs(0.0534),cognitive needs (0.0343),and aesthetic needs (0.0296).
The physiological needs were ranked the first,which showed that the most essential aspect in determining the quality of longterm care for OADs is the care of physiological needs.This is consistent with the fact that physiological needs are the most primitive and basic needs of human beings in Maslow’s hierarchy of needs [16].In our study,the physiological needs,that is,the basic needs to maintain the lives of OADs were considered to be needs of dietary,hygiene,excretion,ambulation,sleep,and rehabilitation care.Among them,excretion care,dietary care and cleaning care had the top three weights,which is consistent with the previous studies [12,28,31].For example,Liu et al.’s study showed that the average importance value of dietary and excretion needs were the most important indicators of daily life needs [31].Pi et al.[12]classified hygiene,diet,and excretion care as part of daily life care,with high weighting under link quality.In this study,we focused on OADs with impaired activities of daily living and cognition;therefore,ambulation and rehabilitation care were also included as basic needs,such as choosing the appropriate method of movement according to the condition of older adults and moving them correctly.
The weight of safety needs was ranked the second.Ensuring safety is essential to promoting a better prognosis and improving the quality of care for older adults.Using the “three-dimensional quality structure” model as the theoretical framework,the quality indicators of long-term care quality for OADs,developed by Pi et al.[12],also included nursing safety,which is consistent with the results of this study.The weights of the indicators under safety needs were in the following order: prevention and care of pulmonary infections,medication safety,observation and monitoring of residents’ condition,prevention and care of pressure ulcers,daily riskfactor control and referral care.The indicator content of safety needs is similar to that in previous studies [12,28].The weight of“prevention and care of pulmonary infections” was ranked first under the safety needs indicator.This may be because pulmonary infections are the most common infectious diseases in older adults.Older patients with pulmonary infections are prone to multiple organ dysfunction syndromes [41];when it occurs,clinical treatment is often difficult,and mortality is high.This implies that prevention and care of pulmonary infections are key indicators of care quality,in line with a previous study [12].In contrast to previous studies [28,31],we used a referral-care indicator.Once the disease in older adults worsens,they need to be transferred to the hospital for treatment.Timely and high-quality referrals also play key role in the follow-up prognosis of older adults.
Moreover,for indicators under physiological and safety needs,they revealed the idea of prevention first.For example,compared with Xu et al.’s study [42],indicators of physiological needs in our study were not in terms of care outcomes,such as the incidence of fecal or urinary incontinence but rather an assessment of the care process to ensure the comfort of older adults,such as assessment of defecation,management of abnormal defecation and related cleaning work.
In higher-level needs,the importance values of belongingness and love,esteem,cognitive,aesthetic and self-actualization needs in our study are obviously lower than those of social,spiritual,entertainment and learning needs,which belong to higher-level needs in other studies [28,31].The low importance values also lead to low weight for high-level needs.Although the weights of these five first-level indicators were low,we retained them in the quality indicators for the sake of meeting the needs of older adults as a whole.This could also be understood.First,in Maslow’s hierarchy of needs,high-level needs are typically considered when lowlevel needs are gratified.For OADs in LTCFs,physiological and safety needs are the most fundamental,and higher-level needs might emerge if the basic needs are gratified.Second,the number and scale of LTCFs such as RCHs in China have grown rapidly.However,the care team for OADs in China’s LTCFs mainly consists of care workers for the aged.They face the dilemma of high work intensity,low salary and low professional identity,and most are older,lack an educational background and have a high turnover rate [43].These make them mainly engaged in physical work,such as basic daily life care,and hardly provide the care of higher-level needs for OADs.
4.2.Limitations and implications
To our knowledge,this study is the first one to apply Maslow’s hierarchy of needs to construct the framework of care quality indicators for OADs in LTCFs.Although this study developed a comprehensive and practical care quality indicator system,it has some limitations.This study paid more attention to practical items and included 107 third-level indicators which make the measurement easy,but using it will be time-consuming,which requires the evaluator to carefully observe care activities in the LTCFs and rate the indicators to ensure accurate measurement.Applicability and sensitivity of a set of quality indicators should be tested before practical application.We will perform further studies to validate and update the set of indicators in the future.
5.Conclusion
Based on Maslow’s hierarchy of needs,combined with an extensive literature review,expert consultation,and AHP methods,this study constructed a scientific quality indicator system for the long-term care of OADs in LTCFs.It consists of 7 first-level,19 second-level and 107 third-level indicators,which are measurable and operational.The quality indicator system can be used to evaluate care quality in LTCFs and identify problems in the process of longterm care services.This is conducive to further improving the quality of life of OADs,providing reference standards for the services of caregivers,and providing a reference for the supervision and management of long-term care quality in LTCFs.
Funding
This study was funded by the National Natural Science Foundation of China(Grant No.72074164);Chinese Academy of Medical Sciences(Grant No.2020-JKCS-024).
CRediT authorship contribution statement
Taomei Zhang:Conceptualization,Methodology,Software,Writing -original draft,preparation,Writing -review &editing,Visualization,Project administration.Ying Liu:Conceptualization,Methodology,Software,Investigation,Data curation,Writing -original draft,preparation.Yaling Wang:Conceptualization,Methodology,Validation,Investigation,Writing-review&editing,Project administration.Chunhui Li:Methodology,Software,Validation,Resources,Visualization.Xiyu Yang:Software,Validation,Investigation,Data curation.Li Tian:Conceptualization,Methodology,Validation,Resources,Visualization.Yin Wu:Conceptualization,Methodology,Software,Investigation,Visualization.Lu Lin:Conceptualization,Methodology,Validation,Resources,Writing -review &editing,Project administration,Funding acquisition.Huiling Li:Conceptualization,Validation,Resources,Writing -review &editing,Supervision,Project administration,Funding acquisition.
Declaration of competing interest
The author(s) declared no potential conflicts of interest with respect to the research,authorship,and/or publication of this article.
Acknowledgments
We would like to express our gratitude to the experts that joined in our research.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2022.09.012.
杂志排行
International Journal of Nursing Sciences的其它文章
- Effects of equine-assisted interventions on older adults’ health: A systematic review
- Multicenter application of a nursing workload measurement scale in adult hospitalization units
- Exploring social movement concepts and actions in a knowledge uptake and sustainability context: A concept analysis
- Palliative care needs and symptom burden in younger and older patients with end-stage renal disease undergoing maintenance hemodialysis: A cross-sectional study
- Lived experiences with unmet supportive care needs in pediatric cancer: Perspective of Chinese children and their parents
- Development and validation of a nomogram for predicting the risk of pressure injury in adult patients undergoing abdominal surgery
