A comprehensive health education plus monitoring support program for older adults with knee osteoarthritis coexisting with overweight and type 2 diabetes
2022-11-05SuprAreeUeInthirRoopswngYuweeSroonPhihprornYounghroenBsiBelzVirojKwinwonggowit
Supr Aree-Ue ,Inthir Roopswng ,* ,Yuwee Sroon ,Phihprorn Younghroen ,Bsi Belz ,Viroj Kwinwonggowit
a Ramathibodi School of Nursing,Faculty of Medicine Ramathibodi Hospital,Mahidol University,Bangkok,Thailand
b Department of Nursing,Amnatcharoen Campus,Mahidol University,Amnatcharoen,Thailand
c School of Nursing,University of Washington,Seattle,WA,USA
d Department of Orthopaedic,Faculty of Medicine Ramathibodi Hospital,Mahidol University,Bangkok,Thailand
Keywords:Aged Community Diabetes Health education Knee osteoarthritis Overweight Volunteers
ABSTRACT Objectives: To examine the patient outcomes of a comprehensive health education plus village health volunteer monitoring support program on older adults with knee osteoarthritis who are overweight and have type 2 diabetes.Methods:Quasi-experimental,two-group,pretest-posttest design was applied.Using random geographic cluster sampling,older adults who met the inclusion criteria were assigned to two groups,62 in the intervention group and 71 in the control group.The intervention group received the comprehensive health education plus village health volunteer monitoring support program.The control group received only the comprehensive health education program.Study outcomes,including blood glucose level,knee pain and range of motion,body weight,physical ability (Timed Up and Go Test),fatigue,depressive symptoms,quality of sleep,and quality of life,were assessed at baseline,3 months,and 6 months after enrollment and analyzed using descriptive statistics and multivariate analysis of variance.Results:One hundred and ten participants completed the study (55 participants in each group).Most patient outcomes in the two groups showed general improvement with statistical significance(P ≤0.001): pain decreased,physical ability improved,less depressive symptoms and fatigue,quality of life and sleep improved.The interaction effect(the group and time)demonstrated statistically significant differences between the intervention and control groups on pain,knee range of motion,and fatigue according to each time follow-up (P <0.001).Conclusions:The comprehensive health education plus village health volunteer monitoring support program promotes good patient outcomes in this population.The integrated health education resource and support for older adults with knee osteoarthritis and type 2 diabetes is an effective,non-surgical treatment that highlights professional nursing roles and non-professional roles-village health volunteers.Nurses should consider implementing a health education plus monitoring support program to mitigate the effects of chronic diseases and improve patients’ quality of life.
What is known?
· Integrating theory,evidence,and resource-based health interventions to promote health and equity for older adults with chronic illness is a significant role for nurses in the community and clinical practice.
· Comprehensive theoretical-based interventions to promote healthy behaviors would be more impactful in reducing symptoms associated with knee osteoarthritis.
· Less is known about integrating local healthcare resources to improve outcomes and maintain adherence to healthy behaviors of older adults with knee osteoarthritis coexisting with being overweight and type 2 diabetes.
What is new?
· Implementing comprehensive health education plus village health volunteer monitoring support-non-surgical treatments-improves patient outcomes in older adults with knee osteoarthritis and type 2 diabetes who are overweight.
· Disseminating a health education intervention embedded in community healthcare resources in a low-middle income country highlights both health volunteers and nursing roles in enhancing care quality for older adults with chronic illness.
1.Introduction
In older adults with knee osteoarthritis (KOA),there is a great need to provide effective care for promoting health that goes beyond hospitals or traditional services,particularly for those with coexisting conditions.According to the prevalence and coexistence of KOA,a common coexisting condition is type 2 diabetes mellitus(T2DM),making KOA more difficult to manage [1-3].T2DM not only shares risk factors with osteoarthritis [4,5],but also its pathological pathways influence inflammation processes and increase adverse outcomes [6].Moreover,being overweight or obese is prevalent in older adults with KOA and T2DM,and it aggravates the risks of developing KOA symptoms and intensifying severity [4,5].The combination of coexisting conditions-T2DM and increased body weight-are more likely to increase risks and alter joint loading resulting in KOA.A combination of being overweight and having T2DM seems to be a characteristic of older adults with KOA;however,the pathogenic interplay among KOA,T2DM and being overweight or obese is complex and remains elusive [4,7].Thus,effective management is needed to prevent disease progression and promote health in this population-older adults with KOA and T2DM who are overweight.
Older adults with KOA who both are overweight or obese and have T2DM are prone to develop more physical and mental suffering [8,9].Common unfavorable health outcomes in this population are pain,physical disability,depressive symptoms,sleep disturbance,disability,and increased care demands and/or dependency[1,8,9]that result in reduced quality of life(QOL)[10,11].For severe KOA progression,surgery is often the treatment of choice,yet the costs of care are substantial;and not all physical function and mobility are regained[1].Efficient management with respect to individual situations is challenging for nurses and other healthcare providers.Reducing the cost of care in addition to using an effective non-surgical intervention (e.g.,lifestyle modification and quadriceps exercise) would be preferred to improve physical functioning,alleviate mental suffering,and enhance the QOL for this population [12].Remarkably,consistent effort is required to adhere to healthy behaviors;thus,considering the personal context may lead to better care.Due to an individual’s perception of their living situation pertaining to social norms,cultural and contextual values,socio-cultural context,and environment affects both personal behaviors and QOL [13].Therefore,comprehensive interventions that combine socio-cultural aspects and available community resources may improve adherence,thereby enhancing long-term healthy behaviors and QOL.However,evidence has demonstrated that current interventions lack comprehensiveness and are less theoretically oriented[14].Still,the value of the sociocultural context for care and local community resources has remained speculative for sustaining healthy behavior change and promoting the QOL [15],particularly in overweight older adults with KOA and T2DM who reside in Thailand.
Numerous multidimensional interventions-multicomponent or multifactor interventions-promoting healthy behaviors and QOL have been developed and led by nurses or a member of the multidisciplinary team [16-19].Interventions to promote healthy behaviors (e.g.,diet control,exercise,and lifestyle modification)have been beneficial in reducing KOA problems as well as producing enhanced joint health [17,18] and reducing the risk of escalating knee pain [19] for better functional performance.These types of interventions have also been effective for T2DM[16].Thus,ameliorating further chronic illness and delaying functional decline and dependency for older adults with KOA who are overweight or obese and T2DM would be optimal [20].Continuing care with compelling motivation is essential for promoting healthy behaviors;highly-motivated individuals are more likely to adhere to interventions [16-19].However,interventions that integrate family involvement for enhanced motivation and healthy behavior change may be less advantageous to older adults living alone with no family support or equality of resources.Since dependent older adults seem to increase,collaboration with the local healthcare resources-healthcare personnel-may have the edge over others in monitoring,promoting health,and ensuring care equity [15].Additionally,current evidence suggests that comprehensive health education with theoretically based interventions is necessary for improving care,particularly for the KOA population [14].Thus,applying comprehensive health education intervention with local healthcare personnel may fill gaps in care.However,there is a paucity of evidence evaluating health education interventions monitored by local healthcare resources.What is not yet clear is the impact of integrating local community resources-other healthcare personnel such as village health volunteers-monitoring health outcomes.Therefore,providing interventions involving health education and care that integrates local healthcare resources (e.g.,nurses and village health volunteers),especially in rural areas,would make a valuable contribution in low to middle-income countries.
Effective practical interventions to prevent dependency and disability are essential for KOA in older adults;however,the presence of coexisting conditions makes KOA more challenging to maximize care [1-3].Thailand is similar to the worldwide population regarding the complexity of KOA and coexisting conditions-T2DM and overweight/obesity.The prevalence of KOA in Thailand has been shown to range from 9.0%to 64.7%depending on the geographic area [2,3].KOA mostly occurs with coexisting morbidity,particularly T2DM.For T2DM,recent evidence revealed that pathological pathways-chronic hyperglycemia and insulin resistance-significantly influence the inflammation processes and increase adverse outcomes in the osteoarthritis population [6].Additionally,T2DM shares risk factors with osteoarthritis[4,5];the prevalence of older people diagnosed with both KOA and T2DM continues to increase [1-3].Notably,the conundrum of KOA and T2DM seems more complex in overweight or obese older adults.Evidence has demonstrated that older adults with KOA and T2DM who are overweight or obese report greater KOA progression [21].Obesity or being overweight is a significant risk factor influencing pro-inflammatory chemicals and insulin resistance,which contribute to the development and suffering of KOA and T2DM.Hence,a person with KOA who experienced T2DM with increasing body weight is more likely to increase the risk of severe arthritis and altered joint loading resulting in a poor prognosis of KOA.Suffering from KOA severity,chronic pain,and poor outcomes are not only associated with,but also shared influenced by both T2DM and being overweight or obese [4-6].Coexisting conditions of T2DM and obesity or being overweight is predominant in older adults with KOA leading to increased risk of dependency,long-term care needs,and poor QOL.Although a few studies have been conducted,the problems of older adults with KOA coexisting with overweight/obese and T2DM have not been sufficiently explored for improving care.Promoting health outcomes in this population requires initiatives that go beyond hospital services;thus,incorporating community resources and inter-sector health service collaborations may be essential.Hence,integrative interventions that focus on risk factors,resource management,and sustaining healthy behaviors to reduce the KOA burden are needed.
Many theory-informed behavior change interventions have been broadly developed to enhance positive health outcomes[18,22],but success in promoting sustainable healthy behaviors in chronic illness seems more challenging.Of those interventions,retention and intervention adherence are important issues for older adults who undertake an intervention to change behavior and improve health outcomes.However,the rate of adherence to healthy behaviors,particularly exercise,tends to be low in Thailand[22].The social cognitive theory posits that enhancing adherence and goal-oriented motivation should focus not only on individual factors,but also on the environment and socio-structural factors for strengthening long-term healthy behavior change [23].Several factors determine behavioral changes and are pivotal in promoting health (e.g.,the reciprocal associations between personal,environmental,and behavioral factors)[24].The core determinants that translate into healthy behaviors in terms of health promotion and disease prevention are knowledge,perceived self-efficacy,perceived outcome expectations,goals,and socio-structural factors.Interventions that promote the adherence to achieve healthy habits in older adults and that integrate community-based resources and family members as socio-structural factors,may promote sustainable healthy behaviors.
Blending local community resources and socio-cultural contexts may have more advantages in increased adherence and sustained changes;notably,the availability of resources may vary across geographical locations.Access to community-based resources in Thailand comes from village health volunteers.Established in the 1960s,the health volunteers form part of Thailand’s comprehensive health system[15].The country is divided into regional geopolitical units,the largest being provinces.Provinces are comprised of districts and sub-districts,in which cities/villages are located.The subdistricts have health promotion hospitals that provide primary health care services.Affiliated with the health promotion hospitals are the village health volunteers who provide support to villagers,collaborate with health care providers,and are frontline workers in promoting primary health care for community-dwelling populations.Therefore,integrating the valuable community resource-a village health volunteer-with a health education intervention might maximize cost-effective care [15].As vital primary health community resources,the village health volunteers monitor and support older adults in carrying out health behaviors that achieve positive and sustainable health outcomes.
The social cognitive theory best explains the interactions between the individual,the environment,and their behavior and the relationship of these factors in promoting behavior change.Several intervention studies have used Bandura’s social cognitive theory as a framework to guide behavior change,such as exercise,physical activity,and nutritional consumption [25].However,few studies have examined these factors in older adults with KOA who are overweight and have T2DM.Thus,the purpose of the study was to evaluate effects of a comprehensive health education plus village health volunteer monitoring support program on clinical and patient outcomes of community-dwelling,older adults with KOA coexisting with being overweight and T2DM in residents of Thailand.More specifically,the study’s aim was to investigate the interaction effects of intervention and times (6-month follow-up)on outcomes of a comprehensive health education program that included exercise (walking and muscle strengthening),and nutrition plus village health volunteer monitoring support program.As an intervention,comprehensive health education program was integrated with the Thai village health volunteer monitoring support roles for primary and secondary prevention of KOA with threetime follow-ups.
2.Methods
2.1.Study design and setting
A quasi-experimental,cluster random assignment,two-group,pretest-posttest research design was conducted in accordance with the TREND statement.We randomly recruited communitydwelling older adults with KOA from 12 sub-districts in a large province in upper northeastern Thailand from January 2019 to February 2019.Potential participants included older adults who visited a local health promotion hospital for a health check-up and those who were telephone screened by four nurse research assistants.To avoid cross-contamination during the intervention,the 12 sub-districts were divided into two areas,southern and northern parts.Based on geographical locations (southern or northern),eligible participants were assigned to either the intervention or the control group (Fig.1).
2.2.Participants
The target population was Thai older adults,aged 60 years and over,diagnosed with KOA using symptomatic criteria based on the American Colleague of Rheumatology [26] (age ≥50 years,knee pain,morning stiffness <30 min,and crepitation on knee motion),diagnosed with T2DM controlled by oral medications,had a body mass index of 23.00-24.99 kg/m2(using Asian body mass index for Thais),could perform activities of daily living independently,and expressed willingness to volunteer for the study.Participants were excluded if they had had knee surgeries (e.g.,total knee arthroplasty,knee arthrotomy),secondary KOA (e.g.,rheumatoid arthritis),received a steroid or hyaluronic acid intra-articular knee joint injections within the past 3 months,severe comorbidities(e.g.,history of myocardial infarction),cognitive impairment,or high risk of falls (information obtained from screening health records of the health promotion hospital).
Using G*Power 3.1.9.2 for Windows,we estimated the sample size to be 102 participants based on a median effect size of 0.40[18],a significance level of 0.05,and a power of 0.80 [27].With an estimated 10% added to account for possible participant dropouts,the targeted sample size was about 112 participants to be randomly assigned to intervention and control groups.
2.3.Intervention protocol
The intervention of comprehensive health education plus monitoring support from village health volunteers was developed using social cognitive theory [23] and modified from a previous study that had not included health volunteers[18].For participants in the intervention group,the study began with a 3-consecutive day health education workshop (see Appendix A).Following the workshop,the participants undertook an exercise regimen at least 3 days per week that consisted of brisk walking and quadriceps muscle strengthening exercises,targeting both cardiovascular and musculoskeletal systems.Participants established their preliminary plans and goals to complete their exercise assignments.For the first one to two weeks,participants exercised brisk walking for 20 min per day for 3 days a week.The trained village health volunteers(one per village with a total of 11 persons who were specifically trained in how to support,assist,and monitor participants in adhering to the study protocol with safety concerns) led the participants in the brisk walking and muscle strengthening exercises,then monitored and helped them to achieve their goals by acting as peer walking or performing muscle strengthening with them.
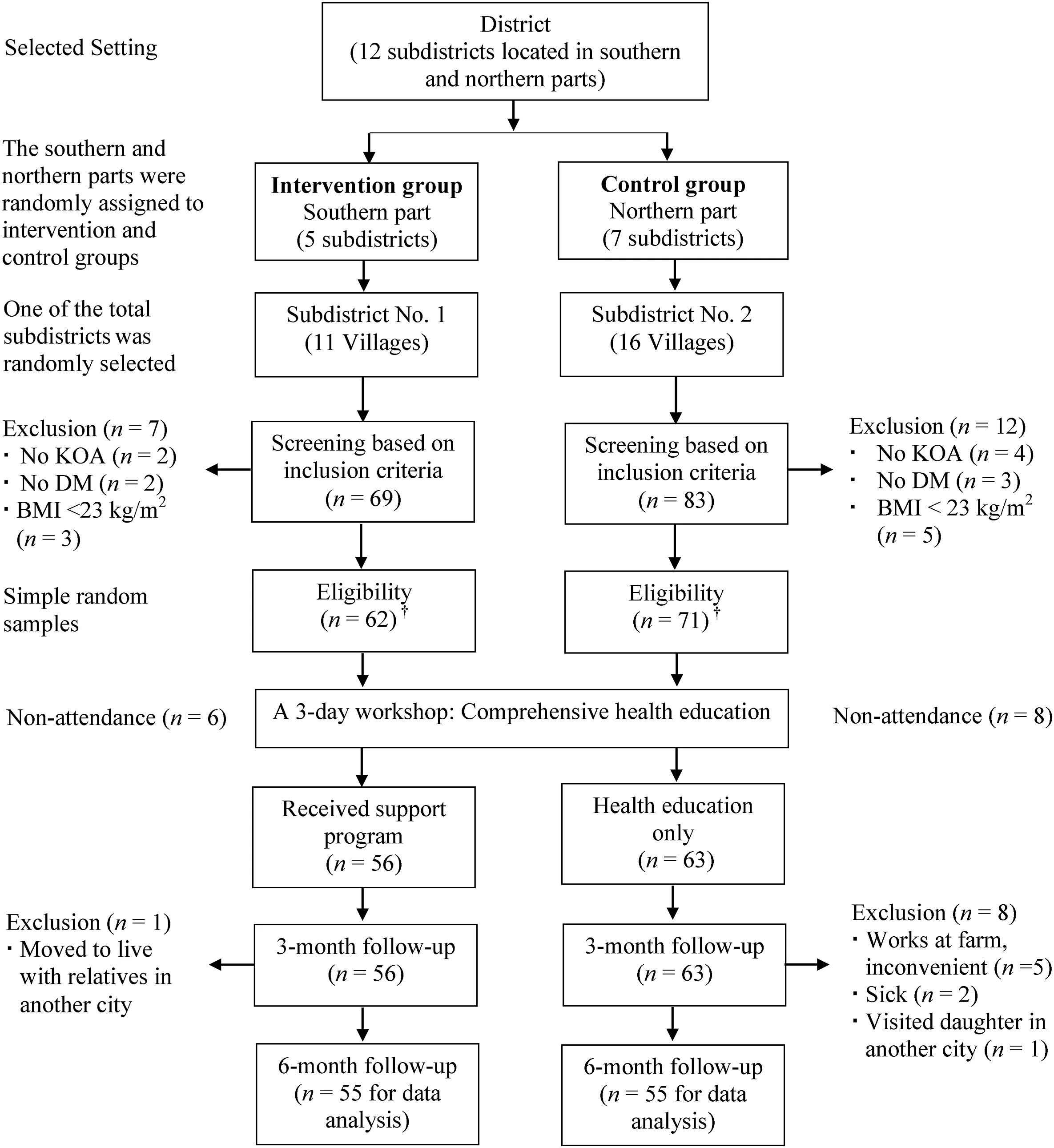
Fig.1.Flow chart of setting and sample selection.
In the third to fourth weeks,the walking exercise increased to 30 min per day for 3 days a week.In the fifth week through 6 months,the daily exercise increased in frequency to 30 min for 5 days a week,or 150 min a week,under the leadership and support of the village health volunteers [16,18].
To strengthen muscles,participants performed 10 cycles of strengthening quadriceps per session,with three sessions each day for at least 3 days a week.Additionally,participants received training on how to calculate caloric intake and were taught that they should consume less than their daily caloric requirement,but not under 5,040 kJ (1,200 kcal) daily [18].To determine whether they had met their goals,participants kept daily exercise and dietary logs with help from village health volunteers and family members.
Participants in the control group also started with a 3-day health education workshop.After the workshop,they were encouraged to follow the same regimen of brisk walking,muscle strengthening,and dietary consumption outlined for the intervention group.However,there were no village health volunteers to provide leadership and support to ensure they met their goals.Family members who wanted to attend the workshop and assist them could do so independently.Additionally,safety concerns regarding any exercise and walking were also emphasized during the 3-day health education workshop.
2.4.Measures
2.4.1.Demographic characteristics and health information questionnaire
A researcher-developed questionnaire elicited information about participants’demographic characteristics,including age,sex,marital status,education level,sufficient incomes,exercise behavior,and health status (e.g.,comorbidities,knee pain selfmanagement,and strategies to control diabetes).
2.4.2.An Accu-Chek
An Accu-Chek (Roche Diagnostic,Thailand) is an instrument that tests proximal sugar levels,reporting the average blood glucose level in mg/dl.Blood was collected from the fingertip 1-2 h after breakfast.Blood glucose levels >180 mg/dl (10.0 mmol/L)were considered high.
2.4.3.Numeric rating scale for pain
The pain scale was used to measure knee pain [28].The selfreport 11-point scale is widely used in research and clinical practice.Participants were asked to rate their pain level over the previous 24 h on a scale from 0(no pain)to 10(worst pain).The scale has shown good validity for measuring pain intensity [29].
2.4.4.A goniometer
A goniometer is a mechanical device to measure the range of motion (ROM).It is comprised of three parts: a body that is designed as a protractor,a stationary arm,and a moving arm.A normal knee flexion range is 0 (full knee extension) to 140°(full knee flexion).Since difficulty in knee flexion is a common symptom of KOA,the degree of flexion is reported in this study.
2.4.5.The Timed Up and Go Test (TUGT)
The TUGT measures a person’s physical ability.Participants were asked to rise from a chair,walk at a normal pace to a marked line 3 m away,then walk back and sit on the same chair.Higher scores(time taken to complete the test) indicate worse physical ability.The TUGT has excellent test-retest reliability (intraclass coefficient=0.75) in patients with osteoarthritis [30].
2.4.6.Weight scale
A CAMRY BR 9807 personal weight scale(Camry Electronic Ltd.,China) was used to measure body weight in kg.Participants removed their shoes and other objects before standing on the scale.
2.4.7.The Multidimensional Assessment of Fatigue (MAF)
The MAF was used to assess fatigue.The 16-item selfassessment tool contains four dimensions: severity,distress,degree of interference in activities of daily living,and timing.Participants were asked to recall their fatigue experience over the last week;the score is calculated to provide a Global Fatigue Index that ranges from 1 (no fatigue) to 50 (severe fatigue).Reported Cronbach’s α coefficients for the instrument range from 0.81 to 0.96[31].
2.4.8.The Thai geriatric depression scale-15
The depression scale assesses depressive symptoms in older adults.The scale comprises 15 yes-no items and includes positively and negatively worded questions.Total scores can range from 0 to 15,with scores >5 indicating depressive symptoms.The scale’s reported sensitivity,specificity,and internal consistency reliability(Cronbach’s α) are 0.92,0.87,and 0.82,respectively [32].
2.4.9.The Thai Pittsburgh Sleep Quality Index
This questionnaire assesses sleep quality.The seven components contain 19 items.Each component was computed with a total score ranging from 0 (no difficulty) to 3 (severe difficulty).The seven-component score was summed as a global score that can range from 0 to 21,with higher scores indicating worse sleep quality [33].The index has excellent internal consistency (Cronbach’s α=0.83) and test-retest reliability (r=0.89).
2.4.10.The osteoarthritis knee and hip quality of life questionnaire
The questionnaire assesses the QOL in people with KOA.The self-report 43-item scale contains five dimensions (physical activities,pain,mental health,social activities,and social support) and three separate items related to relationship with a partner,sexuality,and employment.The normalized total score ranges from 0 (worst possible QOL) to 100 (best possible QOL).Higher scores reflect greater health-related QOL.The original version of the questionnaire showed satisfactory reliability for each dimension(Cronbach’s α ranges from 0.72 to 0.96).The construct validity(convergent and divergent validity) and reproducibility (intraclass coefficient) were moderate to excellent [34].Applying the committee approach,a professional translator and the principal investigator (fluent in French and Thai) translated the questionnaire from French into Thai independently;then,the expert (a linguist) adjust the disagreement.The reliability was tested by a pilot test in 30 older adults similar to these study participants;the internal consistency (Cronbach’s α) was 0.85.
2.5.Data collection
Outcomes of this study were obtained from self-report and objective measures,medical equipment,and health information questionnaires at baseline,3 months,and 6 months later.The patient outcomes(blood glucose level,ROM,body weight,knee pain,and TUGT) were assessed by trained research assistants (two graduate nursing students)using standard medical equipment.The patient-reported outcomes (fatigue,depressive symptoms,quality of sleep,and QOL) were evaluated by standard measures.Participants who could not complete the 6-month assessment were not included in the final analysis.
2.6.Data analysis
We analyzed descriptive and inferential statistics using SPSS for Windows version 18.0 (SPSS Co.,Ltd.,Bangkok,Mahidol License).During a preliminary examination of all variables,the data-blood glucose levels,pain,and physical ability (TUGT)-were different between groups.Thus,these three variables should be assigned to be covariates based on the standard assumption of multivariate analysis of covariance (MANCOVA) analysis.However,the prior analysis demonstrated non-linearity indicating a low association between these covariate dependent variables,which was a violation for further analysis with MANCOVA [35].Therefore,another option for statistical analysis as multivariate analysis of variance(MANOVA) is of concern for precision analysis.
The assumption for MANOVA was validated,and the findings revealed the heterogeneity of covariance matrices between groups and dependent variables (Box’s M Test=266.938,F=2.424,P <0.001).However,if differences in variances of the dependent variables in each group were lesser than ten times,they were considered normality.Accordingly,the MANOVA analysis was the choice to investigate the effect of the intervention and the interaction effects on patient outcomes across and between the three time periods [35].
2.7.Ethical consideration
This study was approved by the two institutional review boards(IRBs) of the Faculty of Medicine Ramathibodi Hospital,Mahidol University(Protocol#ID 07-59-23)and Nakhon Phanom Province(Protocol # HE600020) before data collection began.The administrative heads of the villages allowed access to conduct research,and the provincial public health office approved engaging the village health volunteers.All participants signed written consents after being informed orally and in writing about the study’s purpose and protocol,the confidentiality of all data collected,and their ability to withdraw without hindering access to health care services.
3.Results
3.1.Characteristics of participants
Of 119 participants who participated in the 3-day comprehensive health education workshop,one dropped out of the intervention group and eight left the control group (total dropout rate:7.56%);no adverse events were found in both groups.Data were analyzed for 110 participants (n=55 in each group).
In both groups,the majority of the participants were female(Table 1).Most participants were between 60 and 74 years old,and 32 participants in each group (58.2%) had chronic illnesses other than T2DM (e.g.,metabolic syndrome).A somewhat greater percentage of participants in the intervention group had pain in both knees.Of all participants’ general characteristics,only the age category showed a statistical difference between intervention and control groups at baseline.
3.2.Effects of the intervention on patient outcomes
Table 2 displays changes in the means of patient outcomes across three time periods.Most patient outcomes in the two groups showed general improvement with statistical significance across time points(P ≤0.001):pain decreased,physical ability improved,less depressive symptoms and fatigue,quality of life and sleep improved.The Bonferroni procedure was performed for multiple comparison tests.The blood glucose level showed a trend to drop and knee ROM showed a trend to increase by the 6-month followup without statistical significance;body weight remained fairly stable.
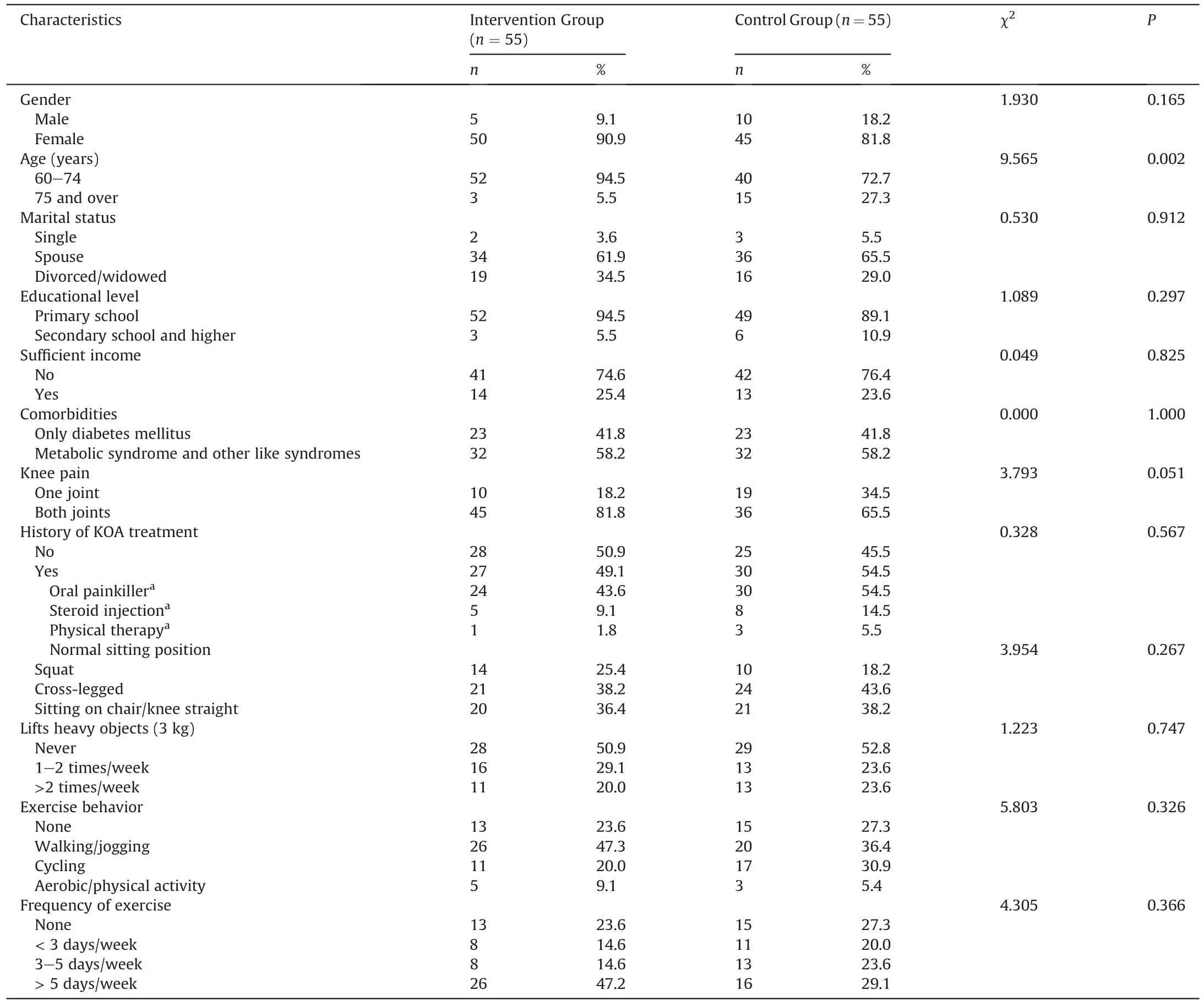
Table 1General and health characteristics of participants.
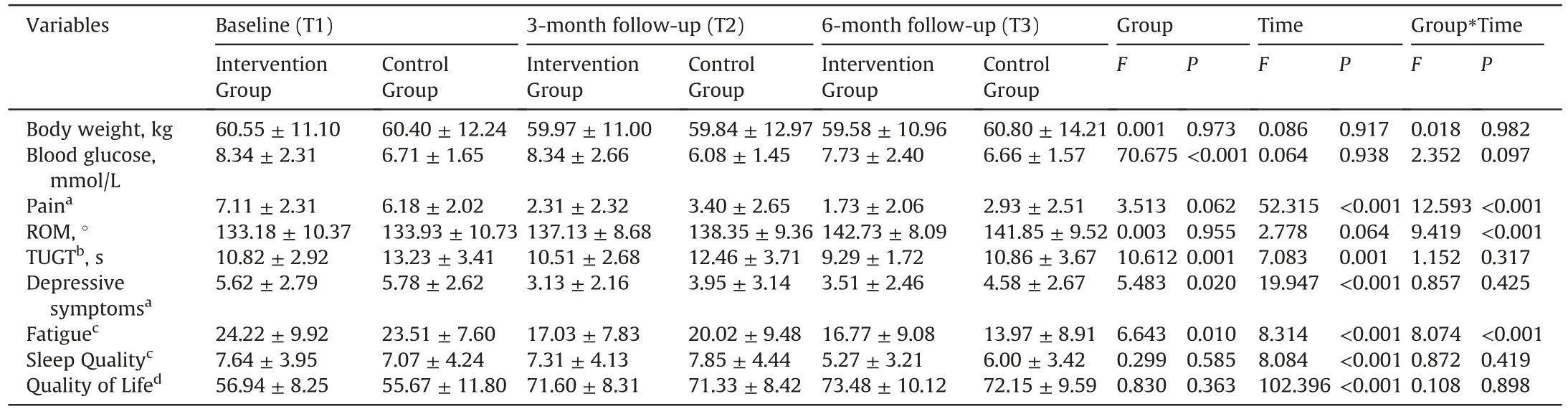
Table 2Means and standard deviations of the study variables across time (n1= n2=55).
The MANOVA analysis showed a statistically significant interaction effect between groups and times indicating that differences existed in the improvement trends of pain,knee ROM and fatigue between the two groups(P <0.001).Differences between the two groups were revealed in blood glucose level,depressive symptoms,fatigue and TUTG with statistical significance (P <0.05).
4.Discussion
This quasi-experimental study evaluated the effects of the comprehensive health education plus village health volunteer monitoring support program on patient outcomes of communitydwelling overweight older adults with KOA and T2DM in Thailand.Participants in the two groups showed general improvement in most patient outcomes,such as pain decreased,physical ability improved,less depressive symptoms and fatigue,and quality of life and sleep improved.These results highlighted the role of nurse-led comprehensive health education for these overweight older adults with KOA and T2DM.The older adults who participated in brisk walking,muscle strengthening exercises,and diet control(comprehensive health education)with social support from village health volunteers lowered their pain levels and enhanced ROM better than those who did not receive support from village health volunteers,and experienced different levels of fatigue across time points of assessments.This is evidence that village health volunteers provide the emotional support and motivation that many older adults find necessary to maintain healthy behaviors.We found that the dropout rate was also lower in the intervention group than in the control group probably because village health volunteers who live in the same community enhance older adults’ self-efficacy to adhere to exercise practices.Utilizing community healthcare providers’ potential may be a significant advantage for countries with limited resources (e.g.health care providers per capita).
Previous research has demonstrated a relationship between depression,pain,and physical ability in patients with osteoarthritis[10,36].It is notable that we found that knee ROM increased and pain decreased for all participants engaged in brisk walking,muscle strengthening,and diet control,independent of the support from the village health volunteers.At each follow-up assessment period,pain and physical ability in both the intervention and control groups showed a trend for improvement.
Pain is a key osteoarthritis symptom that has a negative impact on functional ability and QOL.Previous research has shown an association between pain,depression,and time spent walking in older adults with severe KOA [10,36].Pain is considered to be a mediating factor between depression and physical ability [37].It can lead to poor quality of sleep [9],subsequent fatigue [38],and negative effects on QOL [10,11].Even though pain variation at the base was identified,our results support that exercise programs reduce pain and improve overall physical ability resulting in improved ROM[36,39].
Knee flexion deformity is a common KOA symptom that impacts physical ability [40].Physical and functional limitations have the potential to contribute to other health conditions,particularly fatigue [11].Fatigue in people with KOA is associated with other health conditions,including pain and physical ability [8,11].Consistent with previous studies,we found a reduction in pain scores at each follow-up period with an improvement in physical ability (TUGT decrease).Although we did not investigate causal effects,there is evidence of an association between pain and fatigue[10,11]and between fatigue and physical disability[8,10].However,a note of caution is due because pain does fluctuate,particularly with disease severity.Also,pain perception,nerve function,and central pain processing may be altered due to diabetic conditions,both type 1 diabetes and T2DM [1].Our positive impacts on pain and physical ability,therefore,need to be interpreted with caution.
One issue that emerged from our results is that health beliefs,cultural aspects,and socioeconomic conditions are important factors when initiating tailored interventions to promote health in older adults with multiple chronic illnesses,particularly those who live in rural areas.For example,although the intervention group showed a weight-loss trend,the inability to detect a statistically significant change between groups may have been due to the rural culture in Thailand in which older adults live with extended families and all family members eat the same type of food.When living with extended famliy,it might be difficult to prepare individual meals.Not preparing food themselves,personal or family food preference habits,and health problems can add to older adults being overweight and not adhering to a dietary intervention program [22].We also found that one-third of participants reported insufficient income.Economic problems may limit access to the healthy dietary choices the intervention recommends.
Additionally,some people may believe that lower body weight causes hypoglycemia.Because body mass index influences blood glucose levels,people may wrongly assume that low body weight correlates with dangerously low blood glucose levels.Multiple factors affect the changes in blood glucose levels in older adults with T2DM and multimorbidities [41],including health-related beliefs and practices.Older adults with diabetes might be concerned that hypoglycemia will result when they try to control food consumption to reduce body weight;consequently,body weight remained unchanged.However,the influence of baseline blood glucose variability on outcomes remains unclear.Thus,health beliefs,which consider these variables,are an essential topic for further exploration.
Our results reflect substantial evidence congruent with the recent model of care from the WHO,integrated care for older people (ICOPE),which emphasizes the use of local and family resources integrated together with the implementation of a new way of involving social care workers to promote healthy aging [42].Notably,as mentioned in the social cognitive theory[23],consistent motivation by focusing on individual,environmental,and sociostructural contexts are the keys not only to promoting health,but also to enhancing adherence to healthy behavior changes in the long term.In the present study,the village health volunteers who live in the same socio-cultural contexts may play a pivotal role in understanding personal needs,barriers,and limitations for healthy behavior change.In addition to integrating community resources,the additional roles of village health volunteers-peer support,motivation,reflection,family-collaborating,and monitoring-are momentous in improving adherence to achieve healthy habits in older adults.Undeniably,in chronic illness or long-term care populations,the incorporation of the village health volunteers monitoring support program,or one of similar scope,may be a pragmatic model that reflects the priorities of integrated care for older people that can enhance care and the quality of living in older adults with KOA coexisting with overweight and T2DM,especially in countries with limited resources.
5.Limitations
Although the results are formative,this study has some limitations.The lack of longer follow-up periods(beyond 6 months)may have precluded our detecting significant change in more outcomes.For example,previous research has evaluated body weight more than 12-18 months after participation in an intensive weight loss program[43,44].Also,we did not address other possible adherence barriers to health practices,such as the difference in age(presented in this study) and diagnosed KOA using symptomatic criteria.The discrepancy between blood glucose level,physical ability (TUGT),and pain at baseline prior to intervention is another source of uncertainty;these data should be interpreted with caution.Moreover,participants were from only two sub-districts in one province in Thailand and with mild age bias.The participants from two subdistricts might have different attitudes,beliefs,or socioeconomic status that could influence their health practices.These factors might limit the scope of the analysis and the generalizability of the results.
6.Conclusions
The comprehensive health education plus village health volunteers monitoring and support program was beneficial in promoting good patient outcomes in older adults with KOA and T2DM who are overweight.The effect of the intervention program was significant in alleviating pain and fatigue,and improved knee ROM in the older adults,which showed positive changes across three time periods.The intervention that we have presented can be used as a model (that reflects the WHO model-ICOPE) led by professional nurses for disseminating practice guidelines to reduce the severity of osteoarthritis and enhance health outcomes.Importantly,integrating health education and local/community resources with longitudinal follow-up health outcomes is needed to support adherence to programs for sustainable health behavior change,resulting in more positive patient outcomes in older adults with KOA and T2DM who are overweight.However,questions on physical ability,fatigue,and symptom exacerbation through the trajectory of KOA and T2DM and long-term impact require further research.
CRediT authorship contribution statement
Suparb Aree-Ue:Conceptualization,Methodology,Data curation,Writing -original draft,Writing -review &editing.Inthira Roopsawang:Methodology,Software,Data curation,Validation,Visualization,Writing-original draft,Writing-review&editing.Yuwadee Saraboon:Methodology,Software,Data curation,Validation,Writing -original draft,Investigation.Phichpraorn Youngcharoen:Methodology,Data curation,Investigation.Basia Belza:Conceptualization,Writing-review&editing,Supervision.Viroj Kawinwonggowit:Supervision.
Funding
This study was funded by the National Research Council of Thailand (NRCT/2019).
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of competing interest
The authors have declared no conflict of interest.
Acknowledgments
Special thank you to Asst.Prof.Dr.Pawin Numthavaj,M.D.,Ph.D.and his team-Department of Clinical Epidemiology and Biostatistics,Faculty of Medicine Ramathibodi Hospital;Assoc.Prof.Dr.Jutatip Sillabutra and her team,Department of Biostatistics,Faculty of Public Health,Mahidol University-for professional consultation and additional data analysis.Our thanks also go to all the older participants and village health volunteers in this study.
Appendices.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2022.08.002.
杂志排行
International Journal of Nursing Sciences的其它文章
- Effects of equine-assisted interventions on older adults’ health: A systematic review
- Quality indicators for the care of older adults with disabilities in longterm care facilities based on Maslow’s hierarchy of needs
- Exploring social movement concepts and actions in a knowledge uptake and sustainability context: A concept analysis
- Palliative care needs and symptom burden in younger and older patients with end-stage renal disease undergoing maintenance hemodialysis: A cross-sectional study
- Lived experiences with unmet supportive care needs in pediatric cancer: Perspective of Chinese children and their parents
- Development and validation of a nomogram for predicting the risk of pressure injury in adult patients undergoing abdominal surgery
