Qualitative analysis of compassion fatigue and coping strategies among nurses
2022-11-05NatliaOndrejkovliaHalamov
Natália Ondrejková,Júlia Halamová
Institute of Applied Psychology,Faculty of Social and Economic Sciences,Comenius University in Bratislava,Mlynskˊe Luhy 4,821 05,Bratislava,Slovakia
Keywords:Compassion fatigue Coping Self-care Nurses Qualitative research Psychological adaptation
ABSTRACT Objectives: Nurses are considered to be at risk of experiencing compassion fatigue,which can affect their personal and professional lives.The aim of this study was to investigate stressful factors contributing to the development of compassion fatigue in nurses,their experiences of compassion fatigue,and the coping strategies they used to cope with compassion fatigue.Methods:The convenience sample of 86 nurses from Central Europe was recruited via social networking sites during the pandemic of COVID-19.Data collection was conducted via an online battery of questionnaires which included open-ended questions on the stressful factors,experiences,and coping strategies for compassion fatigue.The data were analysed using a theoretical thematic analysis based on Figley’s descriptions of compassion fatigue.The initial datawas read several times to identify recurring statements.Each statement was then categorized into the emerging domains,subdomains,categories,and subcategories.Results:The results of our study show that stressful factors,experiences,and coping strategies for compassion fatigue in nurses in Central Europe could be related to cognitive,emotional,behavioural,somatic,personal relations,spiritual,and work-related symptoms of compassion fatigue as identified by Figley and that these may resemble experiences of nurses in North America,Japan,and Spain.Conclusion:This study provides a detailed overview of the stressful factors,experiences,and coping strategies for compassion fatigue,which could be used to develop an early screening tool and interventions for alleviating compassion fatigue and for preventive adaptation of the health care system.
What is known?
· Nurses are at risk of experiencing compassion fatigue.
· Compassion fatigue refers to a set of recognizable negative psychological symptoms experienced by helping professionals.
· The triggers of compassion fatigue,experiences of compassion fatigue and coping strategies can be of both personal and workrelated nature.
What is new?
· This study provides a detailed overview of the overall compassion fatigue experience in nurses on all three levels -stressful factors contributing to compassion fatigue,experiences of compassion fatigue and coping strategies.
· This study suggests that the stressful factors,experiences and coping strategies of nurses can all be related to the seven domains as stated by Figley: cognitive,emotional,behavioural,personal relations,somatic and work performance.
· Results of this study suggest that the overall compassion fatigue experience is in fact a multi-dimensional construct and that it may be a cross-cultural phenomenon.
· Based on the results,we recommend developing an early screening tool for nurses as well as utilizing these findings for the development of interventions ameliorating compassion fatigue.
1.Introduction
The concept of compassion fatigue has gained considerable attention in the last couple of decades [e.g.,1,2,3].It was first mentioned in relation to health care professionals as a unique form of burnout experienced by helping and caring professions [4].Compassion fatigue can be defined as a state of tension and preoccupation with traumatized patients through re-experiencing traumatic events,resulting in a desire to avoid patients and reminders of their trauma,and a reduced capacity or interest in bearing the suffering of others[5].It can also be conceptualized as a combination of burnout,associated with a feeling of hopelessness and having to deal with work,and secondary traumatic stress linked to work-related secondary exposure to traumatic and stressful events [6].The main difference between burnout and secondary traumatic stress is the cause -whereas secondary traumatic stress is the result of repeated exposure to suffering,burnout is the result of long-term exposure to various workplace stressors[7].
According to Figley [8],compassion fatigue symptoms can manifest in and affect seven domains: cognitive (e.g.decreased concentration,disorientation,apathy),emotional (e.g.powerlessness,anxiety,numbness),behavioural(e.g.irritability,withdrawal,hypervigilance),spiritual (e.g.loss of purpose,questioning prior beliefs,lack of self-satisfaction),personal relations (e.g.decreased interest in intimacy,isolation from others,increase in interpersonal conflicts),somatic (e.g.sweating,rapid heartbeat,dizziness) and lastly work performance (e.g.lowered motivation,absenteeism,exhaustion).
Helping professionals and health care workers,who are repeatedly required to provide a high degree of care to clients,often experience compassion fatigue [9].Although some helping professionals experience compassion fatigue,many do not and continue to be committed to and effective in their work.These professionals may be motivated by a sense of satisfaction from helping others,labelled as compassion satisfaction [6].
In the field of compassion fatigue research,much of the focus is on nurses.Nurses are considered to be at high risk of experiencing compassion fatigue as they are frequently exposed to patients’traumatic experiences [e.g.10].Several studies have investigated nurses’ experiences of compassion fatigue and we will summarize the results of these.
The first study,by Maytum,Heiman,and Garwick[11],identified work-related triggers of compassion fatigue(e.g.caring for children with chronic conditions and their families,professional roles,work overload,and broader system issues) and personal triggers of compassion fatigue (e.g.being excessively involved or crossing professional boundaries,having unrealistic expectations of oneself,outside commitments,and family problems).Participants also reported having a broad range of physical and emotional symptoms of compassion fatigue.Maytum et al.[11] identified some coping strategies of both a personal (e.g.taking care of oneself through exercise,meditation,focusing on non-work relationships or developing a personal philosophy and faith) and a work-related nature (e.g.debriefing,developing supportive professional relationships).Nurses also emphasized that they found it very important to learn their own triggers and coping mechanisms to prevent the onset of compassion fatigue,and taking care of oneself and having a good work-life balance were described as essential in managing it.
Austin et al.[12] conducted a study of experiences of compassion fatigue,involving nurses who self-identified as experiencing compassion fatigue.Nurses in this study described changing the way they worked,shielding themselves,and distancing themselves from the suffering of patients and families.They also described feeling as if they were running on empty and impotent as nurses,as well as feeling irritable,angry,and hopeless.Another aspect was work difficulties that had carried over into their personal lives,affecting their relationships with family and friends.
A study by Perry et al.[13] described five themes relating to compassion fatigue: defining compassion fatigue,causes,factors that worsen compassion fatigue,factors that lessen compassion fatigue,and outcomes.Participants provided examples of compassion fatigue,but reported having limited knowledge about compassion fatigue.Causes of compassion fatigue included lack of support,lack of knowledge,and lack of time or ability to give high quality care.The difference between the quality of care nurses wanted to provide and what they were actually able to provide and other physical and emotional stresses were identified as worsening compassion fatigue.Factors that lessened compassion fatigue included colleague support,work-life balance,connecting with others,acknowledgement,and maturity and experience.The outcomes of compassion fatigue were profound fatigue of the mind and body,negative effects on personal relationships,and considering leaving the profession.
Ward-Griffin,St-Amant,and Brown [14] examined compassion fatigue among double-duty nurses who provided care both at work and at home.The authors identified the theme of living on the edge and subthemes such as blurred boundaries,preoccupation,lack of resources,feelings of anger,helplessness,exhaustion,guilt,physical consequences,and the need for greater support from colleagues.
Melvin [15]identified three themes:risk of compassion fatigue due to repeated exposure to deaths,the physical and emotional cost of providing care and setting boundaries,and healthy coping strategies (e.g.physical activity outside work,setting boundaries,debriefing with colleagues).Similarly,Drury et al.[16],focused on exploring factors that have an impact on compassion satisfaction.Their results showed that nurses’capacity to cope can be enhanced by strong social and collegial support,infrastructure that supports the quality of nursing care,and positive affirmation.In addition,Mason et al.[17] asked nurses for sources of moral distress and strategies for coping with stress.The identified themes included role conflict with management,death and suffering,dealing with violence,dealing with family,powerlessness,physical distress,and medical versus nursing values.Sheppard [18] described four themes relating to nurses’compassion fatigue:life is unfair,endless suffering,unable to let it go,and wanting support but pushing it away.Nurses experienced symptoms consistent with burnout and secondary traumatic stress,which reduced their compassion satisfaction.In their study,Giarelli et al.[19] identified nurses’sources of stress as communication breakdown,structure of the work environment,care-driven factors,and feelings of self-doubt.The nurses’ recommendations for minimizing work-related stress and compassion fatigue included personal strategies and institutional change.
Lastly,Nolte et al.[3] conducted a meta-synthesis of nine previous qualitative studies of experiences of compassion fatigue.They identified four main themes related to compassion fatigue:physical symptoms (feelings of being worn out,complaints of fatigue/exhaustion along with aches and pains),emotional symptoms(hopelessness,frustration,despair,incompetence,and isolation),trigger factors (workplace stressors,poor coping skills,sense that no one protects or cares for nurses,and difficulties achieving a work-life balance) and remedies to overcome or prevent compassion fatigue (support at work,mentoring,leadership,self-care).
There are other studies about nurses’compassion fatigue which were not included in the meta-analysis [3].Namely,Yoder [20]described the trigger factors of compassion fatigue among nurses:caring for dying patients,or patients with extensive burns and those victimized by a closer other.Other trigger factors were heavy workloads,an unsupportive work environment and failure to achieve personal goals;the authors considered these factors to be associated more with burnout than compassion fatigue.Some coping strategies were described,such as a change in personal engagement,introspection,extra days off,debriefing,change in patients’ assignments,and spiritual activities.
In their study,Berg et al.[21] explored perceptions of stress triggers contributing to compassion fatigue and coping strategies.The analysis revealed certain highly stressful events -children,abuse,family members,avoidable situations,and situations similar to personal experiences.The coping strategies seemed to differ for respondents;however,two coping strategy themes were identified-group strategies (talking/debriefing in small work groups) and independent strategies (talking with a significant other outside work).Similarly to Fukumori et al.[22] studied triggers of compassion fatigue in nurses and found sense of professional inadequacy,compassion for patients and their families,desire to support patients and their families,ruminating about oneself or one’s family,sense of professional mission,dissatisfaction with medical staff,desire to integrate with colleagues,desire to avoid one’s duties,the conflict between one’s belief and reality,reconsideration of the meaning of life,and lastly a sense of powerlessness over cancer.Similarly,Finley and Sheppard[23]found the following triggering factors of compassion fatigue: over-relating with patients and their families,long patient stays,and high patient mortality.The symptoms experienced included internalizing patients’and families’ emotions,being haunted by specific patient deaths,feelings of emotional depletion,assuming that all patients will end up dying,and physical exhaustion.Recently,Perˊez-García et al.[24]studied the causes and consequences of compassion fatigue from the nurse’s perspective and identified the lacks of time and resources to provide comprehensive nursing care as the main cause.The consequences of compassion fatigue included difficulties in carrying out their work,repercussions on family and private life,anxiety,stress,and desire to quit the profession.
As most of the qualitative research on compassion fatigue among nurses has been conducted in North America[e.g.12,13,21],apart from just one study in Japan [22] and a very recent one in Spain[24],we were interested in whether nurses in Central Europe have similar or different experiences of compassion fatigue,its triggers,and coping strategies.Similar experiences would suggest that compassion fatigue among nurses may be a cross-cultural phenomenon.In addition,none of the previous studies directly tested Figley’s [8] model of compassion fatigue experiences or similar,so that was a further reason for embarking on the present study.Consequently,only one of the previous studies [11] examined the overall experience of compassion fatigue including the triggers,symptoms and coping.By studying the overall experience we may gain greater understanding of what nurses go through in their everyday lives and what they tend to do in order to try to manage it.This knowledge is greatly important for understanding the compassion fatigue experience in order for us to incorporate their inputs into effective intervention programs for reducing compassion fatigue.
Furthermore,as none of the research was conducted in Central Europe,we do not know whether nurses here deal with the same or some other issues in their work,therefore we are not able to come up with intervention programs tailored to their specific needs.Moreover,for example in Slovakia or Czech republic,there is generally a shortage of healthcare workers,including nurses [25],which results in greater workloads and pressure of nurses working in healthcare system.Gurkovˊa et al.[25]reported that intentions to leave the workplace,or to go work abroad,is predicted by the level of satisfaction in the nursing profession,with around 29%of nurses reporting they were considering leaving the profession and 46%of nurses considering to leave the organization,which could be explained by both economic and psycho-social influences.K¨overovˊa and ˇDurbisovˊa [26] reported that nurses in Slovakia are experiencing compassion fatigue on a moderate level,while they considered their profession to be challenging,unappreciated and stressful,along with some positive associations such as their work is fulfilling,meaningful,and beneficial.For these reasons,it is important to pay attention to what nurses have to say about their experiences and challenges in the nursing profession in order to try to support their well-being and professional effectiveness in their day-to-day work lives.
2.Aim of the present study
The aim of this study was to explore experiences of compassion fatigue in nurses in Central Europe using a qualitative approach,which has never been done before.We aimed to explore the overall experience of compassion fatigue in nurses and all three stages -preconditions,experience and coping.We focused on the preconditions i.e.stressful factors contributing to compassion fatigue,nurses’ experiences of compassion fatigue,and the coping strategies nurses use or would like to use to help them cope with compassion fatigue symptoms.A further aim was to test Figley’s[8]model of compassion fatigue experience comprising seven domains: cognitive,emotional,behavioural,spiritual,personal relations,somatic,and lastly work performance.We were interested in whether all stages of compassion fatigue experience (stressful factors i.e.preconditions,experiences,coping strategies) correspond to this model of seven domains.Finally,we were interested in comparing the experiences of nurses in Central Europe with those of nurses in North America,Japan,and Spain.
3.Methods
3.1.Qualitative approach
The study follows a phenomenological approach in order to understand and describe the experiences of compassion fatigue by nurses,what they feel like contribute to its development and how they cope with it.A theoretical(deductive)approach was applied to data analysis in order to see whether the overall experience of nurses fit Figley’s model [8] of compassion fatigue.The methodology is encompassed upon an interpretive philosophy paradigm of research which emphasizes the understanding of the individual’s interpretation of the world [27] and believes that its elements are frequently shared among many other individuals or across different cultures.
3.2.Research team
The research team consisted of two members.The first member of the research team was NO-a postgraduate student and assessor who conducted the primary qualitative analysis.The second member of the research team was JH -a university professor and auditor with extensive experience in qualitative research.NO works primarily on quantitative and qualitative research in compassion,self-compassion,and compassion fatigue.JH works primarily on the qualitative and quantitative research of selfcompassion and self-criticism.
3.3.Ethical issues pertaining to human subjects
The data in the study were collected in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments as well as comparable ethical standards (a Faculty of social and economic sciences Comenius University ethical committee 4/2018) and followed Standards for Reporting Qualitative Research (SRQR,www.equator-network.org/reporting-guidelines/srqr).Informed consent was obtained from all participants prior to their inclusion in the study.
3.4.Data collection
Social networking site -Facebook,was used for the questionnaire distribution,targeting health care and nursing groups (e.g.Nurses and health,Nurses and Doctors SK,Nurses advise,Nurses and healthcare assistants,etc.).The questionnaire was distributed by the first author of this study.The data collection was conducted from January to October 2020.At the beginning,all participants provided online informed consent and sociodemographic information.Informed consent included a brief description of the aim of the research,course of the research,confidentiality of information,rights of participants,contact information for the researchers and information that by filling out the questionnaire they agree to participate in the research.They then filled in an online battery of questionnaires,which included the following open-ended questions about their experiences as a helping professional:
(1) What do they and their colleagues consider to be most stressful in their profession?
(2) How does compassion fatigue specifically manifest in their life and how do they experience it?
(3) What coping strategies would alleviate compassion fatigue and what self-care strategies do they find useful and practice themselves in order to manage compassion fatigue?
The third question included seven sub-questions,prompting them to address how they regularly take care of several areas of their life-physical,work,cognitive functions,emotional,personal relations,spiritual and behavioural.All of the questions included in the questionnaire were mandatory-participants needed to fill out their answers in order to move on to another question and finally complete the questionnaire.However,if participants did not want to answer some of the questions,they could have answered just very briefly or typed in any symbol (eg.dash) to move on to the next questions,which was the case in some participants.
A questionnaire with open-ended questions was chosen as a form of data collection for this qualitative research,due to its easy administration,ability to access a larger scale of participants over a relatively short period of time,potential to gain rich and more focused data,as well as some practical advantages for both participants and researchers,such as its accessibility,non-onerosity,being less burdensome for participants,giving them control of key aspects of their participation[28].According to Braun et al.[28],qualitative questionnaires have the ability to produce rich data of the type of sense-making,such as subjective experiences,practices,narratives,etc.Furthermore,Braun and Clarke [29] claim that qualitative questionnaires tend to be filled with more focused and relevant information.
The questionnaire was kept short (10 questions in total) and to the point of research aims,to accommodate the current ongoing pandemic of COVID-19 which severely impacted healthcare workers in Central Europe,resulting in greatly increased work overload and work-related pressure.According to Braun and Clarke[29],good qualitative survey questions should be open,short and expressed as clearly as possible.Such type of data collection was considered more suitable for the current situation,as many nurses might have gone through fatigue (compassion fatigue or general tiredness) and another type of qualitative data collection,such as interviews could be even more exhausting for them due to its timeconsuming nature.
3.5.Research sample
A convenience sample of 86 nurses was recruited via social networking sites targeting health care and nursing professionals in family and friend networks.Participants needed to be actively working as a nurse at any hospital or facility to be included in the study.The research sample consisted of 81 women and 5 men,with a mean age of 40.1 (SD=12.44).All of them were from Central Europe: 68.6% of participants were of Slovak nationality,26.7% of Czech nationality,and 4.7% were of Hungarian nationality.Participants had the following amount of nursing experience: 30.4% had up to 5 years of experience,13.0%had between 6 and 15 years,16.3%had between 16 and 25 years,19.8%had between 26 and 35 years,and others had more than 36 years.Participants reported experiencing compassion fatigue every day(19.4%),a few times per week(14.0%),once a week(3.5%),a few times per month(14.0%),once a month (9.3%),a few times per year (14%),and a few times in their life (22.3%).Lastly,3.5% of nurses had never experienced compassion fatigue.
3.6.Data analyses
We chose the theoretical (deductive) thematic analysis approach[30]to test Figley’s[8]model of compassion fatigue.This type of analysis tends to be driven by the researcher’s theoretical interest in the area[30]and starts with the theoretical propositions derived from the literature review,which are then applied to the data analysis [31].As MacFarlane and O’Reilly-de Brún [32,p.607]said,“… qualitative research designs informed by … theory can be useful to sensitize researchers to concepts and processes that they might not necessarily identify through inductive processes.” In the first step,the assessor studied the initial data several times.Then the recurring statements and emerging themes within the data were identified.In the next step,the statements were coded using pre-existing individual codes.Then,we went through the individual codes to identify patterns within them and categorized them into emerging themes -pre-existing domains,subdomains,categories,and subcategories.Afterwards,the auditor checked the first categorization and provided feedback to the assessor.The auditor’s comments were discussed and incorporated into the final version of the categorization.In the subsequent step,we reviewed the categorization several times to make sure it was an accurate representation of the data.
4.Results
4.1.Stressful factors contributing to compassion fatigue
Statements on the stressful factors in the data were divided into seven main domains -1) Emotional,2) Behavioural,3) Personal Relations,4) Somatic,5) Spiritual,6) Cognitive,and 7) Work Performance.
The first stressful factors domain -Emotional stressors -included all the statements relating to emotions,images of emotions,and emotional difficulties.We identified four subdomains:1)Helplessness,2) Tension,3) Anger,and 4) Confusion.Nurses described feelings of helplessness (“Helplessness.”),tension(“Stress.”),anger (“Impatience and aggression.”),and confusion(“Confused patients.”).
The behavioural domain included all statements relating to actions.We identified one subdomain -Dealing with the Diagnosis.Nurses mentioned having to deal with various diagnoses which they found stressful.They also talked about having to handle acute and emergent cases that changed from minute to minute (“Acute cases in Emergency Room.”) and child patients with difficult diagnoses (“Resuscitating a child.”).
Another domain was Personal Relations.This domain included all statements regarding contact with other people.We identified two subdomains:1)Dealing with People and 2)Negative Feedback.The Dealing with People subdomain was further divided into categories-work team,patients,and patient’s family(listed in Fig.1).Nurses mentioned multiple problems with their work team.First,relationships with colleagues were poor(“Interpersonal conflicts.”);second,they were under pressure not to care too much about patients (“A more empathetic person is a ‘black sheep looking for problems’.”),and lastly,they had to deal with difficult colleagues(“Sociopathic colleagues.”).Nurses found it stressful having to deal with patients and their attitudes (“Sometimes the patient’s attitude towards me.”) and the patient’s family (“Aggravated situations with the family.”).Lastly,nurses described receiving negative feedback from people as stressful(“Negative feedback.”).
The Somatic domain included all statements regarding physical sensations.We identified two subdomains: 1) Physical Difficulties and 2) Exhaustion.Nurses mentioned various physical difficulties(“Heavy physical loads.”) and feeling exhausted (“Lack of rest.”).
The Spiritual domain includes all statements regarding spiritual thoughts and values.This domain can be divided into three subdomains:1)Dealing with Death,2)Difficulty Maintaining a Worklife Balance and 3) Not Having Enough Time for Family.Nurses described having to deal with the deaths of patients in their work(“Death of a patient.”),finding it difficult to maintain a work-life balance (“Combining work and personal life.”) and not having time for their family or close ones (“… even less time for the family.”).
The Cognitive domain includes all statements related to cognitive functioning.We identified two subdomains: 1) Handling Responsibility and 2)Dealing with Situations Out of my Control.These could be further divided into several categories(see Fig.2).Nurses mentioned the stress of being responsible for saving patient lives(“Saving lives.”),patients’ health (“Huge responsibility for patients’health.”)and responsibility for not harming patients(“I worry that I will make a mistake at work and harm the patient.”).Furthermore,they mentioned having difficulty coping with various situations out of their control.These included not being able to help(“Inability to help.”),being unable to solve the problem (“Not knowing about the problem.”),coping with unsuccessful outcomes (“Even though I try,it doesn’t end well.”)or unpredictability(“Unpredictable situations.”).
Lastly,the Work Performance domain included all statements regarding work-related difficulties.There were seven subdomains:1) Workload,2) Shortage of Resources,3) Management,4) Health Care System,5)Health Care Workers not Appreciated,6)Travelling for Work,and 7) Demanding Working Hours.In the Workload subdomain,nurses talked about having a large number of patients(“Many patients.”) and having to work under time pressure(“Working without a break.”).The nurses also found the sheer number of administrative tasks stressful (“The amount of admin.”).Secondly,nurses mentioned there was a shortage of resources,both in terms of staff (“Lack of staff.”) and material resources in the workplace (“Lack of material resources.”).They also talked of management problems: being pressurized by management (“Constant pressure from management.”),bad leadership (“Incompetent leadership.”)and a lack of employer support(“Little support/supervision.”).Problems were also identified with the health care system.Nurses described the health care system as being outdated (“Old health care system.”),having pointless rules (“Meaningless regulations.”),requiring high education levels (“High educational requirements.”)and being bureaucratic (“Bureaucracy.”).Furthermore,nurses talked about health care workers being unappreciated,undervalued (“Underestimated by the employer.”) and insufficiently remunerated(“Financial evaluation.”).They also mentioned having to travel for work(“It is stressful having to travel abroad for work.”)and,lastly,demanding working hours (“Difficult working hours.”).
4.2.Experiences of compassion fatigue
The statements regarding experiences of compassion fatigue were categorized into seven main domains according to Figley’s model [8]: 1) Emotional,2) Behavioural,3) Personal Relations,4)Somatic,5) Spiritual,6) Cognitive,and 7) Work Performance.
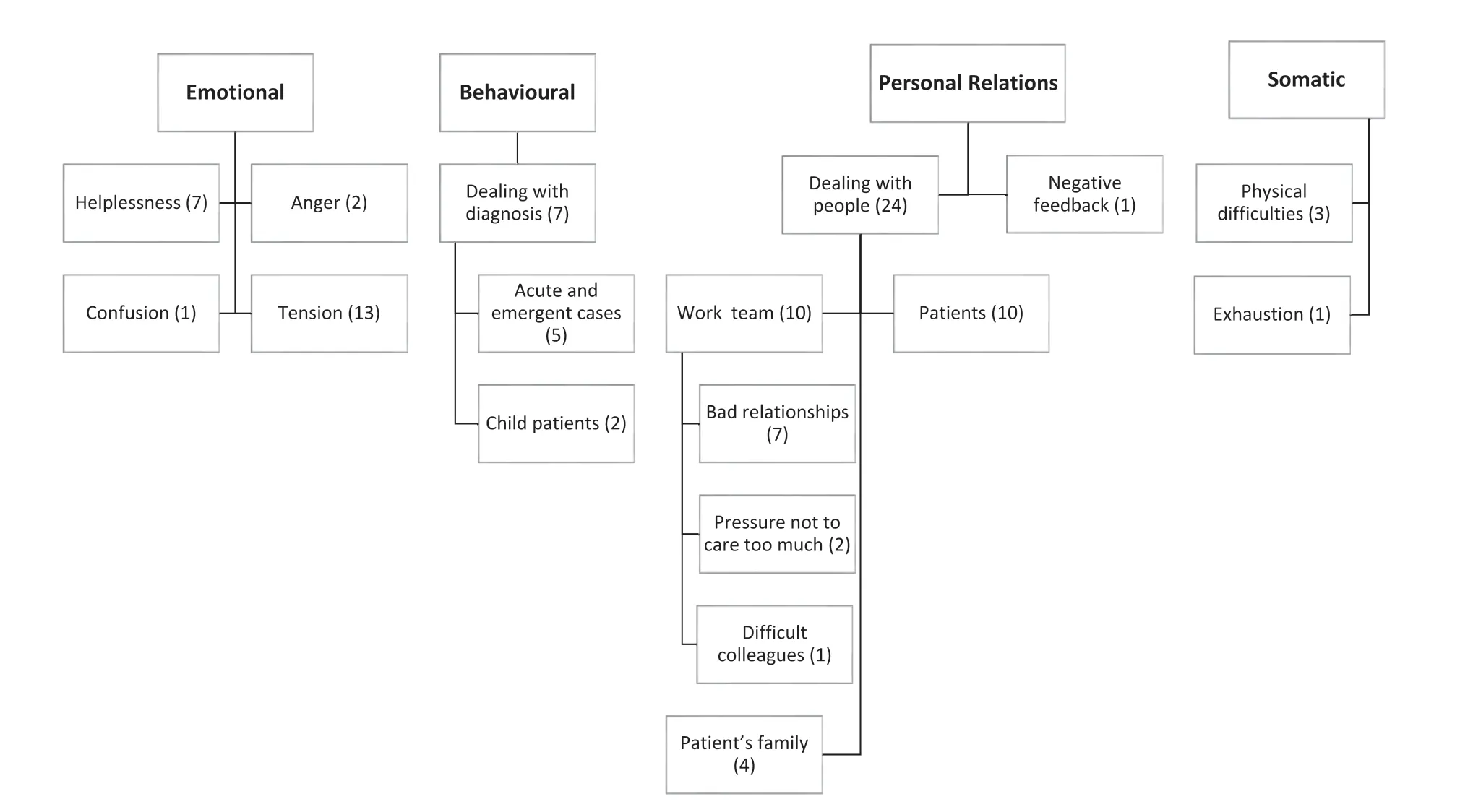
Fig.1.Domains,subdomains,categories,and subcategories of Emotional,Behavioural,Personal Relations,and Somatic stressful factors,with the number of occurrence.
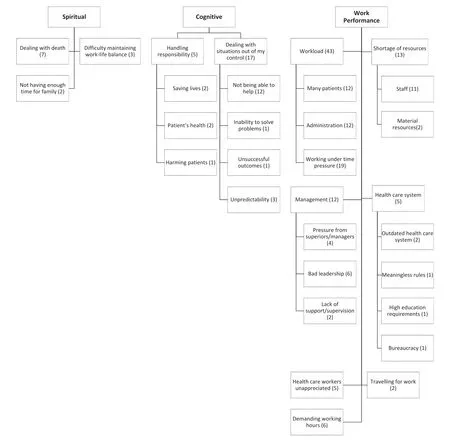
Fig.2.Domains,subdomains and categories of Spiritual,Cognitive,and Work Performance stressful factors,with number of occurrences.
The Emotional domain includes all the statements related to emotions and emotions experienced during compassion fatigue.This domain includes 11 subdomains which correspond to the emotions experienced(see Fig.3).Nurses described feeling wound up(“I’m not nice to the patients,I feel wound up…,everyone’s getting on my nerves.”),sad(“When it happens to me[compassion fatigue],I feel sad…”),apathetic(“I’m not in the mood for anything.”),numb(“I do my job without emotion …”) and disappointed (“I feel disappointed …”).Some also felt fear (“I feel … scared.”),hopelessness(“Everything is stupid,there is no progress at all.”),powerlessness(“I feel mentally tired at not being able to help the patient,I don’t have enough time or the capacity to help.”)and helplessness(“The feeling that I can’t do anything more,it’s too much.”).
The Behavioural domain includes all statements regarding actions and behavioural intentions/tendencies related to compassion fatigue.This domain was further divided into three subdomains:1)Unpleasant behaviour,2)Avoidance and 3)Escape from everything,and the seven categories are listed in Fig.3.Nurses mentioned various unpleasant behaviours,such as being more impatient (“I don’t have enough patience.”),irritated (“Everyone around me irritates me.”) and explosive (“I am more explosive.”),aggressive (“…aggression”)and obnoxious(“I am obnoxious…”).Signs of avoidance were also found,either in relation to tasks (“I feel exhausted,irritable,I feel like running away from all my responsibilities.”)or people(“I have no interest in contact with people.”).The last domain is the general desire to escape(“I feel like running away from everything.”).This domain contained all the statements related to the impact of compassion fatigue on nurses’ interpersonal relationships.It includes one subdomain labelled Isolation from Others,in which we identified two underlying categories:1)Not communicating and 2)Preferring solitude(refer to Fig.3).We identified two Isolation from Others categories,concerning communication with others and tendency to isolate oneself.Nurses mentioned not being in the mood to communicate with others(“I feel the need to be silent for at least 2 hours…”) and preferring to be alone (“The need to be alone,having time for psychohygiene.Everyone should leave me alone for at least a day.”).
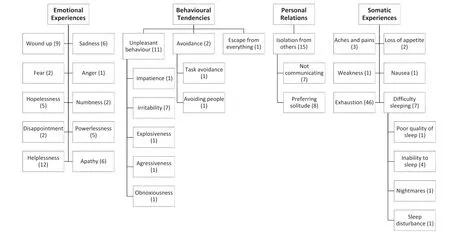
Fig.3.Subdomains and Categories of Emotional Experiences,Behavioural Tendencies,Personal Relations,and Somatic Experiences,with number of occurrences.
The Somatic domain includes all the statements concerning bodily sensations and somatic difficulties.We identified six subdomains: 1) Aches and Pains,2) Loss of Appetite,3) Weakness,4)Nausea,5) Exhaustion,and lastly 6) Difficulty Sleeping.The latter had four different categories,see Fig.3.Nurses described experiencing various aches and pains(“My whole body is in pain,especially my head.”) and loss of appetite (“I don’t usually eat anything at all during this period and I drink a maximum of 1 glass of water a day.”).The most common somatic experience was exhaustion(“I feel like I am drained of energy.”),followed by difficulty sleeping,such as poor quality of sleep (“Poor quality of sleep.”),being unable to sleep (“I can’t sleep,even at night,I sleep only 1 or 2 hours.”),having nightmares (“When I fall asleep,I have nightmares about failing to help someone close to me and usually they die or something bad happens to them.”) or having sleep disturbances (“Waking up at night.”).
The Spiritual domain includes all statements regarding worldview,purpose of life and death,spiritual or religious beliefs and behaviours.We identified three subdomains.1) Questioning the Point,2) Thoughts about Death and 3) Searching for Spiritual Answers(see Fig.4).Nurses mentioned having doubts about the point of their work(“Anyway,I just wonder if it all makes any sense,what would happen if I went and did something else.But in the morning I wake up and look forward to seeing my colleagues …”),thoughts about deaths they have witnessed (“I think about death.”),and searching for answers (“I need to absorb it all and deal with everything.”).
The Cognitive Experiences domain includes all statements related to cognitive functioning and cognitive changes.This domain was further divided into three subdomains:1) Intrusive Thoughts,2) Overwhelmed by Number of Stimuli,and 3) Not Thinking Properly.The Intrusive Thoughts subdomain was further divided into 10 categories (see Fig.4).Nurses reported having various cognitive experiences,including being overwhelmed by the sheer number of stimuli (“Mentally overwhelmed.”) or not thinking properly (“I can’t concentrate on anything at home,not even on household chores.”),and various intrusive thoughts including questioning the reasons for this state(“Why am I feeling this way?”),analysing failure(“What am I doing wrong?”)and how to improve it(“What can I do differently?”),wondering when this state will end(“When will this end?”),questioning oneself (“Have I forgotten something?”),and thinking about free time (“What TV programme should I watch,what book should I read,where is there nice weather in the mountains… ?”).
The Work Performance domain includes statements regarding the impact on nurses’ work performance or effectiveness.We identified five subdomains: 1) Reluctance to Work,2) Loss of Motivation,3) Less Effective with Patients,4) Doing the Work Mechanically and Unemotionally,and 5) Less Productive Outside Work.We also defined some categories (see Fig.4).Nurses mentioned being reluctant to work and longing for retirement(“Only retirement can help me at this point.”).They also described disliking their work (“I dislike my job.”) and preferring to stay at home(“I would like to shut myself up in my room and not go out for a long time.”).Another subdomain mentioned was loss of motivation to work (“My work does not positively motivate me.”),doing their work mechanically,and losing interest in patients (“I do the work mechanically.”),being less productive even outside work (“I lie passively and watch TV or play with my mobile phone.”).The last subdomain we identified was related to working with patients:nurses said they would rather take care of plants (“I would rather take care of flowers than people.”)or coma patients(“…I’m trying to take care of coma patients.”),being detached from patients’ problems (“Avoiding and not admitting problems.”),or even avoiding patients (“I avoid that person.”).
4.3.Coping with compassion fatigue
The statements regarding coping strategies for compassion fatigue were categorized into seven main domains based on Figley’s model of compassion fatigue and the relevant area:1)Emotional,2)Behavioural,3) Personal Relations,4) Somatic,5) Spiritual,6)Cognitive,or 7) Work Performance.These included all statements regarding any coping strategies used or any strategies they would like to use to cope with compassion fatigue.
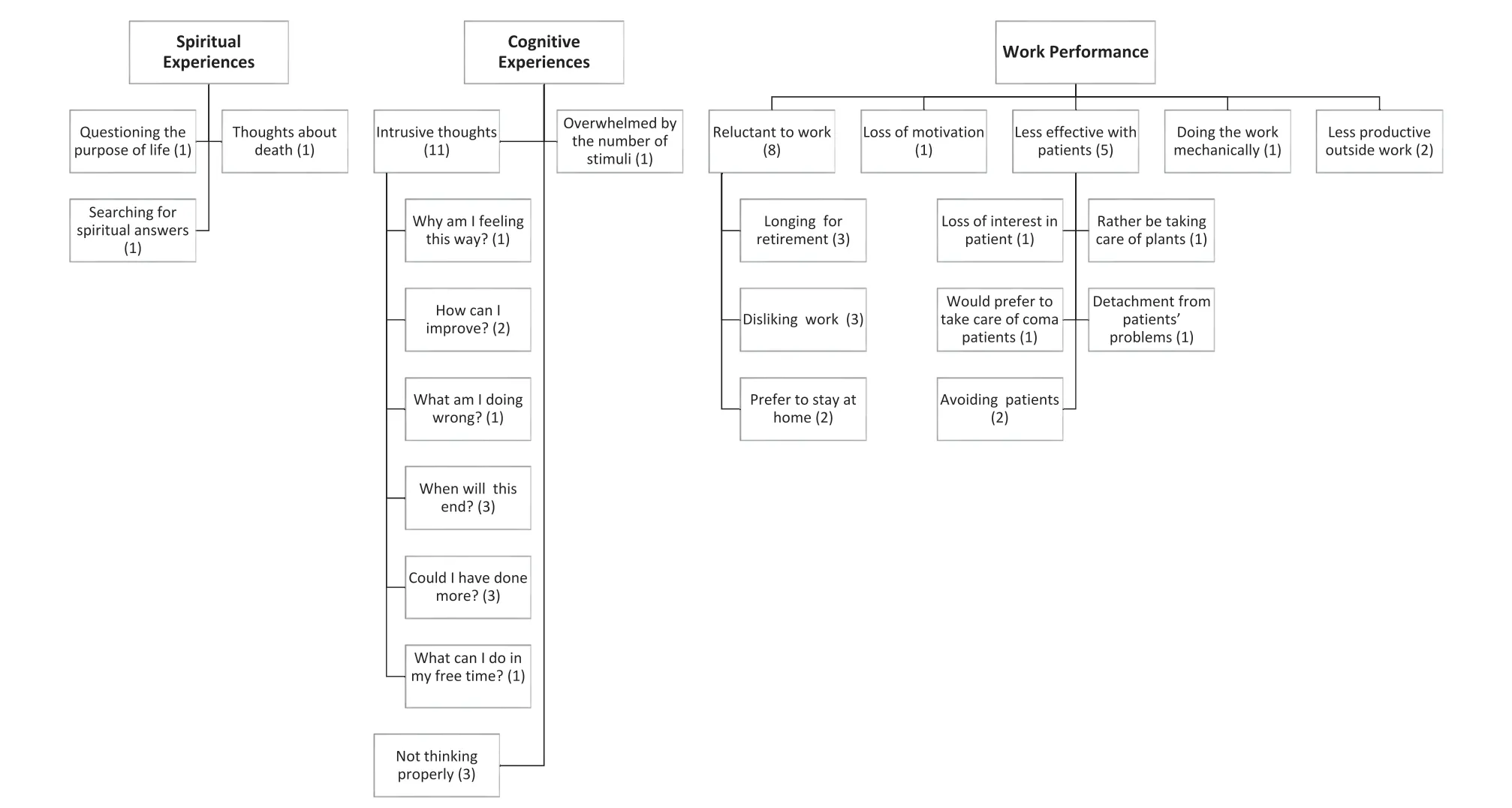
Fig.4.Subdomains and Categories of Spiritual Experiences,Cognitive Experiences,and Work Performance,with number of occurrences.
The emotional coping strategies subdomain includes all the statements related to emotional care or processing emotions.Three subdomains for emotional coping strategies were identified: 1)Affection from Others,2) Processing one’s Emotions and Experiences,and 3)Affection from Pets.Further categories were identified within these subdomains(see Fig.5).Within the data,we identified several emotional coping strategies including affection from others.Nurses mentioned receiving love,smile,and hugs from others,or even gratitude from patients and their families.The presence of a partner or close other was also mentioned.Another coping strategy identified was making an effort to process emotions and experiences,either by going to a psychologist or psychotherapist,keeping a diary and recording their daily experiences and emotions,and trying to regulate their emotions.Lastly,taking care of pets and spending time with them was another coping strategy mentioned.
The Behavioural domain includes statements regarding any actions the nurses took to maintain well-being and deal with compassion fatigue.Four subdomains of behavioural coping strategies were identified: 1) Hobbies,2) Self-growth,3) Going to the Countryside,and 4) Simply Doing Nothing.These were further divided into categories (see Fig.5).The behavioural coping strategies the nurses adopted included finding time to do their hobbies(e.g.creative activities,music,cooking,and baking or playing games),working on their self-growth,either by working on improving themselves,overcoming bad habits,practicing selfcontrol,trying new things or reflecting on their behaviour and thinking.Another coping strategy we identified was going to the countryside.
This domain contained statements related to attending to personal relations: 1) Contact with Others,2) Isolation from Others,and 3) Better Relationships with Colleagues.For the subdomains and categories,see Fig.6.Participants mentioned attending to their relationships via contact with close others (family,children,partners,or friends),usually by doing joint activities(e.g.going on trips,to movies,restaurants)or communicating with them(by phone or face-to-face).They also mentioned isolating themselves from others for a time,while they absorbed and coped with their feelings or bad mood to protect their relationships.
The Somatic domain includes all statements related to body care.This domain was divided into five subdomains:1)Taking Care of the Body,2) Relaxation,3) Exercise,4) Sleep Habits,and 5)Healthy Eating Habits.The categories are listed in Fig.6.Nurses described taking care of their body by having massages or pedicures,going to the hairdressers or cosmetician,or engaging in aromatherapy.They relaxed either by resting or going to a wellness centre or sauna.Another somatic coping strategy we identified was exercise including fitness regimes,yoga,hiking,and swimming.They also maintained regular sleeping and healthy eating habits.
The Spiritual domain contains all statements related to care associated with spiritual and religious beliefs and worldviews.Eight subdomains were identified: 1) Quest for Purpose,2) Working on Future Dream,3) Changing Way of Life,4) Religious Activities,5) Reading Literature,6) Showing Gratitude,and 7)Meditating.The categories are listed in Fig.7.Nurses talked about trying to find meaning in their life and work,working on achieving a dream,making changes to their lives -either by changing their way of thinking or their lifestyle.They mentioned religious activities like praying and attending liturgies,or going to church.They also devoted time to reading spiritual,motivational,or religious literature,showing gratitude and meditating (including mindfulness).
The Cognitive subdomain includes statements regarding work and cognitive functioning.Cognitive Coping Strategies were further divided into five subdomains:1)Expanding Knowledge,2)Reading,3) Logical Thinking,4) Learning to Detach,and 5) Understanding from Others.These could be further divided into categories (see Fig.7).Nurses mentioned various coping strategies relating to cognitive functioning such as expanding their knowledge by learning languages,further education in their field,or learning other new things.Nurses also devoted their free time to reading,either for pleasure and escaping from reality into a fantasy world or others’ stories,or reading for professional development.They also mentioned working on expanding their logical thinking,by doing crosswords,sudoku,or brain teasers.Other coping strategies identified were learning to distance themselves from work or other people’s problems (“Distancing.”),and understanding from others.
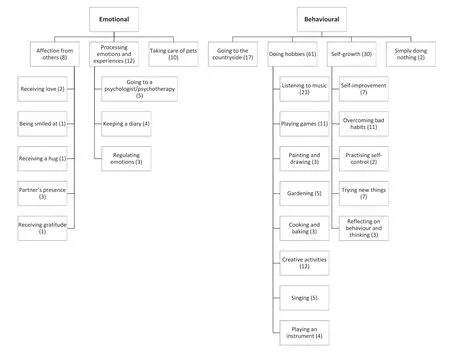
Fig.5.Subdomains and categories of Emotional and Behavioural Coping Strategies,with number of occurrences.
Lastly,work-related coping strategies included all statements regarding coping with work.Seven subdomains were mentioned:1) Better Working Conditions,2) Managing Work,3) Change of Work,4) Break from Work,5) More Feedback,6) Better Work Atmosphere,and 7) Maintaining a work-life balance.These were divided into different categories (see Fig.7).Nurses found improvements in work conditions helpful,such as staff reinforcements,better remuneration,employee benefits,or having fewer work shifts.They also tried to manage their work more effectively through task delegation,task prioritization,and time management.Nurses also thought it helpful to change their work in some way,by taking retirement,finding a different job,or at least changing their working hours or going part-time.Another coping strategy that was identified was taking a break from work by going on holiday,taking longer periods off work,or reducing overtime shifts.Another coping strategy they found helpful was getting more feedback about their work,improving the work atmosphere by working on their relationships with colleagues,or altering the work environment.Lastly,having time to work on their work-life balance was mentioned several times.
5.Discussion
5.1.Stressful factors,experiences,and coping strategies for compassion fatigue in nurses in Central Europe
This qualitative study explored experiences of compassion fatigue in nurses in Central Europe,as well as possible stressful factors contributing to compassion fatigue and coping strategies to see whether compassion fatigue in nurses in this region resembles that described in studies conducted in North America,Japan,and Spain.We also aimed to test Figley’s [8] seven-domain model of compassion fatigue experience.To our knowledge,none of the previous studies of nurses studied experiences of compassion fatigue in such detail and Figley’s [8] model of compassion fatigue had not been tested previously.This study is the first conducted in Central Europe.
Our results show that nurses’experiences of compassion fatigue encompass these seven domains:emotional,behavioural,personal relations,somatic,spiritual,cognitive,and work performance,in all three stages of compassion fatigue -stressful factors,experiences and coping strategies.As our findings on compassion fatigue in nurses in Central Europe are similar to previous findings on compassion fatigue,we presume that compassion fatigue is a crosscultural phenomenon,at least in nurses.
5.1.1.Stressful factors contributing to compassion fatigue
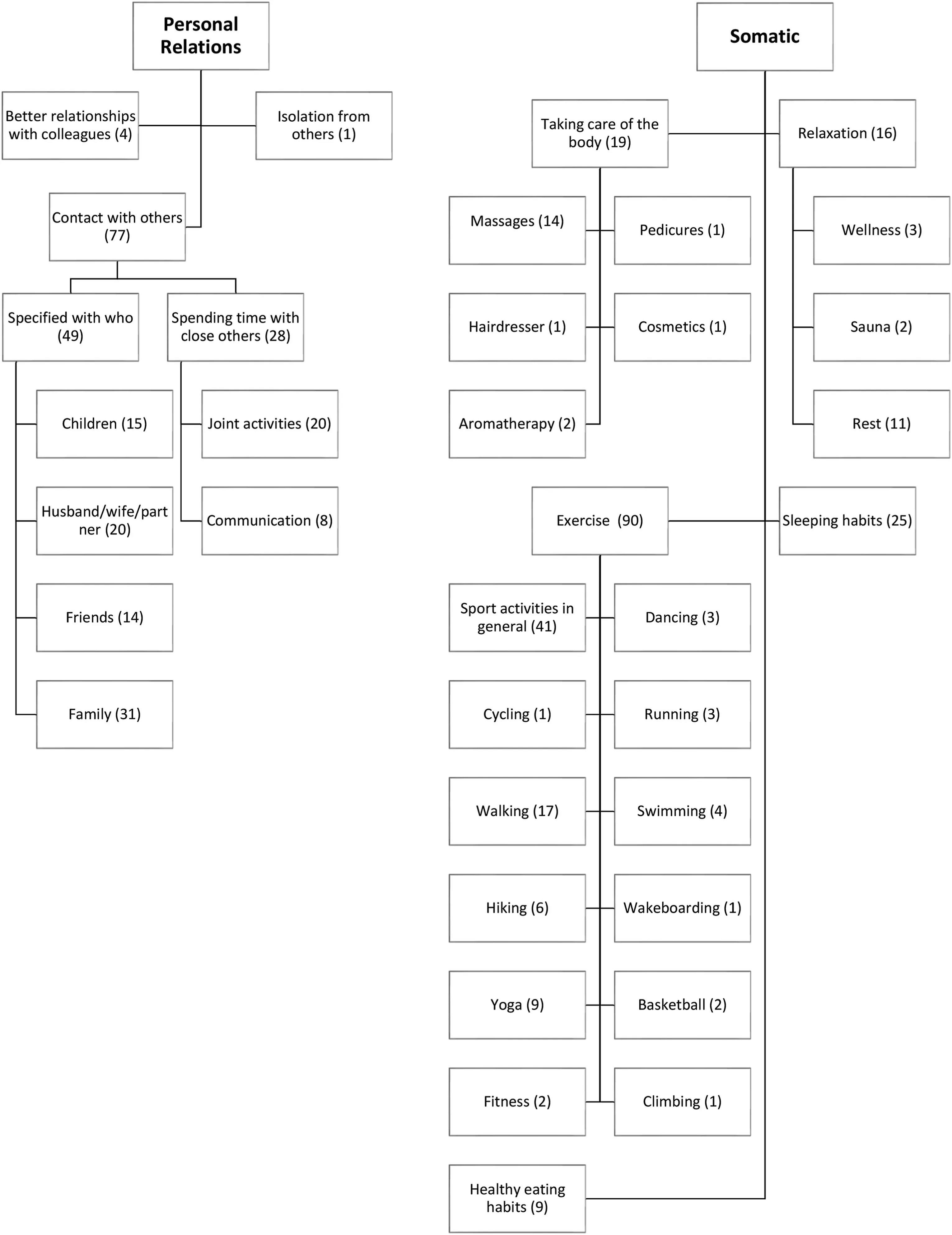
Fig.6.Subdomains and categories of Personal Relations and Somatic coping strategies,with number of occurrences.
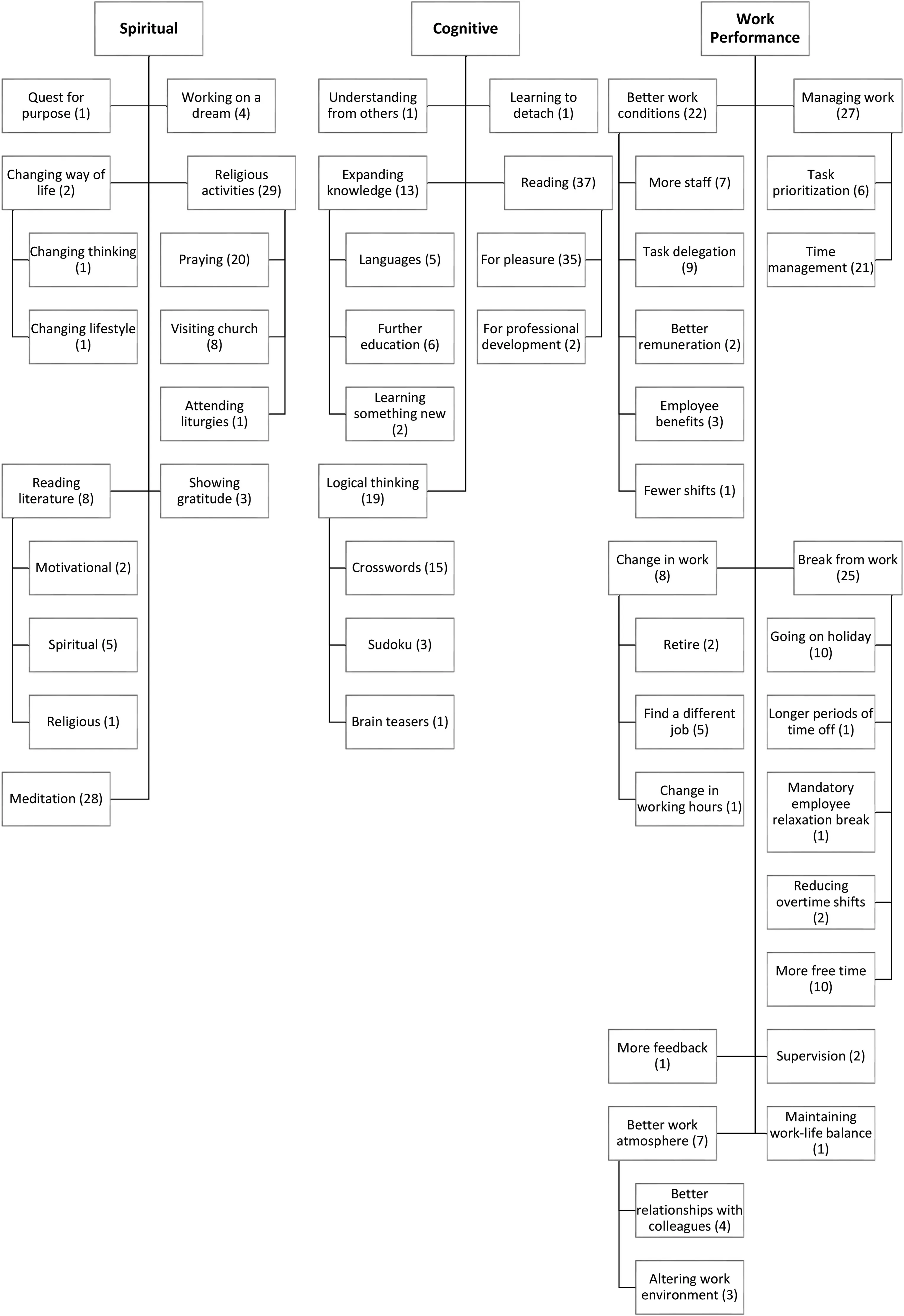
Fig.7.Subdomains,categories,and subcategories of Spiritual,Cognitive,and Work Performance Coping Strategies,with number of occurrences.
We found that the stressful factors contributing to compassion fatigue are experienced on the emotional,behavioural,personal relations,somatic,spiritual,cognitive and work performance levels.The nurses mentioned work-related stressors most,such as workload.Similarly to a study by Perˊez-Garcia et al.[24] and Maytum et al.[11],nurses indicated having heavy workloads (patients and administration) and lacking resources [24],which meant they felt they were working under greater time pressure and could not provide patients with the proper care.The nurses in our study also felt they were under constant pressure from management,and even colleagues,not to provide too much care to the patients,which is something that none of the previous studies reported.Perry et al.[13]did however report that nurses felt a lack of support from management and even a lack of time to provide such quality of care they would like to provide.Nurses in our study described having to deal with various stressors in their work,including having to cope with emotions,situations out of their control,different diagnoses,a high level of responsibility,and different people situations.Contrary to previous findings,having to deal with the family of patients was in our study more related to negative situations with the family or their attitude towards nurses(such as aggravated situations,conflicts or being pressured),than related to over-relating with the family[23]or being burned by the suffering of family[17].Other stressors contributing to compassion fatigue included nurses’ demanding working hours and physical difficulties related to having been on their feet for most of their shifts,poor hospital management,the health care system,and difficulty maintaining a work-life balance.Furthermore,various emotions were identified as stressors such as powerlessness similar to Mason et al.[17] and contrary to previous research feelings of anger,tension or confusion as well.Our findings are similar to previous research in identifying both personal and work related stressors as the causes or triggers of compassion fatigue[11,21,22],however,none of the previous research did report these preconditions to this extend,e.g.Perˊez-García et al.[24]in their study reported only work-related stressors.Some of these preconditions can be thought of as being more closely related to secondary traumatic stress (such as contact with death or dealing with emergent cases and uncontrolled situations),whereas others are more similar to burnout (such as workload or pressure from management);however,it seems that when these are combined compassion fatigue emerges,as described by Stamm [6].The cooccurrence of all these stressors seems to lead to the onset of compassion fatigue in nurses,which has an impact on both their personal and professional lives.
5.1.2.Experiences of compassion fatigue
These stressors feed into experiences of compassion fatigue.Compassion fatigue seemed to be experienced in seven domains,the same domains as in Figley’s [8] description of compassion fatigue.These are emotional,behavioural,personal relations,somatic,spiritual,cognitive and work performance.The findings show that compassion fatigue is in fact a multidimensional construct affecting different areas of a nurse’s personal and professional life.Emotional symptoms are generally present in compassion fatigue,and we did report quite a lot of emotions which accompany compassion fatigue.Similar to Austin et al.[12],we did report emotions like anger and hopelessness,we did however report several more emotions such as disappointment,sadness,being numb or apathic.In contrast,Nolte et al.[3]reported also feelings of despair or incompetence,or Ward-Griffin et al.[14]reported nurses feeling guilty,neither of these were identified in our study.Compassion fatigue in our study was accompanied by several behavioural symptoms,most prevalent of which were unpleasant behaviors.Austin et al.[12] described nurses being irritated,which was present in our study as well.Furthermore,we did report several more unpleasant behaviors such as impatience,or obnoxiousness.Another area of life in which we can observe the impact of compassion is the area of personal relations.We did report in our study negative impact on personal relations of nurses,similarly to findings by Austin et al.[12] and Perry et al.[13],in terms of preferring to be alone or not communicating with others.Furthermore,nearly half of the nurses in the study had experienced somatic experiences,particularly total exhaustion.This is similar to findings described by Finley and Sheppard [23],as well as Nolte et al.[3]and Perry et al.[13].In our study,we managed to identify some other somatic experiences such as nausea,loss of appetite,aches and pains,or sleep difficulties.Spiritual experiences were not in large presented by previous studies,with the exception of Finley and Sheppard[23]who reported nurses assuming that all patients will end up dying,which could correspond to spiritual changes or some kind of loss of belief in good outcomes and Fukumori et al.[22],in which compassion fatigue was accompanied by reconsideration of the meaning of life.We did,however,report some spiritual experiences such as questioning the purpose,thoughts of death or searching for spiritual answers,although it was not that prevalent in the data.Similarly,cognitive experiences were not that prevalent in previous studies as well.We did report a number of different intrusive thoughts or cognitive difficulties such as not being able to think properly.Finley and Sheppard[23]did however report nurses feeling like they are being haunted by specific patient deaths,which relates to the cognitive and intrusive imagery.In contrast,the intrusive thoughts in our study were more related to thoughts about why is it happening to them and re-thinking the situation(e.g.,what else I could have done)than being related to a specific occurrence of one patient.Lastly,quite prevalent in work performance experiences in our study was the reluctance to work and being less effective with patients.Perry et al.[13] did report nurses having considered leaving the profession,but other studies did not report such occurrences,along with any of them not reporting the ineffectiveness with patients,which included in our study loss of interest,avoidance,detachment,etc.We did not report inclination to leave the profession,like Perry et al.[13],we did however report nurses being reluctant to work,similar to Fukumori et al.[22],and longing for retirement,disliking their job or preference to stay at home.Some of the nurses (n=3) in our study stated that they had no symptoms at all or had even experienced the opposite of compassion fatigue -compassion satisfaction,as described by Stamm [6].
5.1.3.Coping strategies with compassion fatigue
Lastly,some strategies were identified for coping with compassion fatigue.These included attending to one’s cognitive and emotional functioning,bodily care,spiritual care,relations with close others,working on behaviour,or work related coping strategies.Therefore,they were described on the same seven domains as were stressful factors and experiences of compassion fatigue.Similar to Berg et al.[21],our participants responses seemed to differ from participant to participant,which resulted in quite a lot of generated categories.As we managed to recruit a larger number of participants than we would in other types of qualitative research design e.g.,in-depth interviews,our data are more detailed and they describe more types of categories (activities) in each domain,compared to those from previous studies.Some findings are however in line with results from previous researches.For example,Nolte et al.[3] mentioned that one remedy for overcoming or preventing compassion fatigue was the provision of greater support at work,leadership,and self-care strategies.And a study by Maytum [11] identified both personal and work-related strategies.In our study,attending to relationships outside work was another coping strategy.Berg et al.[21] obtained a similar finding:talking with a significant other outside work was helpful in overcoming compassion fatigue.Furthermore,Yoder[20]described some spiritual activities as well.
5.1.4.Summary
The prevalence of compassion fatigue is much higher in our study (96.5%) than in any of the other studies (7.3% and 40%,see Ref.[33]) which might be due to participants’ characteristics and the poor state of the health care system,the low wages,and very low status of nurses in the health care hierarchy,compared to doctors for example.The COVID-19 pandemic could be another cause,as it was ongoing during the data gathering and severely tested health care systems in Central Europe and around the globe.
Our findings summarize the overall experience of compassion fatigue,stressful factors which could possibly lead to compassion fatigue,and coping strategies adopted or considered helpful in overcoming it.As most of the previous research we have accessed was conducted in the United States,Canada,and Japan,and one very recent study in Spain,our results from Central Europe support that compassion fatigue be a cross-cultural phenomenon;further research is needed.
5.2.Limitations
The main limitation of our study is the form of data collection.This written form of data collection was useful in obtaining a sufficient amount of key information over a short period of time and avoided a long rewriting process.However,the data were less detailed,more limited,and more succinct.Interviews,for example,could have provided more in-depth,illustrative data.Another limitation may be the presence of a sampling bias.This limitation is generally present in questionnaire design,as there is the risk of excluding participants for example with limited literacy skills or those participants who are not that privileged in this digital age[28],or those participants who choose not to spend time online,on social networking sites,or do not participate in online groups,discussions,etc.
5.3.Implications
Our findings improve understanding of nurses’ experiences of compassion fatigue.They could be used to develop interventions to alleviate compassion fatigue and to preventively adjust health care systems.In addition,our results summarize a variety of coping strategies nurses use to overcome compassion fatigue,which could be used to draw up best practice guidelines for nurses to help them cope with compassion fatigue or prevent it from arising in the first place.The overview of the possible stressors and preconditions could be used in the future to detect early signs of compassion fatigue to prevent it from becoming more serious and aid a rapid recovery.Findings could also be incorporated into intervention programs to ameliorate compassion fatigue.The intervention targets multiple areas,such as self-criticism,self-care,mission,worklife balance and skills necessary for helping professionals to better prevent,deal and overcome compassion fatigue.
In addition,we suggest that further analysis be conducted on nurses’ experiences of compassion fatigue and their coping strategies,so nurses who have never experienced compassion fatigue have a deeper understanding of it and are better able to avoid or prevent compassion fatigue developing,and aimed at creating a set of nurses’ best practices to prevent compassion fatigue.Further research could focus on analysing the relationship between the different self-care strategies and compassion fatigue,and examine which self-care strategies seem to be most effective in countering compassion fatigue and fostering compassion satisfaction.In addition,as most of the research is focused on nurses,further research should focus on exploring experiences of compassion fatigue among different helping professions,such as social workers,psychologists,teachers,and police officers,and the problems they face in overcoming compassion fatigue.That would answer the question of whether there is a general form of compassion fatigue experienced similarly by all helping professions or whether it is a profession-specific phenomenon.
6.Conclusion
This study provides a detailed overview of the stressful factors,experiences,and coping strategies of compassion fatigue among nurses in Central Europe.The results of our study indicate that compassion fatigue among nurses in Central Europe is accompanied by cognitive,emotional,behavioural,and somatic changes,as well as changes in personal relations and work performance,as described by Figley [8].Additionally,the experiences of nurses in Central Europe resemble the experiences of nurses in North America,Japan,and Spain,which might suggest that compassion fatigue is a cross-cultural phenomenon.Our findings provide information for gaining a greater understanding of nurses’ experiences of compassion fatigue.These findings could be further used in developing interventions for alleviating compassion fatigue and creating better health care systems to prevent it.
CRediT authorship contribution statement
Natˊalia Ondrejkovˊa: Conceptualization,Methodology,Data curation,Formal analysis,Writing -original draft,Writing -review &editing.Júlia Halamovˊa: Conceptualization,Methodology,Formal analysis,Writing -original draft,Writing -review &editing.
Funding
Writing this work was supported by the Vedeckˊa grantovˊa agentúra VEGA under Grant 1/0075/19.
Data availability statement
In order to comply with the ethics approvals of the study protocols,data cannot be made accessible through a public repository.However,data are available upon request for researchers who consent to adhering to the ethical regulations for confidential data.
Declaration of competing interest
The authors declared no potential conflicts of interest with respect to the research,authorship,and/or publication of this article.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2022.09.007.
杂志排行
International Journal of Nursing Sciences的其它文章
- Effects of equine-assisted interventions on older adults’ health: A systematic review
- Quality indicators for the care of older adults with disabilities in longterm care facilities based on Maslow’s hierarchy of needs
- Exploring social movement concepts and actions in a knowledge uptake and sustainability context: A concept analysis
- Palliative care needs and symptom burden in younger and older patients with end-stage renal disease undergoing maintenance hemodialysis: A cross-sectional study
- Lived experiences with unmet supportive care needs in pediatric cancer: Perspective of Chinese children and their parents
- Development and validation of a nomogram for predicting the risk of pressure injury in adult patients undergoing abdominal surgery
