Multicenter application of a nursing workload measurement scale in adult hospitalization units
2022-11-05MrFuensntHellGilMrzenMiklAnMyrimSevLlorMrDoloresRoldVlcrcelFrnciscoJvierIbezpezMrJospezMontesinos
Mrí Fuensnt Hellín Gil ,Mrzen Mikl ,An Myrim Sev Llor ,Mrí Dolores Roldán Vlcárcel ,Frncisco Jvier Ibáñez-López ,MríJosé López Montesinos
a University of Murcia,Murcia,Spain
b Biomedical Research Institute of Murcia (IMIB),Murcia,Spain
Keywords:Hospital Measurement Nursing administration research Workload
ABSTRACT Objectives: The study aimed to the multicenter application of a nursing workload measurement scale in the internal medicine and surgery adults hospitalization units.Methods:The study design was a multicenter,observational,and descriptive study.A multicenter application of the MIDENF® nursing workload measurement scale was carried out,which consists of 21 items,and covers the four nursing functions (patient care items,teaching,manager,and researcher),in units of hospitalization of adults of internal medicine and surgery of four different hospitals.Each item contains one or more of the nursing interventions of Nursing Interventions Classification (NIC) and has an assigned time,after comparing the real time it takes to perform each intervention with the North American Nursing Diagnosis Association (NANDA) standardized time.The study was carried out during nine months of the year 2020,measuring two days each month in the three work shifts (morning,evening,and night) to all patients admitted on the days of measurement in the indicated units.Results:The descriptive and inferential analysis of 11,756 completed scales,5,695 in general surgery and 6,061 in internal medicine,showed a greater care load for the two units during the morning shift(227,034 min in general surgery,261,835 min in internal medicine),especially in the items of“self-care”,“medication”,“common invasive procedures”,“fluid therapy”,and “patient and family support”,while the managerial function was similar during the three work shifts in the two units studied,getting values between 57,348 and 62,901 min.In the analysis by shift and unit,statistical significance was obtained both for the total workload and the four nursing functions(P <0.001).Conclusions:It is shown that the use of validated scales with the standardized language of nursing functions,adapted to the units,provides objective information to adjust the nursing staff to the real situation of care in any hospital and unit where it is applied,improving quality and patient safety.
What is known?
· Documentary workload measurement scales for intensive care and resuscitation units are known,and their adaptation to internal medicine and surgery hospitalization units is not possible,since these scales (Nine Equivalents of Nursing Manpower Use Score,Simplified Therapeutic Intervention Scoring System with 28 items,Nursing Activities Score,etc.) do not measure based on nursing functions (patient care,management,teaching,research) or the activities of adult units based on Nursing Interventions Classification (NIC).
What is new?
· This study that we present corresponds to the multicentric application,in the internal medicine and surgery adult hospitalization units of four different hospitals,of a scale previously designed and validated with mixed methodology,registered as MIDENF® and associated with a registration software and analysis of data.
· This scale is based on NIC interventions(standardized language of North American Nursing Diagnoses Association and internationally recognized) and covers the four nursing functions (patient care,management,teaching,and research).
1.Introduction
Nursing workload,according to existing literature,can be considered as the amount of time,physical and cognitive effort,assumed by professionals to perform direct and indirect care activities,and those not directly associated with the patient[1,2].This approach expands the concept of time dedicated to the demands of patients,since it also includes all the actions performed by the team during the process of caring and the time needed to execute the necessary interventions,not only in the care practice environment but also within the own professional development [1,3,4].
It is a complex phenomenon to measure,that is why it must be evaluated by objective,validated instruments and designed by the professionals themselves,taking also into consideration the care needs required by patients,those related to the management of the unit,the research and teaching development of healthcare professionals and taking into account the entire care system [1,5].
A nursing intervention refers to any treatment or care based on clinical judgment and knowledge that the nurse performs to enhance patient outcomes[4].Each intervention detailed a series of activities,which encompass the specific behaviors or actions developed by nurses to implement an intervention to help the patient to improve his/her health outcome [4,6].To standardize nursing language internationally,the Nursing Interventions Classification(NIC)was published.It describes specific behaviors of the act of caring and enables comparisons between the care practiced in different scenarios,and besides,it is regularly updated [4,6].
Identifying and measuring adequately the workload of nursing professionals is an important indicator to achieving efficient and effective management of human resources and establishing the amount of staff needed for proper health care,based on scientific evidence [7],as it constitutes the most significant staffing percentage in any healthcare organization[8].It also demonstrates the importance of balancing the amount of this stuff not only in quantitative but in qualitative terms,to provide quality health care[7,9],as a significant association has been demonstrated between workloads in hospitalization units and the average length of hospital stay,increased morbidity and mortality,and patient satisfaction.This confirms that increased workload has an impact on the quality of health care and patient safety,and therefore,adequate staffing to care demands,promotes safer care environments[10,11],as has also been demonstrated in recent months as a result of the COVID-19 pandemic [8].
Traditionally,nursing workload measurement scales have been designed for special units,such as ICU,where we find several validated scales:Nine Equivalents of Nursing Manpower Use Score(NEMS),Simplified Therapeutic Intervention Scoring System with 28 items (TISS-28),Nursing Activities Score (NAS),etc.,some even validated for different languages [12,13].But when it comes to Adult Hospitalization Units,we observe that the scales of ICU [14]or another type are used [15],not adapting to these internal medicines and surgery units,since they are not based on an internationally recognized standardized language (Nursing Interventions Classification [NIC]) nor in professional functions (patient care,management,teaching,and research).
The design and application of a workload measurement instrument,in addition to using standardized language and covering all nursing functions,as aforementioned,must be preceded by the validation of the instrument,which includes the vision of the healthcare professionals who will use it.A pilot test should also be performed in real-life conditions,before being approved for use,to ensure proper quality management and administration of care,resulting in improved satisfaction of the recipient of nursing care and patient safety [3,16].
The study we present corresponds to the multicenter application of a scale designed and validated with mixed methodology (qualitative and quantitative)for Adult Hospitalization Units,based on NIC interventions and that covers the four nursing functions,within a research Project financially supported by the Carlos III Health Institute (ISCIII) (AES-Spanish acronyms for Strategic Action in Health-2018 call),in relation to the Spanish National Plan for Scientific and Technical Research and Innovation 2017/2020,aimed at projects and initiatives in health services research,as a research priority in the challenge “Health,demographic change,and well-being” [17],and within the “Spanish Pluri-regional FEDER Operational Programme(POPE)2014-2020”(PI18/00950)with state funding[18].
The aforementioned scale has been registered under the name MIDENF® and is associated with software for data recording and analysis,designed and registered within the same project.The main objective of this study was to apply this scale in the internal medicine and surgery units of four hospitals with different circumstances,structures,patients,etc.to study not only the workload obtained in each unit and establish inferences but also to check how this recently created scale performs in different health institutions.
2.Methods
2.1.Study design
The study design was a multicenter,observational,and descriptive study.
2.2.Setting and participants
The characteristics of the four hospitals included in the study were: Hospital 1 (30 beds in internal medicine and 28 beds in surgery,for a staff of 13 nurses in each unit,distributed in three nurses for the morning shift,three for the evening and two at night),Hospital 2 (36 beds in each unit for a staff of 14 nurses in each unit distributed in four for the morning shift,three for the evening and two at night),Hospital 3 (30 beds with a staff of 12 nurses for each unit,distributed in three for the morning shift,three for the evening and two at night),and Hospital 4(34 beds in Surgery and 35 in internal medicine,for a staff of 13 nurses per unit,distributed in three for the morning shift,three for the evening and two at night),which resulted in a total of 131 beds for internal medicine and 128 beds for surgery,for a total of 104 participating healthcare professionals and their corresponding supervisors,constantly involved in the research project.The hours of each work shift were:morning from 8:00 a.m.to 3:00 p.m.,evening from 3:00 p.m.to 10:00 p.m.,and night from 10:00 p.m.to 8:00 a.m.
The inclusion criteria related to the patients whose interventions have been measured,and therefore,the workload associated with their care,were:patients admitted on the two days of measurement selected for each month in the hospitalization units of internal medicine and general surgery during the three work shifts measured (morning,evening and night) in four different participating hospitals.There were no exclusion criteria.The entire sample universe has been considered,that is,all the patients admitted to the selected units on the days of measurement,without excluding any.
2.3.Measure
The MIDENF® scale covers and is structured based on the functional dimensions of the nursing discipline (teaching,research,management,and patient care).The items were developed from a selection of(NIC)[6],adapting them to each of the aforementioned functional dimensions,and adapted to the tasks or activities arising from these interventions to be applied in Adult Hospitalization Units.
Besides,each item was assigned an execution time determined after a mapping between the real-time measured in current care conditions and the time standardized by the North American Nursing Diagnosis Association (NANDA),so that it would be as adjusted as possible to the current real-life situation.
The MIDENF®scale consists of 21 items,each item contains one or more NIC nursing interventions associated with the same application time.Each item has an assigned time,determined when designing the scale,after comparing the real time it takes to carry out each intervention with the standardized time of the NANDA.To measure workloads,the scale is applied to each patient in each work shift,noting the number of times each intervention/item is performed.The total time dedicated to that patient is calculated by adding the times resulting from each intervention performed.A nurse's care workload is calculated by adding the time spent on each of the patients she attends to during that work shift.To this time,the time allocated to the management of the unit,teaching,and research,during the same work shift,is added to determine the total workload of the nurse in the measured work shift.
The MIDENF® scale consists of 15 items for the patient care pattern:self-care(17 min),prevention(2 min),medication(9 min),samples (5 min),health education (3 min),nutrition (7 min),common invasive procedures (11 min),wounds (9 min),fluid therapy(22 min),care of devices (13 min),monitoring (2 min),airway(6 min),position (4 min),comfort (3 min),and patient and family support (8 min);four items for the management function (three items for the management related to the patient of 9 min each[which includes the care performed on admission and discharge from the unit]and one for the management of the unit,of 21 min),one item for teaching(16 min),and one item for research(20 min).In addition,it includes a separate set of items considered complementary,since they are usually performed in these units,although not as frequently as the previous ones: cardiac arrest (35 min),complex administrations (chemotherapy 18 min,blood products 10 min),transfers(60 min),occasional invasive procedures(9 min),isolation(11 min),behavior(50 min),interventions shared with the physician (27 min),and end-of-life care(38 min).
To complete it,the number of times each item is performed is recorded,and as they have a validated time assigned,we can calculate the total time spent by the nurse on that shift with that patient,therefore,a scale per patient and work shift was recorded for each day of measurement,plus the management time per patient and per unit,and the time allocated to teaching and research.
The recently created and validated scale [19],registered as MIDENF®,was used to carry out this study.In its validation,a Cronbach’s α coefficient of 0.727 was obtained,which is considered acceptable,the composite reliability was 0.685,Average Variance Extracted(AVE)of 0.099,and an Omega coefficient of 0.704,which would also be considered acceptable.Likewise,regarding construct validity,a KMO of 0.5 and a significant result in Bartlett’s Test were obtained,which dismisses that any variable caused multicollinearity and ensures the correct correlation of all variables.
2.4.Data collection
The study was developed in 2020,within a research project financially supported by the Carlos III Health Institute (ISCIII)(Spain),in its AES 2018 call,which began in 2018 with the design and validation of the MIDENF® scale.
The multicenter study was conducted during 9 months of the year 2020(only the months of March,April,and May were excluded due to the first waves of the COVID-19 pandemic,and the consequent health care collapse and state of confinement of the population).During the months of measurement,data were collected two days each month in the internal medicine and surgery units of four hospitals in the Region of Murcia.
The measurements consisted of applying the MIDENF® scale during each work shift(morning,evening,night),to all the patients admitted to these units,by the same nurses who cared for them.These measurements were recorded on a website with specifically designed software based on this scale,in which they were collected,stored,and could be analyzed subsequently.Therefore,the sample universe was considered,in other words,all the patients admitted on the days of measurement.
The person responsible for collecting the data is the corresponding author,and in addition,in each hospital,there were one or two people in charge of collecting and supervising the data collection (scales completed by the nursing staff working in the selected units),as well as include them in the software designed and created for this research project,where they were saved,classified and prepared for the statistical analysis carried out by one of the authors,who is a statistician at the University of Murcia.
2.5.Statistical analysis
The results of the multicenter study were subjected to a descriptive and inferential analysis using the R program version 4.0.3 (R Core Team 2020).
A total of 57 variables were analyzed.The independent variables“hospitalization unit” and “shift” were crossed with other variables:age,gender,length of stay per patient and medical specialty assigned to the patient,workload due to patient care,management,teaching and research activity,and the one corresponding to each of the items of the scale.
In turn,the independent variables “hospitalization unit” and“shift” were crossed with the dependent variables that allow calculating the time spent by nurses in those activities and tasks related to the selected NICs: self-care,preventive activities,medication administration,samples collection,health education activities,nutrition,invasive procedure activities,wound care,fluid therapy,care of devices,airway care,monitoring activities,patient comfort care,family support,cardiorespiratory arrest activities,chemotherapy,transfusions,transfers to other units,occasional procedures,patient isolation interventions,patient companionship,interventions shared with the physician,care of terminally ill patients,other management activities from the abovementioned(admissions,patient discharges,administrative requirements of the unit),and research and teaching activities.All these activities were analyzed in every single unit and shift.
Inferential analysis was carried out using a two-way ANOVA,but to do so the following assumptions had to be met: normality in each of the crosses of the two independent variables(unit and shift)and homoscedasticity of each of the independent variables mentioned in the descriptive analysis.If these assumptions were not met,the Welch AD test(robust ANOVA) would be used.
2.6.Ethical considerations
The corresponding permissions were requested from the Ethics Committees of the four participating hospitals,by their protocols.The study was approved by every hospital,maintaining confidentiality,as established in Law 15/1999,of 13 December,on the Protection of Personal Data(PDCP,Spanish acronyms),and the General Data Protection Regulation (GDPR),2016/679,of 27 April.It was also approved by the Ethics Committee of the Biomedical Research Institute of Murcia (IMIB-Arrixaca) on April 23,2018,registration number 04/2018.
3.Results
The results were obtained after a descriptive and inferential analysis performed on 11,756 completed observations/scales,5,695 in general surgery,and 6,061 in internal medicine,during 18 days of measurement in the eight participating units(total 144 days),in 54 work shifts for each unit(total 432 shifts).In Hospital 1,2518 scales were collected,3271 in Hospital 2,2485 scales in Hospital 3,and 3482 in Hospital 4.
In each work shift,3,976 scales were performed in the morning,3,879 in the evening,and 3,901 during the night shift.Regarding the socio-demographic variables,5,963 were performed on men and 5,793 on women,with a mean age of 68.61 years,a mean length of stay in the unit of 11 days,and although the patients were admitted to 34 different medical specialties,41.6% were from internal medicine and 22.1% from general surgery.
The workload per shift and according to the nursing function performed compared between the two study units was calculated in minutes based on the number of interventions/items performed in each shift on each patient and the associated execution time of each of them.We observed that the care load was higher than the rest,especially during the morning shift,resulting in a total of 261,835 min for internal medicine in the four hospitals,and 227,034 min for surgery (Table 1).About the workload of the management function,we can see that it is similar in the three work shifts and the two units,around 60,000 min in all the cases.Regarding the workload related to teaching and research,it is slightly higher during the morning shift,but also similar among the three shifts,ranging from 25,000 to 38,000 min per work shift(Table 1).
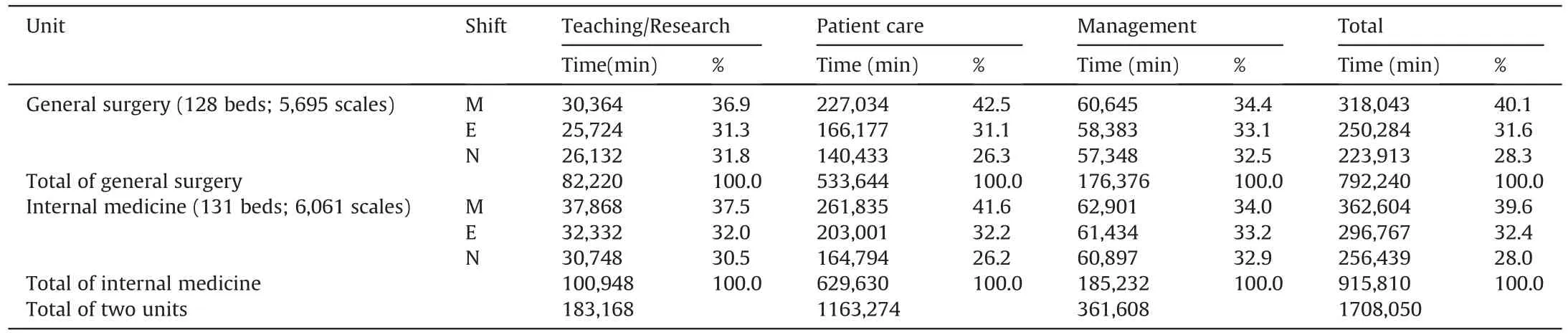
Table 1Descriptive time table for each type of workload from each unit and shift.
About the results according to the items of the scale,a heavier workload was obtained for all items during the morning shift,but greater for the items corresponding to the care function,those encompassing the NIC of “self-care”,“medication”,“common invasive procedures”,“fluid therapy” and “patient and family support” (Table 2).
Among the items included in the “supplements” or “occasional interventions” section,the items related to behavioral alterations and interventions shared with the physician stand out as those with the greatest workload,with a total time of 79,950 min for general surgery and 85,900 min for internal medicine,and 32,670 min for surgery and 34,425 min for internal medicine,respectively(Table 2).
Regarding the management function,the total time spent on“patient management” in surgery was 51,255 min and 54,594 min for internal medicine.For “unit management”,119,595 min were spent in surgery and 127,281 in internal medicine units,in both cases also greater during the morning shift (Table 2).
The total time spent in research was 56,060 min for surgery and 66,660 min for internal medicine,and for teaching,26,160 min in surgery,and 34,288 min in internal medicine units,in both cases higher during the morning shift (Table 2).
About the patient care workload,which is the nursing function with the greatest workload,if we compare it per unit and work shiftin the four hospitals participating in the study,we can observe that the greatest nursing workload occurred at Hospital 2 during the morning shift,120,671 min for surgery and 150,066 min for internal medicine (Table 3).
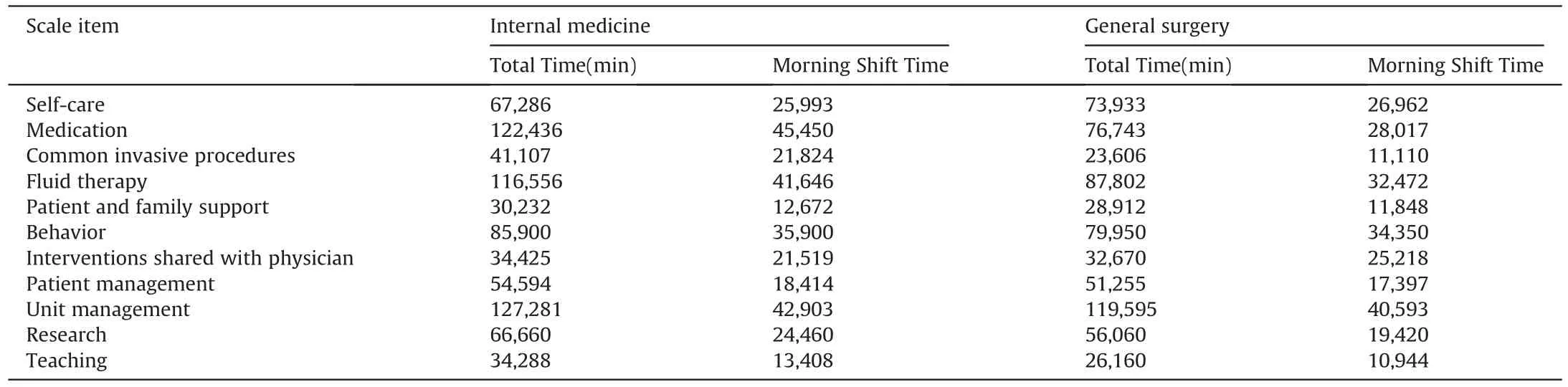
Table 2Scale items with the greatest workload in minutes in the four hospitals based on the hospitalization unit and the nursing function performed.
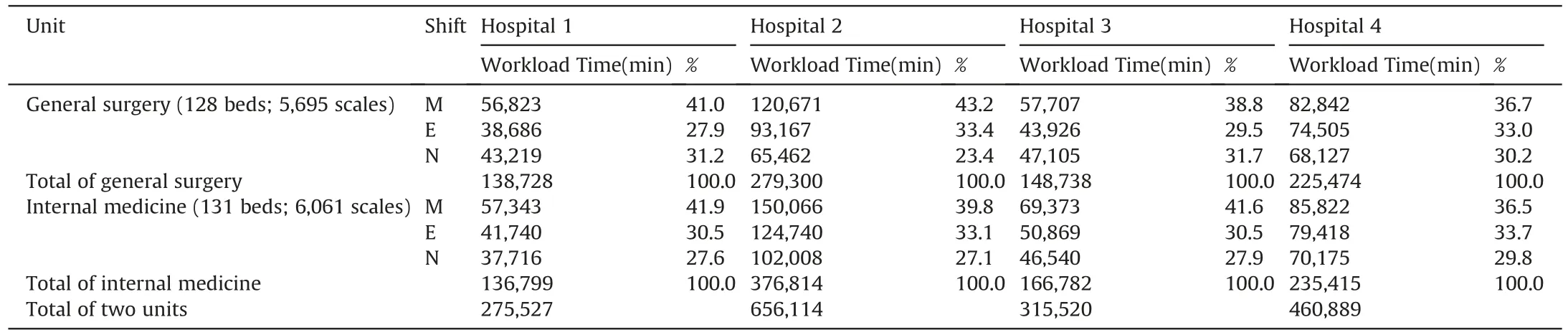
Table 3Patient care workload per hospital,unit and shift.
Referring to the additional inferential analysis performed on the data to find out statistically significant differences in the variables according to unit and shift,as well as their interaction,statistical significance was obtained about the shift in all except in the “prevention” item.For the unit,there is statistical significance in all except the items corresponding to “samples”,“comfort”,and “patient support”.The statistically significant differences regarding the interaction between unit and shift,through calculations of robust mixed models(P <0.001) were obtained in the items: “management workload”,“medication”,“samples”,“health education”,“invasive procedures”,“wounds”,“care of devices” and “monitorization”(Appendix A).The measurement of a real patient during the three work shifts in one day and the example of workload of a nurse who takes care of six patients in the morning shift were exposed(Appendix B,C).
4.Discussion
The measurement of workloads through validated scales covering all the functions of the nursing discipline and using a standardized language such as nursing interventions with NIC terminology has shown,through the present study and other studies[3,7,20]that use this type of interventions,that the hours of care spent to each patient can be established.At the same time,it can make visible the sizing of the team who works in the health units [1],which is beneficial since it reflects all the activities performed during each work shift,whatever type they are.
Other studies consulted that were carried out on patients in different medical specialties from those included in our study,have also used a selection of NIC interventions [21],and have grouped them into domains [4,7,20],as set out by NANDA,but we have found no studies that classify NIC interventions based on the four main functions of nursing as this study does.It collects all nursing activities,performed with more or less frequency in hospitalization units,with the application of the MIDENF®scale since,as reflected in other studies [3],nursing work is not limited to care activities,but there are other indirect care activities of collaboration with other healthcare professionals,students,etc.,that should be taken into account in the measurement instruments,assessing those that directly influence workload.
Other studies that have used NICs to measure workloads made a selection of interventions excluding personal activities,believing that they could hinder their comparison with other research[7]or they did not include family care or support [4].That is why the present study could be considered more complete,in the sense that it attempts to collect all the interventions or activities that a nurse could perform throughout her/his working day.But,at the same time,they agree with us that mapping the time measured in real conditions for the interventions used in the study,compared to the standard time assigned by NANDA [6],is significantly lower [3].
In studies that have used some interventions similar to those of our study,there are differences in the terms used to denominate them,for example,they highlight,as in ours,a greater time devoted to care activity,but they express it as a physiological domain [20],not as specific interventions.
In our study,if we compare the care activity per unit and work shift in the four participating hospitals,we can observe that the highest nursing care load occurred in Hospital 2 in the morning shift,120,671 min in surgery,and 150,066 min in internal medicine,especially if we compare it with Hospital 1,56,823 min in surgery and 57,343 min in internal medicine,being the two large reference hospitals.The 4 hospitals agree that the workload is slightly higher in the internal medicine department than in the surgery department.In general,the total workload of Hospitals 2 (656,114 min)and 4(460,889 min)is much higher than that recorded in Hospitals 1 (275,527 min) and 3 (315,520 min),with the same thing happening if we look at the results by units.The possible causes of these differences may be due to the different circumstances existing in each hospital,related to its structure,human resource management,etc.
In the case of activities related to management,which in our study account for 20%-30% of the total working day,we can see that it is similar in the three work shifts and the two units,around 60,000 min in all the cases,considering separately the management related to the patient and to the unit,when in other research they measure it only with the NIC intervention “Documentation”,which accounts for 15.8%[3],or 11.47%[20],while our item includes more activities related to management,not only documentation,although they do consider this intervention as one of the most relevant of those performed by nurses,in line to our results.
Another intervention highlighted in several studies is communication,as an element enhancing safe and effective practices for the patient and if interrupted,can hinder care and increase the time spent on this activity [22],but they consider it globally,including communication with other professionals,students teaching,telephone communication for patient or unit management and family support,accounting for 44% of the nurse's work time [3].
In our study,we have measured these different types of communication within their corresponding items of patient and family support,management,and interventions shared with the physician or teachings,and all these,as shown above in Table 2,were highlighted as those activities that require more nursing work time.
Other studies consulted [10] are in line with our research.Measuring the workload of nursing staff in clinical(such as internal medicine) and surgical (surgery) hospitalization units,allowed identifying the appropriate proportion of patients for each healthcare professional based on the real demands of care in the different work shifts.Significant differences between the workloads of clinical and surgical nurses [14] were found,in line with our view of the need for comparison between these units.As stated in the results,we found statistically significant differences in the four hospitals in almost all items by unit or work shift or according to the interaction between these variables.In our study,using a scale adapted to hospitalization units,for all interventions,the greatest workload was observed during the morning shift for the two specialties in the four hospitals,while we have found other publications that,using a scale designed for ICU(NAS),applied in hospitalization units,showed a higher workload during the evening shift [14].
The results obtained show that a nurse performs in her 7-h shift the work that she should do in more hours,if we adjust to the adequate time for its correct performance,assigned to each item/intervention,therefore it is shown that there is a high workload and that the staff is not adequate to the real needs of patient care(Appendix B,C).Many of the activities have to be done simultaneously and in less time than would be appropriate (the time allocated to each intervention or element)so that they have time to do them within their work shift.This is the reason why our research has been carried out,that is,to ensure that,through objective records such as our scale,the nursing staff adjusts to the real demands of patient care,improving the quality of care.
We would also like to highlight,independently some studies have attempted to measure workloads using electronic patient data[23] or hospital information systems [24],in our study we have designed,registered,and used specific software for the measurement of nursing workloads and its corresponding analysis,whereas other studies do not consider or propose as a future line of research[20].
5.Limitation
The limitations inherent to the health care activity influence data collection,such as the fact that many interventions are performed in a multitasking manner during the same time,as also reported in other studies [3],and the workloads to which the healthcare professionals were subjected during data collection may have influenced or hindered the correct recording of the data.
It should also be noted as a limitation that the multicenter study phase was carried out during the months of the COVID-19 pandemic throughout the year 2020.The Internal Medicine specialty(one of the study units)was one of the most affected for this reason as it suffered variations in terms of infrastructure and personnel to separate the usual patients of this unit,in which the data were collected,from the patients with COVID-19,admitted in other units not included in the study,with the emotional,physical and work-related burden this entailed for the nursing staff who participated in this study.
6.Conclusions
The results obtained in our research demonstrate the importance of the adequate distribution of personnel through the objective evaluation of nursing workloads using validated instruments,adapted to the units they are used in,with standardized terminology and that cover the interventions or activities performed by nurses in the four fields of functions they perform throughout their working day,and not only the care function or related to the patient's physiology,as the MIDENF®scale offers,to provide a safer attention and care environment of the highest quality.
The application of a validated scale for the measurement of workloads in Hospitalization Units,associated with the NIC,evinces an adaptation of its design to the real-life situation in which it will be used.This increases and corroborates the previously obtained validity of this scale.Moreover,it is accepted by healthcare professionals who,by seeing their work reflected in the instrument,can facilitate its applicability in practice.It can also satisfy their need to measure workloads so that staff can be adjusted to the real demands of care and confirm their commitment to the improvement of nursing management of human resources.
The workload associated with the real nursing interventions in Hospitalization Units,measured during the work shift,and calculated using times that have been confirmed and mapped with NANDA standards,and including all possible activities performed in these units,is presented as the most reliable indicator to determine the number of nursing staff required,considering the MIDENF®scale as a relevant management tool when balancing the number of staff.
The need among healthcare professionals to adjust nursing staff to the real demands of care with validated instruments and adjusted to the current nursing real-life situation is still valid today more than ever.Hence the number of studies that have addressed this issue in recent years,and many have incorporated the NIC terminology,to provide the management of nursing human resources with objectivity and adequate accuracy to the real-life nursing activity in any unit,but even more necessary in Adult Hospitalization Units,since they suppose a significant percentage of admissions in any health institution.
Therefore,our line of research will continue to try to incorporate or make this scale and/or its specifically designed software compatible with the different software used for patients’electronic clinical recording.It can thus be fed back by such records when filling in the different items,facilitating both its registration and interpretation,as well as the possibility to be used and applied in other health centers.And the management of nursing human resources in real-time in an objective manner and adjusted to the patients admitted at any given moment in the units become a daily reality in nursing work.
Funding
This research Project is financially supported by the Carlos III Health Institute(ISCIII)(AES-Spanish acronyms for Strategic Action in Health-2018 call),in relation to the Spanish National Plan for Scientific and Technical Research and Innovation 2017/2020,aimed at projects and initiatives in health services research,as a research priority in the challenge “Health,demographic change and wellbeing”(WHO,2014),and within the “Spanish Pluriregional FEDER Operational Programme (POPE) 2014-2020” (PI18/00950) (Pluriregional Operational Programmes,2018,Resolution of 28 December 2017,of the Director of the Carlos III Health Institute(ISCIII)).
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Credit authorship contribution statement
María Fuensanta Hellín Gil:Conceptualization,Methodology,Validation,Investigation,Data Curation,Writing -original draft,Writing -review &editing,Visualization,Supervision,Project administration,Funding acquisition.Marzena Mikla:Investigation,Data curation.Ana Myriam Seva Llor:Conceptualization,Methodology,Investigation.Maria Dolores Roldˊan Valcˊarcel:Conceptualization,Methodology,Investigation,Data curation.Francisco Javier Ibˊa˜nez-Lˊopez:Formal analysis,Writing -original Draft,Writing -review &editing.María Josˊe Lˊopez Montesinos:Conceptualization,Methodology,Validation,Investigation,Writing-original Draft,Writing -review &editing,Supervision.
Declaration of competing interest
The authors have declared no conflict of interest.
Acknowledgments
We would like to thank all the people and institutions that have collaborated with this project:the Carlos III Health Institute(ISCIII),IMIB/FFIS for the financial support and management of the project,the Statistical Support Section (SAE in its Spanish acronyms),Scientific and Research Area(ACTI in its Spanish acronyms),University of Murcia (www.um.es/web/acti) for their statistical analysis,and the IMIB bioinformatics platform for the data collection software.
To the four participating hospitals for allowing to carry out this research project in their centers (H.C.U.V.Arrixaca,H.G.U.Reina Sofía,H.G.U.Santa Lucia and H.G.U.Los Arcos del Mar Menor),to all the nursing staff and experts who participated in the different methodological phases of the validation,as well as to the supervisors of the units under study,and to the Quality Area Supervisors of the Santa Lucia and Los Arcos del Mar Menor Hospitals.
Appendices.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2022.09.011.
杂志排行
International Journal of Nursing Sciences的其它文章
- Effects of equine-assisted interventions on older adults’ health: A systematic review
- Quality indicators for the care of older adults with disabilities in longterm care facilities based on Maslow’s hierarchy of needs
- Exploring social movement concepts and actions in a knowledge uptake and sustainability context: A concept analysis
- Palliative care needs and symptom burden in younger and older patients with end-stage renal disease undergoing maintenance hemodialysis: A cross-sectional study
- Lived experiences with unmet supportive care needs in pediatric cancer: Perspective of Chinese children and their parents
- Development and validation of a nomogram for predicting the risk of pressure injury in adult patients undergoing abdominal surgery
